To analyze trends in the prevalence of contact sensitization to p-phenylenediamine between 2004 and 2014, taking into consideration that the concentration of this product in cosmetics was regulated in 2009. To explore risk factors for contact allergy to p-phenylenediamine.
Materials and methodsRetrospective observational study of patients suspected of having contact dermatitis from allergy to p-phenylenediamine during the years between 2004 and 2015 in 8 tertiary level hospitals. The patients underwent patch testing (TRUE-test) with the standard series of the Spanish Research Group on Contact Dermatitis and Skin Allergies. This series included p-phenylenediamine 1%. We followed international recommendations for the statistical analysis of data related to contact allergies.
ResultsThree hundred eighty-six out of 9341 patients (4.1%) had positive reactions to p-phenylenediamine. The prevalence tended to decrease in the early years (2004–2007) and then leveled off at around 4%. Risk factors for developing contact dermatitis from p-phenylenediamine were sex, age over 40 years, multiple sensitivities, and profession, notably workers in hair salons and those who handle rubber and plastics.
ConclusionsThe prevalence of p-phenylenediamine allergy remains high among patients with contact eczema. Risk factors for p-phenylenediamine contact allergy are consistent with previous reports.
El objetivo del trabajo es mostrar la tendencia de la sensibilización de contacto entre los años 2004-2014 tras la regulación de su concentración en cosméticos en el año 2009 e investigar los factores de riesgo de la alergia de contacto a la parafenilendiamina.
Material y métodosEl diseño del estudio fue observacional retrospectivo incluyendo pacientes con sospecha de alergia de contacto parcheados con la serie estándar del Grupo Español de Investigación en Dermatitis de Contacto y Alergia Cutánea durante los años 2004 al 2014, en 8 hospitales terciarios españoles.
En las pruebas epicutáneas estaba incluida la parafenilendiamina al 1% en vas. ó 0.073 mg/cm2 en el TRUE-test®. El estudio estadístico se realizó siguiendo las recomendaciones internacionales del análisis de los datos en alergia de contacto.
Resultados386 (4,1%) pacientes de los 9341 incluidos fueron positivos a la PPD, cuya tendencia empezó a decrecer en los primeros años (2004-2007) y a partir de ahí se mantuvo en torno al 4%. Los factores de riesgo para el desarrollo de una alergia de contacto a la PPD fueron el sexo, la edad por encima de los 40 años, la polisensibilización y la profesión, entre las que destacan los trabajadores de la peluquería, los trabajadores de la goma y el plástico
ConclusionesLa alergia de contacto a la PPD sigue siendo elevada en pacientes con eccema de conatcto. Los factores de riesgo que predisponen a la alergia de contacto a la PPD coinciden con los que han sido publicados previamente.
p-Phenylenediamine (PPD) is an aromatic amine found in textile, leather and hair dyes and in henna preparations for temporary tattooing. The rate of PPD allergy detected in patients undergoing patch testing for suspected contact eczema ranges from 3% to 5%.1,2 A rate of 7% was reported in the United States,3 but the prevalence was lower in a European general population study.4 PPD is not included in the standard series of allergens used in many central European countries because of risk of active sensitization. Since the concentration of PPD in cosmetics was regulated in 2009, trends in contact sensitization in Spain have not been studied.5 This study aimed to analyze variations in the frequency of contact sensitization to PPD between 2004 and 2014 and to explore risk factors for this allergy.
Material and MethodsThis retrospective observational study analyzed records for patients suspected of having contact allergy who underwent patch testing with the standard series of the Spanish Research Group on Contact Dermatitis and Skin Allergies between 2004 and 2014. Eight tertiary level hospitals with departments specializing in such allergies participated. The hospitals were located in different areas across Spain.
