The starting dose for narrowband UV-B phototherapy is determined by a patient's skin phototype or minimal erythema dose (MED). Calculation of MED identifies patients with unsuspected photosensitivity. The aim of this study was to investigate the influence of factors such as concomitant use of photosensitizing agents, diagnosis, and combination with acitretin in patients with psoriasis on the frequency and severity of adverse effects in patients with a low MED to narrowband UV-B phototherapy.
Material and methodsWe undertook a retrospective observational cohort study between February 1, 2009 and March 31, 2015. MED values were classified as normal or low.
ResultsIn total, 302 patients with different skin conditions started narrowband UV-B phototherapy at a dose determined by their MED. No differences were found between patients with a low MED and those with a normal MED for number of drugs taken (P=.071) or use of photosensitizing agents (P=0.806). Following adjustment for age, sex, and phototype, the multivariate analysis showed that psoriasis exerted a protective effect against a low MED (OR=0.31 [95% CI, 0.16-0.58]). No significant risk of erythema or pruritus was detected in patients with a low MED (OR=1.68; 95% CI, 0.91-3.29 and OR=2.04; 95% CI, 0.99-4.22, respectively).
ConclusionsPsoriasis protects against a low MED. Although erythema and pruritus were more common in patients with a low MED, the differences were not significant.
La dosis de inicio en la fototerapia UVB de banda estrecha (UVBBE) viene determinada por el fototipo o por la determinación de la dosis eritematógena mínima (DEM). El cálculo de la DEM identifica pacientes con fotosensibilidad no sospechada. El objetivo de nuestro estudio es conocer la influencia que puedan tener en una DEM disminuida los fármacos fotosensibilizantes concomitantes, el diagnóstico, la asociación con acitretina en pacientes con psoriasis y evidenciar si la DEM alterada provoca más reacciones adversas y más graves.
Material y métodosSe trata de un estudio observacional de una cohorte retrospectiva desde el período comprendido entre el 1 de febrero de 2009 al 31 de marzo de 2015. La determinación de la DEM se categorizó en DEM normal o patológica.
ResultadosTrescientos dos pacientes con distintas dermatosis inician UVBBE en función de la DEM. No se han encontrado diferencias entre el grupo con DEM patológica respecto al normal, ni en el número de fármacos consumidos (p=0,071), ni en el potencial fotosensibilizante (p=0,806). El análisis multivariante ajustado por edad, sexo y fototipo reveló que la psoriasis es un factor protector de DEM patológica (OR=0,31 [IC 95%: 0,16-0,58]). No se encontró riesgo significativo de eritema ni prurito en los pacientes con DEM alterada OR=1,68 (IC 95%: 0,91-3,29) y OR=2,04 (IC 95%: 0,99-4,22), respectivamente.
ConclusionesLa psoriasis protege de tener una DEM patológica. Si bien el eritema y el prurito fueron más frecuentes en los pacientes con DEM patológica, las diferencias no fueron estadísticamente significativas.
Narrowband UV-B (NB-UVB) radiation is a phototherapy modality that arose from the coincidence between the action spectrum of UV radiation in patients with psoriasis1 and the 311-nm emission spectrum. This modality has a lower capacity for induction of erythema.2 Since then, other skin diseases have benefited from this treatment.
NB-UVB phototherapy can cause pruritus, although erythema is the most frequent adverse effect.3 The intensity of erythema can lead to dose increases and can cause treatment to be withdrawn if it is symptomatic and persistent. Of note, the mild and asymptomatic forms are the most prevalent.4
The starting dose is determined based on the skin phototype or on the calculation of the minimal erythema dose (MED). The MED tells us about the sensitivity of the skin to UV radiation from a specific light source5,6 and is defined as the dose necessary (J/cm2) to obtain minimal perceptible erythema at the site of phototesting (reading at 24hours). However, MED is not calculated in most phototherapy units, as it is time-consuming and requires expert nursing care. The skin phototype is not a good parameter for the determination of the starting dose, since very different MED values can be observed for the same phototype.7
Clinical photosensitivity is yet another adverse effect of NB-UVB radiation. Diagnosis is based on an accurate clinical history, a skin examination, and phototesting, which confirms photosensitivity.8,9 Although phototesting results are normal with some photodermatoses, they are always indicative of disease in drug-associated systemic photosensitivity.10 In a prospective study, Cameron et al.11 identified 3 groups of drugs that affect MED, namely, nonsteroidal anti-inflammatory drugs, phenothiazines, and calcium antagonists.
