Porokeratosis is a keratinization disorder clinically characterized by the presence of annular plaques surrounded by a discreetly keratotic border. It was first described back in 1893 by Mibelli, and since then, 6 different types of porokeratosis have been described: Mibelli's porokeratosis, superficial and disseminated actinic porokeratosis, porokeratosis plantaris, palmaris et disseminata, linear porokeratosis, and some rarer variants such as ptychotropic and giant porokeratosis.1 All subtypes share the histopathological presence of the cornoid lamella, a column of compact parakeratosis, with a focal absence of the granular layer, and the concomitant presence of dyskeratotic cells.2
A 52-year-old man presented with disseminated dermatosis, bilaterally and symmetrically, on both the upper and lower extremities, with dorsal surface involvement in both forearms and anterior region of the thighs. The lesions occasionally caused pruritus. Clinical examination revealed the presence of rounded erythematous plaques with a discreet keratotic border (Fig. 1.A). Dermatoscopy revealed the presence of erythema and follicular scaling without a defined dermatoscopic pattern (Fig. 1B). Additionally, the patient reported a past medical history of 4 basal cell carcinomas, all of which were surgically excised with direct closure 2 years earlier, without any signs of recurrence.
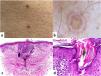
A. Clinical image of the dermatosis characterized by erythema and thin scale that coalesce in round-shaped plaques with discrete keratotic borders. B. Dermatoscopic image: presence of erythema and follicular distribution of scales without a defined dermatoscopic pattern. C. Hematoxylin and eosin (H&E) stain, ×10. Histopathology: the epidermis exhibits orthokeratotic hyperkeratosis and areas of moderate regular acanthosis. Within the dermal thickness, dilated follicular infundibula containing laminar keratin and columns of compact parakeratotic hyperkeratosis corresponding to cornoid lamellae can be seen, with such structures being connected to the follicular epithelium where there is an absence of the granular layer. D. Hematoxylin and eosin (H&E) stain, ×4 and ×40. In other areas of the section, cystic structures containing cornoid lamellae can also be seen, leading to a diagnosis of follicular porokeratosis.
The initial clinical suspicion was multiple actinic keratosis, and treatment was based on a 12-week course of topical 5-fluorouracil, which turned out unresponsive. Therefore, an excisional biopsy of one of the lesions was performed, with suspected possible Bowen's disease. Histopathologically, the epidermis showed orthokeratotic hyperkeratosis and areas of moderate regular acanthosis. In the thickness of the dermis, dilated follicular infundibula with laminar keratin were found, as well as columns of compact hyperkeratosis with parakeratosis that corresponded to cornoid lamellae, connected to the follicular epithelium, where the granular layer was absent (Fig. 2C). In other areas of the section, cystic structures containing cornoid lamellae were seen (Fig. 2D). These findings led to the diagnosis of follicular porokeratosis.
A. Clinical image showing papular lesions that coalesce to form brown-colored plaques. B. Dermatoscopic image of these millimetric lesions with a hyperkeratotic peripheral border and central scale, with the double-track sign, and a homogenous scar-like central region. C. Hematoxylin and eosin (H&E) stain, ×10. Histopathology: exhibits an epidermis with a cornified layer, basal layer hyperpigmentation, and a dilated follicular infundibulum in the central region of the section. In the superficial and middle dermis, moderately dense infiltrates are arranged in focal areas. D. Hematoxylin and eosin (H&E) stain, ×40. At higher magnification, areas without a granular layer and the presence of dyskeratotic cells can be seen, which means that this parakeratotic hyperkeratosis corresponds to the cornoid lamella.
A 58-year-old man consulted due to the presence of pruritic disseminated dermatosis, bilateral and symmetrical, on the upper extremities, trunk, and lower extremities, involving the anterior and posterior regions of the forearms, flanks, lumbar region, and inner thighs. Clinically, papular lesions with keratotic scaling at the border were described, with a tendency to converge forming small, well-defined brown plaques <1cm in diameter (Fig. 2A). Dermatoscopy revealed the presence of a hyperkeratotic peripheral border, the presence of a central scale with the double-track sign, and a central homogenous scar-like region (Fig. 2B). He did not report any other significant past medical history. The rest of the skin and its appendages showed no notable changes.
The histopathological examination of an incisional biopsy of one of the lesions showed an epidermis with a cornified layer, hyperpigmentation of the basal layer, and, in the central region of the section, a dilated follicular infundibulum. Focal moderately dense infiltrates were seen in the superficial and mid-dermis (Fig. 2C). At higher magnification, compact parakeratosis was seen inside the infundibulum, areas where the granular layer was not seen, along with the presence of dyskeratotic cells corresponding to the cornoid lamella (Fig. 2D).
Follicular porokeratosis was proposed as a distinct variety from those described before in 2009 by Pongpudpunth et al.3. Since then, nearly 21 cases have been reported in the overall medical literature currently available. The lesions are more common in women with a male-to-female ratio of 2:3. The age of onset varies from 19 to 85 years, although the peak incidence by age is concentrated between the ages of 20 and 60.4
The pathogenesis of the follicular variety is unknown to this date. However, the involvement of exposure to UV radiation, as it happens with other forms of porokeratosis, has been suggested due to the documented increased expression of protein P53.5 There may be concomitant genetic factors too, since one case has been reported in the medical literature available of an autosomal dominant inheritance pattern.6
It predominantly occurs in photo-exposed areas. By order of frequency, it has been reported mainly on the face, followed by the trunk and extremities, although 2 cases involving the buttocks have been reported too.7 The most common clinical presentation is annular, erythematous plaques, whether brown or skin-colored, of follicular appearance and a discreetly keratotic border, with size ranging from 0.2cm to 2cm in diameter.8
In most patients, it is asymptomatic, and only 4 cases presented occasional pruritus as the predominant symptom.9 This description also corresponds to what was seen in the patients presented in this scientific letter.
In histopathology, the cornoid lamella can be seen confined solely to the hair follicle, there is focal absence of the granular layer, and presence of dyskeratotic cells as the main findings. Coincidentally, though, atrophic epidermis, focal interface changes, mucin deposits, and perivascular infiltrates in the superficial dermis can be present.10,11
The clinical and histopathological differential diagnosis of follicular porokeratosis includes other porokeratotic dermatoses: Mibelli's porokeratosis, linear porokeratosis, and ptychotropic form,12 as well as other dermatoses such as actinic keratosis, discoid lupus, or superficial squamous cell carcinoma.8
Regarding treatment, as it happens in other cases of porokeratosis, multiple therapeutic modalities have been used with variable outcomes. These include 5% imiquimod cream, keratolytics, 5-fluorouracil cream, curettage, and surgical excision, with the latter providing a lower rate of recurrences.13
Follicular porokeratosis can be understood from two different perspectives: first, as a histopathological variety of broader subtypes of porokeratosis, such as disseminated superficial actinic porokeratosis (DSAP). Therefore, in a review of 61 cases of DSAP, a total of 41% of the cases had follicular involvement only.14 However, after Pongpudpunth et al. proposed it as a different variety, there is this growing opinion that it should be considered as a new entity and added as another variety of the previously described subtypes of porokeratosis.3,4
We are aware of only 21 cases of porokeratosis with follicular involvement published to date in the international medical literature. Our cases are consistent with the clinical and histopathological characteristics with the previously reported cases.
FundingThis research has not received specific funding from public or private agencies, or nonprofit entities.
Conflicts of interestNone declared.