The patch tests were carried out following the guidelines of the European Society of Contact Dermatitis.6 The Spanish series included PPD in petrolatum (1%, or 0.073 mg/cm2) in a TRUE-test panel. The reactions were assessed using an internationally applied scale, where + indicates light nonvesicular erythema, ++ notable papule formation with discrete vesicles, and +++ strong vesiculation and blistering. Evaluations were made and classified at 48, 96, and 120 hours. Workplace exposure was considered relevant to a PPD reaction if clinical features and professional exposure were consistent with that classification. Exposure might be past, current, or unknown depending on clinical features and location. A patient was considered polysensitized if 3 or more reactions to unrelated substances in the standard series were observed.
Patient data were entered anonymously into Winalldat software as previously described.7
We followed international recommendations for the statistical analysis of data related to contact allergies.8 Descriptive statistics were calculated for the main sociodemographic and clinical variables, the initial locations of lesions, and the MOAHLFA index components (male sex, occupation, atopy, hand involvement, leg involvement, facial involvement, age). We used the χ2 test to compare differences between patients with and without PPD sensitization. Frequencies and percentages of PPD sensitization were recorded for each year of the study, and trends in the percentages were analyzed with the χ2 test. We also analyzed percentages of positive reactions to PPD according to workplace relevance, intensity and sex, calculating 95% CIs for the proportions. Finally, logistic