The Spanish Photobiology Group (Grupo Español de Fotobiología) recently standardized threshold MED values for the various skin phototypes, with particular emphasis on individuals with a low MED.12
Guidelines from the United Kingdom,3 Spain,13 and France14 make recommendations on treatment protocols, although only the British guidelines strongly support calculation of the MED before starting phototherapy with the aim of detecting photosensitivity that was neither suspected by the physician nor reported by the patient.3 The choice between MED and phototype does not affect therapeutic efficacy in patients with psoriasis,15 although as these patients have comorbid conditions that are managed with long-term treatment, the threshold for erythema may be reduced.11,16 MED can make it possible to identify systemic photosensitivity and thus prevent severe adverse reactions.
Given a low MED, our objective was to determine the influence of variables such as age, sex, concomitant medication, diagnosis, and combination with acitretin in patients with psoriasis and to clarify whether a low MED could lead to more frequent and severe adverse reactions.
Material and MethodsStudy designWe performed an observational study of a retrospective cohort that was reviewed and approved by the Research Ethics Committee of Lugo and Santiago. Our research was performed following the principles of the Declaration of Helsinki.
Study populationThe study population comprised patients referred from dermatology clinics to the Phototherapy Unit of Complejo Hospitalario Universitario Clínico de Santiago de Compostela, Santiago de Compostela, Spain to begin narrowband UV-B phototherapy between February 1, 2009 and March 31, 2015.
We included patients with skin diseases that were likely to benefit from phototherapy, namely, psoriasis, atopic dermatitis, vitiligo, plaque parapsoriasis, primary T-cell cutaneous lymphoma, acute and chronic pityriasis lichenoides, prurigo, pruritus sine materia, metabolic pruritus, urticaria pigmentosa, lichen ruber planus, disseminated granuloma annulare, polymorphous light eruption, and solar urticaria. Patients aged under 14 years, for whom MED was not calculated, were excluded.
Phototesting protocolThe MED was calculated using the phototherapy cabinet (UV 7002 system [Waldmann] equipped with 21 F79/120W-TL01 tubes [311nm]). We irradiated 8 areas (1.5cm) on an unaffected area of the back with progressively increasing doses (increments of 20%) 1 day before initiation of treatment. In patients with phototypes I and II, the corresponding doses were 0.24, 0.29, 0.35, 0.42, 0.50, 0.60, 0.72, and 0.86J/cm2. In phototypes III and IV, the doses were increased to 1.00 and 1.20J/cm2. In order to obtain the erythemal irradiance of the TL01 lamps, we used a double-monochromator spectroradiometer (MACAM- SR 2271, MACAM) to calculate the absolute irradiance (4.73mw/cm2) and the irradiance with the potential to induce erythema (0.26mw/cm2), both of which values are measured annually. The resulting quotient is the correction factor used to transform these absolute irradiated doses (J/cm2) into erythemal doses (mJ/cm2): 13.19, 15.94, 19.24, 23.09, 27.49, 32.99, 39.58, 47.28, 54.98, and 65.97mJ/cm2, respectively. These biological effective doses for erythema correspond to the doses of the solar simulators; low MED can be determined using the TL01 lamps.
Study variablesWe recorded sociodemographic variables, clinical history, diagnosis, phototype, and MED value. We also recorded the drugs administered, doses (starting, final, and total [J/cm2]), the number of sessions, and adverse reactions (mild erythema [asymptomatic]; moderate erythema [erythema and transient pruritus<24h]; and severe erythema [erythema and pruritus>24h]; and pruritus). All data were retrieved from the specific phototherapy histories and from the electronic clinical history system of Galicia (IANUS). A database was designed specifically for this study.
The retrospective cohort was divided into 2 groups depending on the classification of MED as low or normal. The threshold for a low MED was defined by Pérez Ferriols et al.12 using the solar simulator as source.
Thus, in individuals with phototype I, MED values <0.12J/cm2 correspond to an erythemal dose<7mJ/cm2; in patients with phototype II, MED values <0.34J/cm2 correspond to an erythemal dose <19mJ/cm2; in patients with phototype III, MED values <0.49J/cm2 correspond to an erythemal dose<27mJ/cm2; and in patients with phototype IV, MED values <0.69J/cm2 correspond to an erythemal dose<38mJ/cm2.
