Radiation therapy is well known to cause both acute and chronic changes in irradiated skin. Isolated cases of immediate xanthomatous changes following radiotherapy or chemotherapy have been described in association with certain tumors and with inflammatory disorders such as herpes zoster infection and mosquito bites.
We present the case of an 83-year-old woman with a history of diabetes mellitus, dyslipidemia, chronic kidney failure, Parkinson disease, and left breast cancer treated with breast-conserving surgery with axillary lymph node dissection, radiotherapy, and chemotherapy in 2008. The patient was referred to our department for assessment of an asymptomatic yellowish plaque of 6 months’ duration on the left breast. The physical examination showed a large yellow-brown plaque that was slightly hard to the touch and had a verrucous, papilliform surface surrounded by an erythematous halo. The plaque had well-delimited borders and a peculiar geometric shape. There was no evidence of inflammation or local infection (Fig. 1). No other relevant findings were observed in the examination.
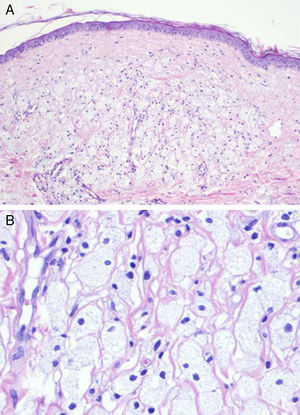
A skin biopsy was performed to investigate the suspected diagnoses of tumor recurrence, xanthogranulomatous mastitis, and radiation-induced xanthomatous changes. The histopathologic findings showed a thinned epidermis with flattened rete ridges, an infiltrate consisting of numerous clusters of foamy histiocytes interspersed with inflammatory cells in the superficial dermis, and discrete inflammatory interstitial infiltrates in the deep dermis (Fig. 2). There were no signs suggestive of malignancy. The xanthoma-like cells were positive for CD68 and negative for cytokeratins in the immunohistochemical study. Results of a complete blood count, chest radiograph, and abdominal ultrasound were unremarkable.
A diagnosis of delayed xanthomatous pseudotumor secondary to chemotherapy and radiotherapy was established.
The general criteria for diagnosing radiation-induced tumors include histologic confirmation of a tumor in the irradiated area, a period of latency between exposure to radiation and development of the tumor, and exclusion of a tumor before radiotherapy.1
Few cases of xanthomatous transformation have been reported in patients with tumors treated by radiotherapy and/or chemotherapy, and most have involved B-cell lymphomas (Table 1).1–9
Summary of Cases of Xanthomatous Transformation of a Tumor Following Radiotherapy and/or Chemotherapy.
| Type of Tumor | Treatment | Latency Period | |
|---|---|---|---|
| Sasaki et al. (1983)2 | Malignant pleomorphic fibrous histiocytoma | Radiotherapy | 3 wk |
| Ashfaq et al. (1992)3 | Abdominal Burkitt lymphoma | Polychemotherapy | 4 mo |
| Ijiri et al. (2000)1 | Ependymoma | Radiotherapy+chemotherapy | 8 y |
| Chung et al. (2003)4 | Primary cutaneous CD30+ large T-cell lymphoma | Radiotherapy | 5 wk |
| Tan et al. (2003)5 | High-grade invasive ductal carcinoma | Chemotherapy | Immediate, on completion of chemotherapy |
| Chumsri et al. (2007)6 | Hodgkin lymphoma | Radiotherapy+polychemotherapy | Immediate, on completion of treatment |
| Chandra et al. (2009)7 | Two cases of diffuse large B-cell lymphoma | Polychemotherapy | 1 and 3 mo |
| Otto et al. (2012)8 | Diffuse large B-cell lymphoma | Polychemotherapy | 3 mo |
| Turrión-Merino et al. (2016)9 | Primary cutaneous CD30+ anaplastic large T-cell lymphoma | Radiotherapy+methotrexate | Immediate, on completion of methotrexate therapy |
These inflammatory pseudotumors are an enigmatic entity and appear to be due to a localized inflammatory process mediated by inadequate production of cytokines. Several terms have been proposed to describe formations of xanthomatous cells that appear after radiotherapy and/or chemotherapy, including postchemotherapy histiocyte-rich pseudotumor, xanthomatous pseudotumor, and benign histiocytic proliferation with xanthomatous changes.2,5,7,9,10
Despite the few cases published, it has been hypothesized that these xanthomatous cells may be histiocytes that survived the chemotherapy or radiotherapy or histiocytes from peripheral blood that engulf necrotic fat debris released by destroyed tumor cells and become xanthomatous cells.1,3–5,7,9 It is plausible that chemotactic substances released in response to the tumor necrosis trigger the recruitment of monocytes, which then differentiate into histiocytes. These, in turn, would be activated, increase in size, and trigger the release of more chemokines, leading to the recruitment of additional monocytes and a considerable accumulation of histiocytes in response to the tumor necrosis.7 This process does not appear to be related to high cholesterol or triglyceride levels. Rather, it seems to be an unpredictable treatment sequela related to phagocytosis of necrotic cell debris.3
These collections of xanthomatous cells can form large pseudotumors and polypoid lesions that can mimic neoplastic disease, and their recognition is essential from the perspective of patient management.3 The transformation generally occurs within the first few weeks or months of treatment. In our case, the xanthomatous pseudotumor appeared 7 years after the patient was treated with radiotherapy and chemotherapy. There is just 1 other report in the literature of a similarly long latency period: that of a xanthomatous meningioma that developed 8 years after radiotherapy.1
In our patient, the site of the lesion (clearly located in the irradiation field) and its characteristics (clearly demarcated borders) suggest that radiotherapy may have been the main factor responsible for the xanthomatous transformation.
We have reported the first case of a xanthomatous pseudotumor following the treatment of breast cancer with radiotherapy and chemotherapy. The long latency period between the treatment and the appearance of the changes is particularly noteworthy.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: González-Sabín M, Mallo-García S, Rodríguez-Díaz E, Gonzalvo-Rodríguez P. Seudotumor xantomatoso diferido tras tratamiento de cáncer de mama. Actas Dermosifiliogr. 2017;108:484–486.