regression was used to identify risk factors for PPD allergy. Statistical significance was set at P < .05. All statistical analyses were done with STATA software. The study design was approved by the ethics committee of Hospital Universitario de la Princesa.
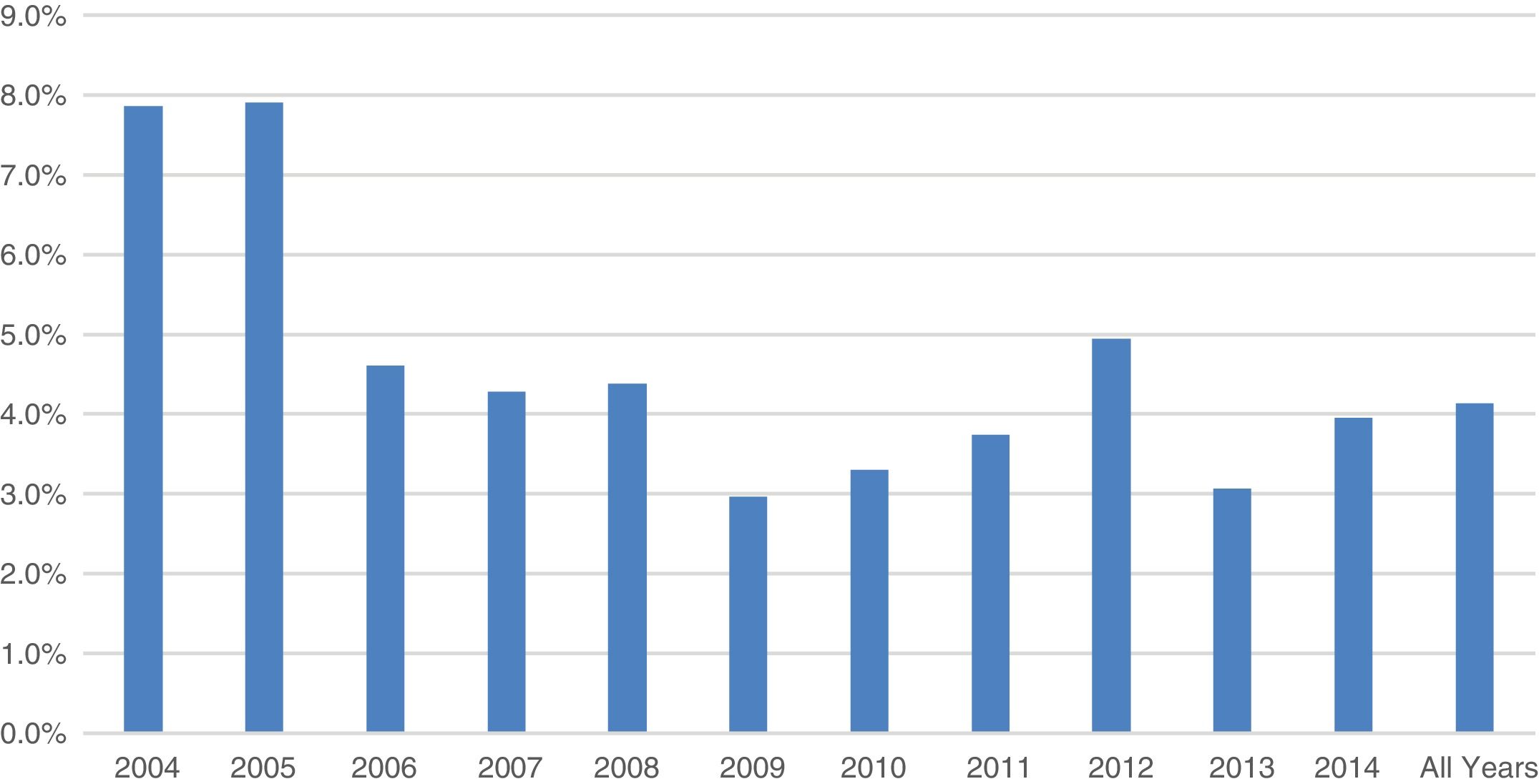
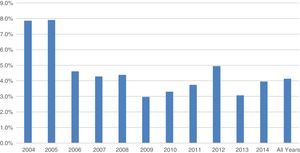
ResultsA total of 9341 patients underwent patch testing in the 8 participating hospitals; 386 of them (4.1%, 95% CI, 3.75%–4.5%) had positive reactions to PPD. The proportion began to decrease between 2004 and 2007, after which it held steady at around 4%. Higher rates of positivity were seen in the first 2 years (Fig. 1).
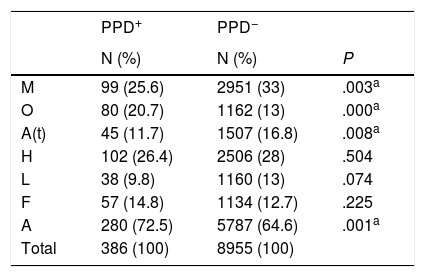
The characteristics of patients with contact allergy to PPD are shown in Table 1 according to components of the MOAHLFA index: 25.6% were men, and significantly more patients (72.5%) were older than 40 years (P < .001); 20.7% had signs that allergy was workplace-related (P < .001). The most frequent locations were the hands and scalp.
Characteristics of Patients Sensitized and Not Sensitized to PPD According to Components of the MOAHLFA Index
| PPD+ | PPD− | ||
|---|---|---|---|
| N (%) | N (%) | P | |
| M | 99 (25.6) | 2951 (33) | .003a |
| O | 80 (20.7) | 1162 (13) | .000a |
| A(t) | 45 (11.7) | 1507 (16.8) | .008a |
| H | 102 (26.4) | 2506 (28) | .504 |
| L | 38 (9.8) | 1160 (13) | .074 |
| F | 57 (14.8) | 1134 (12.7) | .225 |
| A | 280 (72.5) | 5787 (64.6) | .001a |
| Total | 386 (100) | 8955 (100) |
Abbreviations: A, age over 40 years; A(t), history of atopy; F, facial involvement; H, hand involvement; L, leg involvement; M, male sex; O, occupation; PPD, p-phenylenediamine.
