A 33-year-old healthy female, nurse, Fitzpatrick phototype IV, presented with a history of a piercing proceeded on the left nasal ala in 2019. She referred multiple local traumas in daily activities, such as accidental adhesion of the piercing to clothes or bath towel. In January 2021, a papule appeared on the same nasal region. The patient repeatedly tried to remove the lesion with a small needle, resulting in local bleeding and progressive growth to a tumor. No other lesions or constitutional symptoms have been described.
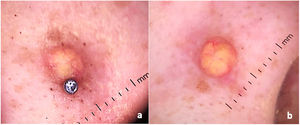
Dermatological examination revealed small erythematous-brownish nodule, 1.5cm diameter, similar to a keloid adjacent to the nasal piercing (Fig. 1). No other injuries have been identified. Dermoscopic analysis indicated a yellow-orange central area surrounded by peripheral erythematous border with fine linear telangiectasias, suggestive of xanthogranuloma (Fig. 2a and b).
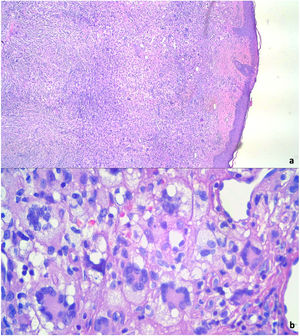
We proceeded the complete excision of the tumor. Histopathological study identified a nodular dermal proliferation with xanthomized histiocytes, foreign body-type multinucleated giant cells and Touton multinucleated cells, along with scattered lymphocytes, plasma cells and eosinophils (Fig. 3a and b). Immunohistochemistry appointed positive stains for CD68. S100 and CD1a were absent. BRAF-V600E mutations analysis through real-time polymerase chain reaction (PCR) was negative. Laboratory investigation revealed no abnormalities in routine blood examination parameters, triglyceride levels, liver function or renal function. The tests confirmed the diagnosis of adult xanthogranuloma, and there was clinical improvement after surgical removal. The patient maintains dermatological follow-up with no injury recurrence.
Xanthogranuloma is the most common non-Langerhans cell histiocytosis.1 It is a benign proliferative disorder, usually described in early childhood as juvenile xanthogranuloma (JXG). Almost 85% of cases of JXG occur in infants less than one year of age, with a male preponderance.1 Late-onset lesions in adults is infrequent and represents 10% of all xantogranulomas.1 Most reports describe adult xanthogranuloma between the third and fourth decades of life, with equal sex distribution.2 The pathogenesis is unknown, and the most associated triggers are infections or physical factors,3 with few studies in the world literature describing trauma-induced xanthogranuloma. The patient described in this report presented an unusual onset of adult xanthogranuloma after recurrent local traumas.
The lesion typically manifests as a reddish or yellowish to brown solitary papulonodule on the head, neck, limbs, and upper trunk.4 Nasal involvement is even rarer and only three cases on this specific topography have been published.5–7 Tan et al. (2014) also reported an unusual presentation of adult xanthogranuloma on the left nasal ala, as we describe herein. However, unlike our case, no trigger factor has been identified.5 A few articles documented multiple lesions and extracutaneous and systemic involvement.2,4,8 Dermoscopic evaluation is a powerful tool to define diagnostic hypothesis, revealing the characteristic yellow-orange central area surrounded by a peripheral erythematous border with fine linear telangiectasias.1 Differential diagnosis includes dermatofibroma, Langerhans cell histiocytosis, other xanthomatous lesions, mastocytoma, and Spitz nevus.
Diagnostic confirmation is made through skin biopsy. Histopathological analysis identifies dense dermal histiocyte infiltrate and Touton giant cells, which are multinucleated cells, with homogeneous eosinophilic cytoplasmic center and peripheral xanthomatization.3 Immunohistochemistry is also important to define diagnosis and shows positive stains for Factor XIIIa, CD68, CD163, CD14, and fascin. Stains for S100 and CD1a, specific for Langerhans cells, are negative.9 In cases with atypical histology features or immunohistochemistry suggestive of xanthogranuloma and Langerhans cell histiocytosis (LCH), the investigation of BRAF-V600E mutations is recommended. BRAF-V600E mutations have been described in LCH and can identify LCH coexisting with xanthogranuloma.10 In this case report, this oncogenic mutation was absent, reaffirming the xanthogranulomatous nature of the tumor.
Usually, no laboratory abnormalities are identified in patients with solitary AXG. However, clinicians should be aware of systemic involvement and hematological malignancies in adults with multiple xantogranulomas.8 In these cases, laboratory and imaging investigation are essential. AXG generally follows a benign course, with spontaneous regression in approximately 3–6 years.1 Surgical excision, CO2 laser, and intralesional steroids can be performed, mainly for cosmetic reasons.3
In this report, the patient's history and clinical examination suggested a keloid lesion. However, dermoscopic analysis revealed typical findings of xanthogranuloma and guided our Dermatology team to an accurate diagnosis. In conclusion, the correct use of the dermatoscope is effective not only to evaluate melanocytic lesions, but also to non-melanocytic, as in the present case. Dermatologists should use this tool daily in every physical examination to improve diagnostic accuracy. After directing the diagnostic hypothesis, the confirmation was established through histopathology and immunohistochemistry, which were also compatible with adult xanthogranuloma.
Conflict of interestsThe authors declare that they have no conflict of interest.