Sample sizeFrom a clinical viewpoint, the prevalence of individuals with a low MED is approximately 5%. Assuming a significance of 5%, statistical power of 80%, and a 4% loss of data from clinical records due to underrecording, it was necessary to include 302 individuals in order to achieve a precision of 2.50%. The sample size calculation was performed using Ene3.0.17
Statistical analysisBivariate tests were performed to compare both groups. Categorical variables were compared using the chi-square test. Continuous variables were compared using the t test or Mann-Whitney test depending on normality, which was determined using the Kolmogorov-Smirnov test (with a Lilliefors correction). The risk of experiencing an adverse reaction was determined using the odds ratio (OR) and its 95% confidence interval (95% CI). Logistic regression was used to evaluate risk. Variables with a P value lower than 0.2 were entered into the multivariate regression model. All analyses were performed using IBM SPSS Statistics Version 19 (IBM Corp).18 Statistical significance was set at P<.05.
ResultsPatientsThe study population comprised 302 patients, of whom 54% were men. The median (IQR) age was 49 (34-60) years. The most common diagnosis was psoriasis (148 patients [49%]), followed by atopic dermatitis (36 [11.9%]), cutaneous T-cell lymphoma (18 [6.0%]), photodermatosis (11 [3.6%]), prurigo (12 [4.0%]), and lichen planus (4.0%). Other conditions were diagnosed in 65 patients (21.5%).
In 156 cases (51.7%), the patient was not taking concomitant drugs, 74 (25.5%) were taking 1 drug, and 72 (23.8%) were taking 2 or more drugs. A total of 101 patients (69.2%) were taking photosensitizing drugs (Table 1).
Patient Characteristics.
| Overall Sample N=302 No. (%) | Normal MED n=240 (79.5%) No. (%) | Low MED n=62 (20.5%) No. (%) | P Valuea | |
|---|---|---|---|---|
| Sex (male)b | 163 (54.0) | 115 (47.9) | 48 (77.4) | <.001 |
| Median (IQR) age, yc | 49.00 (33.75-60.00) | 47.00 (33.00-58.00) | 56 (35.50-70.00) | .003 |
| Medical history | 205 (67.9) | 157 (65.4) | 48 (77.4) | .071 |
| Diagnosisb | <.001 | |||
| Atopic dermatitis | 36 (11.9) | 28 (11.7) | 8 (12.9) | |
| Psoriasis | 148 (49.0) | 131 (54.6) | 17 (27.4) | |
| Cutaneous T-cell lymphoma | 18 (6.0) | 13 (5.4) | 5 (8.1) | |
| Photodermatosis | 11 (3.6) | 8 (3.3) | 3 (4.8) | |
| Prurigo | 12 (4.0) | 10 (4.2) | 2 (3.2) | |
| Lichen planus | 12 (4.0) | 11 (4.6) | 1 (1.6) | |
| Other | 65 (21.5) | 39 (16.3) | 26 (41.9) | |
| Phototype | .013 | |||
| I-II | 110 (36.4) | 91 (37.9) | 19 (30.6) | |
| III | 138 (45.7) | 114 (47.5) | 24 (38.7) | |
| IV | 54 (17.9) | 35 (14.6) | 19 (30.6) | |
| Comorbid conditionsb,d | ||||
| AHT | 64 (21.3) | 46 (19.2) | 18 (29.0) | .090 |
| Diabetes | 20 (6.6) | 15 (6.3) | 5 (8.1) | .609 |
| Hyperlipidemia | 71 (23.5) | 53 (22.1) | 18 (29.0) | .250 |
| Anxiety-depression syndrome | 32 (10.6) | 27 (11.3) | 5 (8.1) | .468 |
| Psoriatic arthritis | 34 (11.3) | 24 (10.6) | 10 (16.1) | .173 |
| Thyroid disease | 20 (6.6) | 13 (5.4) | 7 (11.3) | .097 |
| Asthma or rhinitis | 55 (18.2) | 42 (17.5) | 13 (21.0) | .528 |
| No. of drugsb | .071 | |||
| None | 156 (51.7) | 131 (54.6) | 25 (40.3) | |
| 1 | 74 (25.5) | 58 (24.2) | 16 (25.8) | |
| ≥2 | 72 (23.8) | 51 (21.3) | 21 (33.9) | |
| Photosensitizing drugs | 101 (69.2) | 76 (69.7) | 25 (67.6) | .806 |
| Acitretin | 21 (7.0) | 19 (7.9) | 2 (3.2) | .196 |
| Adverse effectsb | 117 (38.7) | 89 (37.1) | 28 (45.2) | .244 |
| Type of adverse effectb,d | ||||
| Erythema | 83 (27.5) | 61 (25.4) | 22 (35.5) | .113 |
| Pruritus | 61 (20.2) | 43 (17.9) | 18 (21.0) | .052 |
| PLE | 25 (8.3) | 20 (8.3) | 5 (8.1) | .945 |
| Solar urticaria | 1 (0.3) | – | 1 (0.4) | – |
Abbreviations: AHT, arterial hypertension; IQR, interquartile range; MED, minimal erythema dose; PLE, polymorphous light eruption.