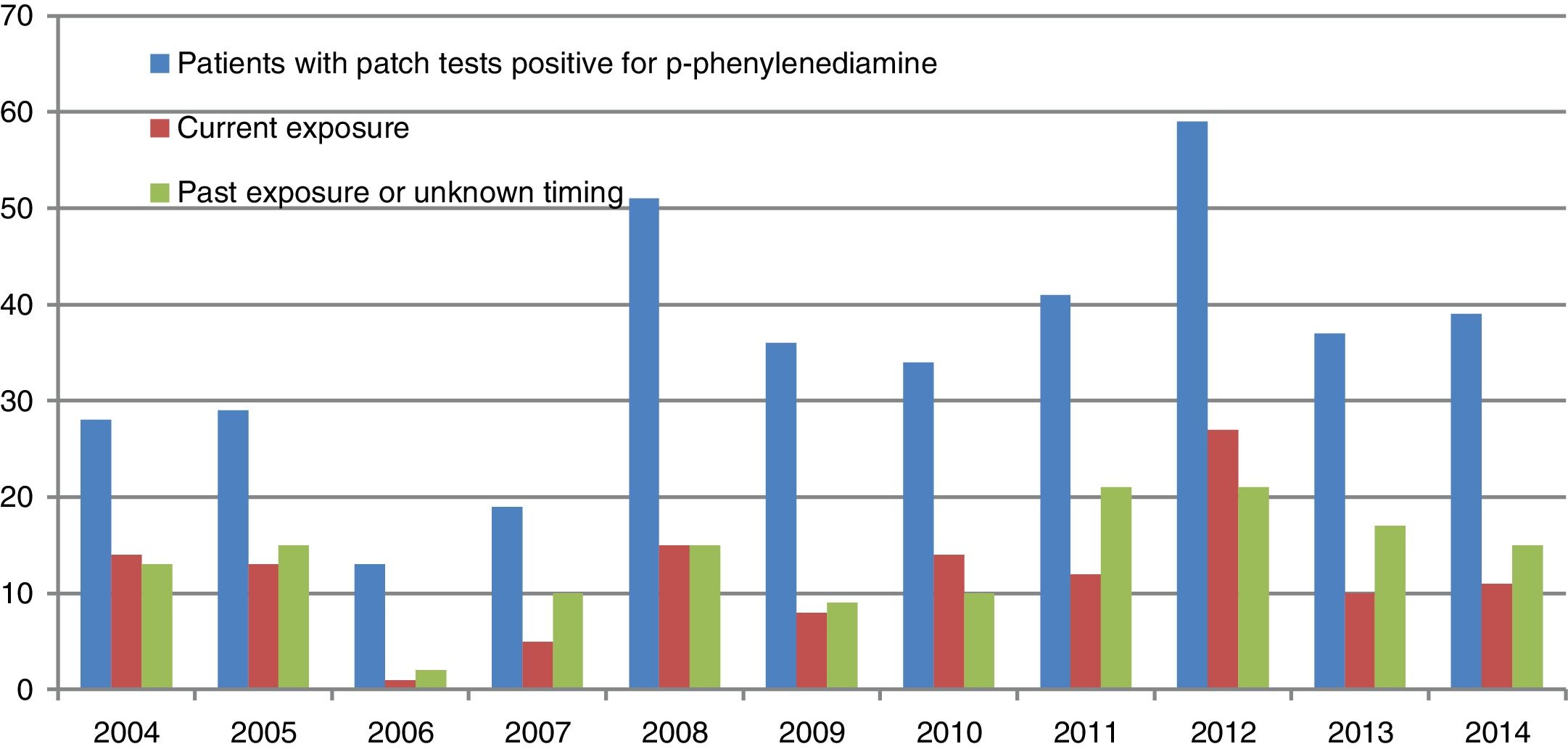
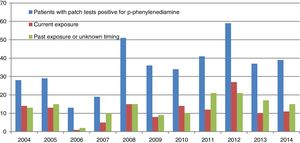
Fig. 2illustrates the numbers of patients with patch tests positive to p-phenylendiamine and relevant current or past (or unknown) exposure exposure during the period between 2004 and 2014. Information about relevant exposure was known for 283 of the 386 patients with PPD reactions and unknown for 103 patients. Most of the 283 patients had been exposed to hair dyes: exposure was current in 130 cases, past in 109, and at an unspecified time in 44. Workplace exposure was most frequent among individuals working in hair salons, rubber and plastics manufacturing, food preparation, and textile and leather working.
