The patient was a 53-year-old male with a history of hypertension, for which he was being treated with enalapril. He attended our clinic because of multiple, scaly, slightly itchy papules on the palmar surfaces and sides of the hands and fingers. These lesions had appeared 2 to 3 years earlier and had remained stable without treatment. During this period the patient's fingernails, particularly that of the left thumb, became fragile and striated.
Physical ExaminationOn the sides of the fingers and the thenar eminences of both hands the patient had multiple skin-colored papules of 1-2mm in size with slightly scaly, keratotic surfaces (Fig. 1). Longitudinal striations were observed on the fingernails of both hands, and pterygium of the nail on the left thumb (Fig. 2). No lesions were detected in the mucosa or in any other locations.
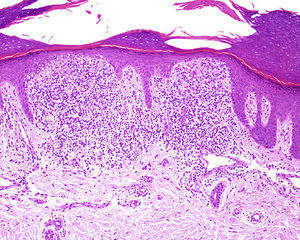
HistologyBiopsy showed a well-circumscribed, dense, subepidermal lymphohistiocytic infiltrate occupying 4 dermal papillae. The infiltrate extended to the epidermal basement membrane, which showed vacuolar degeneration with some apoptotic keratinocytes. The epidermis was thinned and showed parakeratosis (Fig. 3).
Additional TestsFungal culture of nail scrapings was negative.
What Is Your Diagnosis?
DiagnosisPalmar lichen nitidus with nail involvement.
Clinical Course and TreatmentThe patient was treated with topical clobetasol for 2 months with no improvement of the lesions.
DiscussionLichen nitidus (LN) is a chronic inflammatory disease of unknown etiology that predominantly affects children and young adults. It is characterized by the presence of numerous skin-colored papules of a few millimeters in size. These are widely distributed but predominantly present on the genitals, abdomen, chest, and the flexor surfaces of the extremities. Most cases involve few symptoms and resolve spontaneously.1 LN with involvement of the palms, soles of the feet, nails, and mucous membranes is uncommon.2 There are several clinical variants of LN, including keratotic, vesicular, purpuric, perforating, and generalized forms.1,3 LN can be associated with lichen planus in up to 30% of cases, suggesting that these 2 conditions may be different manifestations of the same process, rather than independent entities. Histologically, LN is characterized by the presence of clusters of lymphocytes and epithelioid histiocytes, sometimes accompanied by multinucleated giant cells, occupying between 1 and 5 dermal papillae and making close contact with the epidermal basal layer, which shows vacuolar degeneration and colloid bodies. The epidermis is thinned and exhibits parakeratosis. The inflammatory infiltrate is surrounded by elongated epidermal ridges.
LN localized exclusively on the palmar surfaces is relatively uncommon, and affects comparatively older patients (age range, 37-52 years) than other forms of LN. It can present as punctate papules, keratotic spicules, or diffuse palmar hyperkeratosis with flaking and fissuring.2,4,5 The differential diagnosis of palmar LN should include psoriasis, chronic eczema, and dyshidrotic eczema. Microscopy of palmar LN generally reveals typical LN features, although in some cases the inflammatory infiltrate forms a more diffuse band in the superficial dermis. Palmar LN tends to show a chronic course and can be refractory to treatment.
Nail involvement is observed in less than 10% of LN cases and is often associated with palmar involvement.1 The associated lesions (onychorrhexis, splitting of the distal nail plate, and irregular depressions) are similar to those caused by lichen planus.5
We have presented a case of LN with exclusive palmar involvement. The nail alterations of our patient could be secondary to LN or to the expression of lichen planus which had so far failed to develop in other locations.
Please cite this article as: Córdoba S, Tardío J, Borbujo J. Lesiones queratósicas en las palmas de las manos y alteraciones ungueales. Actas Dermosifiliogr. 2015;106:133–134.