The sample was divided into 2 groups depending on whether MED was normal or low.12 MED was normal in 240 patients (79.5%) and low in 62 (20.5%).
We found statistically significant differences between the groups according to sex (normal MED 47.9% vs low MED 77.4% in men, P<.001) and age (median age was 47 [33-58] years in patients with a normal MED and 56 [35.5-70] years in those with a low MED [P=.003]). Statistically significant differences were also found in the distribution of diagnoses between the groups (P<.001). However, no differences were found in the number of drugs consumed (P=.071), even when these where photosensitizing drugs (P=.806), or in the combination of phototherapy and acitretin (P=.196). Adverse reactions (erythema, pruritus, polymorphous light eruption, and solar urticaria) were recorded in 117 patients (38.7%). MED was low in 45.2% and normal in 37.1%. Erythema presented with a clinically relevant difference in patients with a low MED (35.5%) compared with those with a normal MED (25.4%). However, this clinical relevance was not observed in the case of pruritus, since 17.9% of patients with a normal MED reported the condition compared with 21.0% of patients with a low MED. Table 1 shows the results of this analysis in more detail. As for phototype, in patients with phototype IV, the percentage of patients with a low MED is higher than in patients with a normal MED (30.6% vs 14.6%; P=.013).
Multivariate analysisIn order to construct the multivariate models and evaluate the effect of adverse reactions, the variables we selected for adjustment were those that, on the one hand, proved to be clinically relevant for MED and that, on the other, had a P value <.02 in the bivariate analysis. The variables that fulfilled these criteria were sex, age, diagnosis, and phototype. As shown in Table 2, Model 1 assesses the risk of adverse reactions in patients with a low MED compared with those whose MED was normal. Models 2 and 3 show an individual analysis of the most common adverse effects, namely, erythema and pruritus. Patients with a low MED did not have a greater risk than those who had a normal MED (Model 1). Similarly, refining the analysis by the type of adverse reaction did not reveal a significant risk. The risk of erythema expressed as the odds ratio (OR) in patients with a low MED was1.68 (95% CI, 0.91-3.29) (Model 2) and that of pruritus was 2.04 (95% CI, 0.99-4.22) (Model 3).
Risk of Adverse Reactions.
| Model | OR (95% CI) | P Valuea | aOR (95% CI)a | P Valuea |
|---|---|---|---|---|
| Model 1, adverse effects | 1.40 (0.79-2.46) | .246 | 1.73 (0.91-3.29) | .094 |
| Model 2, erythema | 1.61 (0.89-2.93) | .115 | 1.68 (0.91-3.29) | .130 |
| Model 3, pruritus | 1.87 (0.99-3.55) | .054 | 2.04 (0.99-4.22) | .054 |
Abbreviations: aOR, adjusted odds ratio; CI, confidence interval; OR, odds ratio.
These analyses revealed an unexpected finding with respect to the diagnosis. The bivariate analysis revealed that psoriasis exerted a protective effect against low MED (OR,0.31 [95% CI, 0.17-0.58]). This significance persisted in the multivariate analysis adjusted for age, sex, and phototype (OR,0.31 [95% CI, 0.16-0.58]).
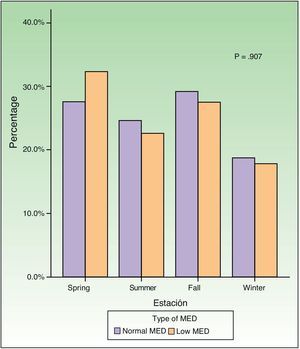
Study of dose and seasonalityComparison of the mean values of the dose for each group showed that the starting, final, and total doses were significantly different (P<.001, P=.004, and P=.001, respectively). However, the increase in dose and number of sessions was not significant (P=.304) (Table 3). Finally, we determined whether the distribution of MED differed according to the season of the year this value was determined; however, no significant differences were observed (Fig. 1).
Treatment Variables.
| Total N=302 | Normal MED n=240 (79.5%) | Low MED n=62 (20.5%) | P Valuea | |
|---|---|---|---|---|
| Dose, J/cm2b | ||||
| Starting | 0.35 (0.25-0.50) | 0.42 (0.35-0.50) | 0.24 (0.17-0.29) | <.001 |
| Final | 2.1 (1.37-2.31) | 2.13 (1.49-2.32) | 1.65 (0.54-2.17) | .004 |
| Total | 33.23 (20.20-48.20) | 35.39 (22.70-48.98) | 25.95 (6.85-46.03) | .001 |
| Dose increaseb | 1.56 (0.99-1.87) | 1.56 (1.13-1.82) | 1.41 (0.56-1.97) | .304 |
| No. of sessionsb | 26 (21-32) | 26 (21-32) | 26 (19.5-35) | .884 |
Abbreviation: MED, minimal erythema dose.