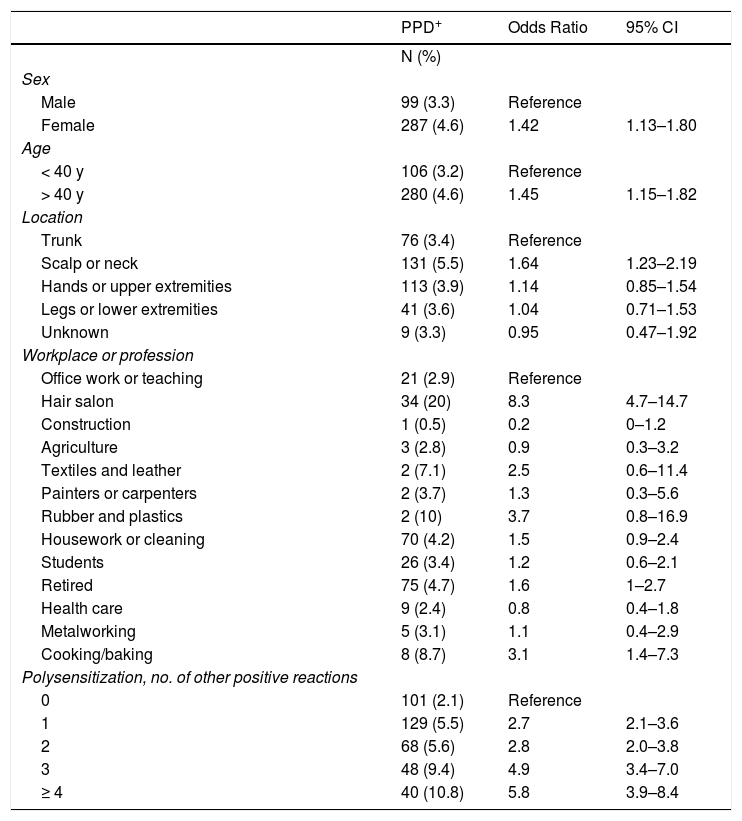
The risk factors that were statistically related to PPD allergy were sex, age over 40 years, multiple sensitizations, and profession — especially work in hair salons (OR, 8.3; 95% CI, 4.7–14.7) or rubber and plastics manufacturing (OR, 3.7; 95% CI, 0.8–16.9) (Table 2).
Risk Factors for Contact Allergy to PPD
| PPD+ | Odds Ratio | 95% CI | |
|---|---|---|---|
| N (%) | |||
| Sex | |||
| Male | 99 (3.3) | Reference | |
| Female | 287 (4.6) | 1.42 | 1.13–1.80 |
| Age | |||
| < 40 y | 106 (3.2) | Reference | |
| > 40 y | 280 (4.6) | 1.45 | 1.15–1.82 |
| Location | |||
| Trunk | 76 (3.4) | Reference | |
| Scalp or neck | 131 (5.5) | 1.64 | 1.23–2.19 |
| Hands or upper extremities | 113 (3.9) | 1.14 | 0.85–1.54 |
| Legs or lower extremities | 41 (3.6) | 1.04 | 0.71–1.53 |
| Unknown | 9 (3.3) | 0.95 | 0.47–1.92 |
| Workplace or profession | |||
| Office work or teaching | 21 (2.9) | Reference | |
| Hair salon | 34 (20) | 8.3 | 4.7–14.7 |
| Construction | 1 (0.5) | 0.2 | 0–1.2 |
| Agriculture | 3 (2.8) | 0.9 | 0.3–3.2 |
| Textiles and leather | 2 (7.1) | 2.5 | 0.6–11.4 |
| Painters or carpenters | 2 (3.7) | 1.3 | 0.3–5.6 |
| Rubber and plastics | 2 (10) | 3.7 | 0.8–16.9 |
| Housework or cleaning | 70 (4.2) | 1.5 | 0.9–2.4 |
| Students | 26 (3.4) | 1.2 | 0.6–2.1 |
| Retired | 75 (4.7) | 1.6 | 1–2.7 |
| Health care | 9 (2.4) | 0.8 | 0.4–1.8 |
| Metalworking | 5 (3.1) | 1.1 | 0.4–2.9 |
| Cooking/baking | 8 (8.7) | 3.1 | 1.4–7.3 |
| Polysensitization, no. of other positive reactions | |||
| 0 | 101 (2.1) | Reference | |
| 1 | 129 (5.5) | 2.7 | 2.1–3.6 |
| 2 | 68 (5.6) | 2.8 | 2.0–3.8 |
| 3 | 48 (9.4) | 4.9 | 3.4–7.0 |
| ≥ 4 | 40 (10.8) | 5.8 | 3.9–8.4 |
Abbreviation: PPD, p-phenylenediamine.
