A healthy 57-year-old man presented with a ulcerated lesion in the right parietal region that had first appeared 30 years earlier and had grown slowly and progressively, as well as an asymptomatic ipsilateral nodule in the retroauricular region that had first appeared 20 years earlier.
Physical ExaminationPhysical examination revealed a hard, well-defined, lobulated, ulcerated lesion measuring 10cm×8cm in the right parietal region. A skin-colored nodule of elastic consistency, not adherent to the deeper tissues, was observed in the ipsilateral retroauricular region (Fig. 1).
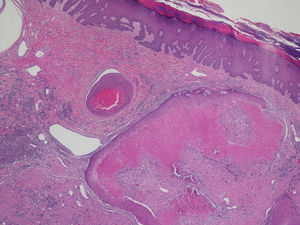
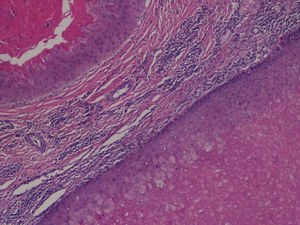
HistopathologyIn both the initial biopsy and the complete excision of the lesion, specimens were obtained for hematoxylin-eosin staining. Both specimens showed a well-defined, unencapsulated cystic tumor formed by several different-sized lobules composed of an external layer of basaloid cells and several layers of eosinophilic spindle cells with abrupt keratinization (Fig. 2). No atypia or mitotic figures were observed at higher magnification (Fig. 3).
Additional TestsFine-needle aspiration of the retroauricular nodule revealed reactive lymphadenitis without evidence of tumor cells.
What Is Your Diagnosis?
DiagnosisProliferating trichilemmal tumor (PTT).
Clinical Course and TreatmentThe lesion was completely excised with safety margins of 1cm and no evidence of recurrence has been observed after 2 years of follow-up.
CommentPTT is a rare malignancy derived from the follicular outer root sheath that was first described in 1966 by Wilson-Jones.1 PTT is more common in women over 60 years of age. The lesions are located on the scalp in 90% of cases, but other sites have also been reported. PTT can appear at the site of a preexisting trichilemmal cyst or arise de novo.
Clinically, PTT presents as a slow-growing tumor of variable size—from <1cm to 25cm—although in some cases the lesion can be fast-growing, which can indicate malignancy. In many cases, the lesion has a lobulated appearance, gradually becomes ulcerated, and can secrete a whitish, foul-smelling material.2
Histologically, PTT is a lobulated tumor consisting of a basement membrane that delimits the lesion, a layer of palisading basaloid cells, and a squamous epithelium with an area of abrupt keratinization, giving rise to cystic cavities that contain a homogeneous eosinophilic material that can show foci of calcification in 25% of cases. Dyskeratosis, mitotic figures, and cells with low-grade nuclear atypia are observed in some cases.
Although the lesions can have an aggressive histologic appearance, the behavior of PTT is benign in most cases. However, there is a malignant variant that can cause lymph node or distant metastases in 30% of cases and is associated with high mortality.
Factors associated with a risk of malignant transformation include non-scalp location, history of rapid growth, size >5cm, infiltrative growth pattern, and the presence of marked cytologic atypia with abundant mitotic figures.3
Immunohistochemistry and flow cytometry can sometimes be useful to predict the behavior of these tumors, as it has been observed that some malignant PTTs have a higher rate of cell proliferation, decreased CD34 expression, and DNA aneuploidy, although the diagnosis should be based mainly on histologic findings.4
The differential diagnosis includes epidermoid carcinomas, epidermoid cysts, sweat gland tumors, dermatofibrosarcoma protuberans, pilomatrixomas, and angiosarcomas.5
Treatment consists of surgical excision with safety margins of 1cm (deep to the galea aponeurotica) or Mohs surgery because PTT is a tumor with a high rate of recurrence, despite its benign behavior.2,6
We have reported this case because PTT is a rare tumor that can have a very alarming clinical appearance, although histologic examination and clinical follow-up show it to be benign.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Hermosa-Gelbard A, Moreno García del Real C, Vañó-Galván S. Tumoración en cuero cabelludo de gran tamaño de larga evolución con adenopatías ipsilaterales. Actas Dermosifiliogr. 2018;109:63–64.