Our study showed the appropriateness of determining MED in patients with skin diseases susceptible to treatment with NB-UVB radiation.
NB-UVB radiation is considered to be an effective treatment modality, with frequent adverse reactions such as erythema and pruritus. Other, less common adverse effects have also been reported. For example, photosensitivity was reported during phototherapy: a patient whose MED was not determined and who experienced an eczematous reaction was diagnosed with chronic actinic dermatitis.19 A subsequent study in which a patient also affected by psoriasis was diagnosed with chronic actinic dermatitis when a low MED was recorded; the diagnosis was confirmed with a photobiology study.20
Drug-induced photosensitivity has also been observed during phototherapy, reaching 10.3% in one retrospective study.21 A prospective study revealed that patients receiving treatment with nonsteroidal anti-inflammatory drugs, calcium antagonists, and phenothiazines had a significantly reduced MED.11 However, we found that neither the number nor the photosensitizing capacity of concomitant medication affected the MED value. Only 2 of the patients with a reduced MED in our study were diagnosed with systemic drug-induced photosensitivity, and 5 patients experienced suspicious acute erythematous reactions caused by unconfirmed drug-induced photosensitivity.21
Two patients receiving treatment with acitretin and NB-UVB phototherapy had a low MED: one was taking tamsulosin and the other an angiotensin-converting enzyme inhibitor, metformin, and a statin. We believe that the reduced MED was associated with these drugs and not with acitretin. Etretinate has been reported to induce a phototoxicity mechanism,22 but acitretin has not. The recommendation to reduce the dose in these patients was not based on the reduction in MED, but on a possible mechanism of action that enables acitretin to act against epidermal acanthosis.23
In our study, older patients and males had a low MED. Comparable results have been published for age, and, while not clinically relevant, more persistent erythema was observed. We did not find similar results with respect to sex or its influence on MED.24–26
The distribution of phototypes differed between individuals with a normal MED and those with a low MED. This finding is difficult to interpret, since other studies have reported that phototype was not associated with MED, although patients with high phototypes had higher MED values.27,28
In contrast with the results from a previous study,29 we found that a low MED did not affect the number of sessions.
The starting dose in patients who received phototherapy was determined based on their MED. We observed that it was significantly lower in patients with a low MED, thus avoiding a higher risk of adverse reactions, since the risk is dose-dependent.11 In addition to the initial dose, we observed how both the final dose and the total cumulative dose were significantly lower in individuals with a low MED. Indeed, the fact that we did not observe a greater risk of adverse reactions in this group was because patients began phototherapy at lower doses. Therefore, consistent with other authors, we believe that adjusting the initial dose based on MED is a useful way of reducing the frequency and severity of adverse reactions.30
Even though erythema and pruritus were more common patients with low MED, the risk calculated was not significantly greater. Furthermore, the dose increase did not reveal differences between individuals with normal and low MED, when it could be expected that if erythema or pruritus had been more frequent in individuals with a low MED, the dose increase would have been smaller, again justifying the need to determine the MED in order to prevent the adverse reactions inherent to phototherapy.31
Finally, we observed a protective effect on the outcome of phototesting among patients with psoriasis, namely, they are less likely to have a low MED, although this has not been confirmed elsewhere.7 This finding could justify the decision to determine MED in this group, with the aim of starting treatment at a higher dose than that corresponding to their phototype, thus reducing the number of treatments with no loss of therapeutic effectiveness.
Ethical DisclosuresProtection of humans and animalsThe authors declare that no tests were carried out in humans or animals for the purposes of this study.
Confidentiality of dataThe authors declare that they have followed their institutional protocols on publication of patient data.
Right to privacy and informed consentThe authors declare that no private patient data appear in this article.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
I am grateful to my boss, Professor Jaime Toribio for his faith in me and for his interest in the smooth running of the Phototherapy Unit.
Please cite this article as: Rodríguez-Granados MT, Estany-Gestal A, Pousa-Martínez M, Labandeira J, Gato Otero R, Fernández-Redondo V. ¿Es útil la determinación de la dosis eritematógena mínima previa a la fototerapia ultravioleta B de banda estrecha?. Actas Dermosifiliogr. 2017;108:852–858.