This multicenter study including all patients suspected of and tested for contact eczema treated in the dermatology departments of 8 Spanish hospitals between 2004 and 2014 found that the prevalence of allergy to PPD was around 4%, without significant differences between centers. The rate has remained constant over the years, with the exception of the first 2 years, 2004 and 2005, when 7% of patch-tested patients reacted to PPD. Selection bias could explain the higher frequency in those years, given that the data came from a single center at that time. Higher rates of PPD sensitization were reported in earlier Spanish studies, but discrepancies may be attributable to methodological differences, time period studied, selection bias, or PPD test concentrations.9–15 These frequencies are similar to those reported for other European countries.2,16 The intensity of reaction to PPD has been found to be greater in Mediterranean countries, probably related to the use of darker hair dyes.1 The maximum allowable PPD concentration in hair dyes was reduced from 6% to 2% in 2009, although the decrease was not associated with a change in the frequency of allergic eczema in this or other studies.5 Various factors may be keeping the frequency of PPD sensitization high. The henna dye used to create temporary tattoos is usually adulterated with PPD and can induce sensitization; nevertheless, it is unregulated.17 One lifestyle trend that may be relevant is that more and more patients are using cosmetics containing PPD earlier in life.4 Finally, hair salon workers often fail to use gloves until contact eczema develops, and in some cases they reuse of gloves contaminated with PPD.
The clinical profile based on the MOAHLFA information showed that most sensitized patients are women older than 40 years of age, consistent with the results of earlier studies.4,16 This profile is attributable to contact with hair dyes containing the compound.
One of the risk factors for PPD contact allergy identified in this study was professional exposure, especially work in hair salons, where hair dyes are commonly applied, consistent with previous reports.2,18,19 Repeated and prolonged contact with these products probably explains the high rate of sensitization in salon workers.20
Polysensitization defined as reaction to 3 or more unrelated chemicals was another risk factor for PPD sensitization. This finding has also been reported previously.21 Patients in this category may have been exposed to various allergens at the same time, or they may have a genetic predisposition to contact allergy.
This study shares limitations common to multicenter studies. The participating centers did not all carry out the patch tests using the same procedures and materials (type of occlusion, allergen concentrations, and vehicles). In addition, the reading of test reactions and the assessment of workplace relevance in particular are subject to observer bias. Sensitization frequencies in patients who undergo patch testing cannot be extrapolated to prevalence rates in the general population. The findings can be expected to overestimate population prevalence, due to selection bias.
ConclusionsThe rate of contact allergy to PPD was high in Spain at around 4% in this series of patch-tested patients suspected of contact eczema between 2004 and 2014 in 8 hospitals. The rates did not differ significantly over the years.
Risk factors for PPD allergy are female sex, age over 40 years, workplace exposure in hair salons, and polysensitization.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Sánchez-Pérez J, Descalzo-Gallego MA, Silvestre JF, Fernández-Redondo V, García-Gavín J, Ruiz-Gonzalez I, et al. ¿Sigue siendo la parafenilendiamina un alérgeno de contacto prevalente en España. Actas Dermosifiliogr. 2020;111:47–52.