Janeway lesions were first described by Edward Janeway in 1899 in patients with infective endocarditis.1 At present they are part of the minor diagnostic criteria (modified Duke criteria) for the disease together with other cutaneous manifestations such as Osler nodes.1–3 However, in recent decades, cases of Janeway-like lesions have been described in connection with other infectious diseases.
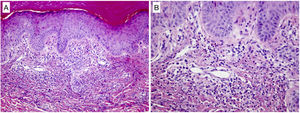
A 69-year-old man complained of fever and shivering lasting 24h with no other signs or symptoms but general deterioration of his health. The physical examination showed tachypnea, impaired consciousness (Glasgow Coma Scale score, 12), and low blood pressure (90/60mmHg). Additional tests ordered in the emergency department revealed leukocytosis with neutrophilia, elevated procalcitonin levels, electrolyte imbalance, and metabolic acidosis. Transthoracic echocardiography did not detect vegetation. The patient was admitted to the intensive care unit with a clinical diagnosis of sepsis of unknown focus (3 points on the quick Sequential Organ Failure Assessment (qSOFA) scale, and empirical antibiotic treatment was prescribed. Subsequently, we requested evaluation due to the appearance of painless skin lesions on the palms. Cutaneous examination revealed millimetric erythematous-violaceous macules with an annular pattern on both hypothenar eminences (Fig. 1A and B), as well as a bleeding longitudinal lesion on the nail of the third finger of the right hand consistent with a splinter hemorrhage. The patient had no plantar involvement. A skin biopsy revealed an inflammatory infiltrate of predominantly polymorphonuclear neutrophils in the papillary dermis forming a microabscess without vasculitis or fibrin emboli (Fig. 2A and B). The epidermis and the glomus presented no abnormalities. The Gram stain was negative. These histologic findings supported the diagnosis of Janeway lesions.
Histologic findings of a biopsied lesion showed dermal but no epidermal abnormalities. (A) Superficial dermal neutrophilic focal infiltration forming poorly defined microabscesses with no signs of vasculitis (hematoxylin–eosin, original magnification ×100). (B) Further enlargement (original magnification ×200) confirmed the absence of vasculitis and also identified mild karyorrhexis and isolated eosinophils.
The culture of 1 of the lesions and blood cultures were negative. Serial transthoracic and transesophageal echocardiography ruled out the presence of endocarditis, and an ophthalmologic examination showed no abnormalities. Laboratory tests showed progressive deterioration of kidney function (creatinine 3.2mg/dL) and the ratio of PaO2 to the inspired oxygen fraction (<300mmHg). Computed axial tomography later revealed an infectious pulmonary focus, and, following bronchoscopy, Enterobacter asburiae and Klebsiella pneumoniae were isolated in the bronchoalveolar lavage.
Based on clinical and histologic findings and additional test results, we established a final diagnosis of sepsis of respiratory origin (qSOFA, 4 points) with associated Janeway-like lesions. The skin lesions resolved in a few days, but the patient developed multiple complications and died 4 months after admission.
Janeway lesions, together with Osler nodes, constitute the main skin manifestation of infective endocarditis.1,2 Traditionally, Osler nodes have been associated with subacute cases and Janeway lesions with acute cases of endocarditis.1,3 Their prevalence ranges from 5% to 15% in infective endocarditis, although this figure may be an underestimation.3 The exact pathogenesis of skin lesions associated with infective endocarditis is still debated.1,4,5 Clinically, Janeway lesions are characterized by small, painless erythematous macules and are located on the palms and soles. They may last from days to weeks and disappear leaving no residual lesions.1,3–6 Classic histologic findings include the presence of dermal microabscesses with no signs of vasculitis, although recent publications argue that diverse histologic patterns are possible.1,3,6Microbiology cultures are not always positive. While such lesions were initially described in connection with infective endocarditis, their presence is not limited to this disease alone. In recent years, cases of Janeway-like lesions have been reported in staphylococcus septicemia (2 cases) and following endovascular procedures (2 cases) (Table 1).7–10 Infective endocarditis was reasonably ruled out in all those cases. Our report of these lesions in a patient with a non-staphylococcus respiratory infection can be included in this group of Janeway-like lesions not associated with infective endocarditis.
Cases of Janeway-Like Lesions With No Signs of Endocarditis.
| Clinical manifestations | Skin biopsy | Microbiologic studies | Additional tests | Final diagnosis | |
|---|---|---|---|---|---|
| Reddy et al. (2013) | Erythematous macules, papules, and vesicles on palms and soles.Fever, dyspnea, and productive cough. | Epidermal necrosis, neutrophilic abscess in reticular dermis with the presence of gram-positive coccobacilli in the center. No signs of vasculitis. | Staphylococcus aureus resistant to methicillin in sputum, blood, and skin cultures | Chest X-ray: bilateral lower lobe consolidations. Transthoracic and transesophageal echocardiography negative. | Janeway-like lesions secondary to staphylococcal septicemia |
| Yamamoto et al. (2014) | Painless reddish-blue spots on palms and soles, subconjunctival bleeding, and erythema with scaling on the scalp and limbs.General malaise and fever. | No | S aureus sensitive to methicillin in blood cultures | No | Staphylococcal septicemia secondary to psoriatic erythroderma with associated Janeway-like lesions |
| Mathes et al. (2016) | Multiple erythematous macules and papules on the right hand upon removal of the right radial arterial catheter inserted for blood pressure monitoring.No systemic symptoms. | No | Skin culture: S aureus sensitive to methicillin | Ultrasound: pseudoaneurysm of the radial artery with extravasation. | Janeway-like lesions secondary to infected radial aneurysm |
| Hernández-Ramírez et al. (2017) | Janeway-like lesions on the sole of the left foot 1 month after bypass of the left femoral vessels during heart surgery for extracorporeal membrane oxygenation.Fever. | No | Blood and skin cultures: Pseudomonas aeruginosa | Transesophageal and transthoracic echocardiography: no signs of endocarditis.Computed tomography: pseudoaneurysm of the left femoral artery. | Localized Janeway-like lesions following extracorporeal membrane oxygenation |
| Our case (2021) | Erythematous-violaceous annular macules on hypothenar eminences, bleeding longitudinal on the third finger of the right hand. No plantar involvement.General malaise, fever, and shivering. | Polymorphonuclear neutrophils forming a microabscess in the papillary dermis. No signs of vasculitis or fibrin emboli. Epidermis and glomus with no abnormalities. | Blood and skin cultures: negative.Culture of bronchoalveolar lavage fluid: Enterobacter asburiae, Klebsiella pneumoniae. | Transthoracic and transesophageal echocardiography: no signs of endocarditisComputed tomography: lung infection.Ophthalmologic study: no abnormalities. | Janeway-like lesions secondary to a respiratory infection |
We present the first case described to date of Janeway-like lesions secondary to a respiratory infection. When such lesions are observed, we think it important to consider possible infectious causes other than infective endocarditis and to investigate a possible history of a recent endovascular procedure.
Conflicts of InterestThe authors declare that they have no conflicts of interest.