The incidence of cutaneous melanoma is rising fast, and its prevalence has doubled in the past 3 decades. Detailed local epidemiological information is essential for informing community-based prevention strategies and optimizing hospital resources.
Material and methodsWe included all patients diagnosed with cutaneous melanoma at Hospital Universitario Araba in the Basque province of Álava, Spain, between January 2015 and December 2018. We described clinical and pathologic characteristics and calculated annual incidence rates adjusted to the European standard population.
ResultsA total of 242 new cases of melanoma were diagnosed between 2015 and 2018. The age-standardized annual incidence rose from 12.92 cases per 100 000 population in 2015 to 18.30 cases per 100 000 population in 2018.
ConclusionsThe incidence of melanoma in our area is higher than that reported for Spanish series in 2017 and 2018. Lentigo maligna accounted for a high proportion of cases and was the second largest histologic subgroup.
La incidencia del melanoma cutáneo está aumentando rápidamente y ha duplicado su prevalencia durante las últimas tres décadas. Tener un conocimiento detallado de la epidemiología local es fundamental para el desarrollo de estrategias de prevención comunitaria y optimizar los recursos hospitalarios.
Material y métodosSe incluyeron todos los pacientes diagnosticados de melanoma cutáneo en el Hospital Universitario Araba, en la provincia de Álava del País Vasco, entre enero de 2015 y diciembre de 2018. Se realizó un análisis descriptivo de las variables clínico-patológicas y un análisis de la incidencia ajustado a la población europea.
ResultadosSe incluyeron un total de 242 nuevos casos de melanoma entre 2015 y 2018. La incidencia estandarizada por edad ha aumentado de 12,92 en 2015 a 18,30 casos por 100.000 habitantes y año en 2018.
ConclusionesHemos observado una incidencia de melanoma más elevada que en la publicada en series nacionales en los años 2017 y 2018. Además, existe una gran proporción del subtipo histológico de tipo lentigo maligno, ocupando el segundo subtipo histológico en frecuencia.
Melanoma is the deadliest preventable form of skin cancer.1 Its incidence is increasing rapidly, and its prevalence has doubled over the past 3 decades.2
Melanoma incidence rates in the European population vary considerably between different countries. The highest incidence rates are recorded in Northern and Western Europe, and the lowest in southern Europe.3
Despite having one of the lowest incidence rates in all of Europe, there are few studies of the epidemiology of melanoma in Spain. However, the most comprehensive studies of melanoma incidence have confirmed a progressive increase in recent decades.4–6
Given this increasing incidence, it is important to carry out epidemiological studies of different geographical areas to determine how cases vary in each region. For this reason, we analyzed the incidence of melanoma in the Araba University Hospital (Vitoria-Gasteiz, Basque Country).
Clinical CasesOur analysis included all patients diagnosed with melanoma at the Araba University Hospital between January 1, 2015 (the date on which a prospective melanoma registry was created at this hospital) and December 31, 2018.
Material and MethodsThis retrospective cohort study analyzed data from the melanoma database of a tertiary hospital (Araba University Hospital in Vitoria-Gasteiz, Basque Country, Spain). These data included patient demographics and the clinical and pathological characteristics of the melanoma. Epidemiological data for the population of Álava were obtained from the National Institute of Statistics (INE).7 All patients diagnosed with melanoma between January 2015 and December 2018 at the Araba University Hospital were included in the analysis. In the province of Álava, most melanoma patients are referred to this hospital for management and treatment. However, we estimate that a small percentage of cases were treated in private centers that are not included in the database.
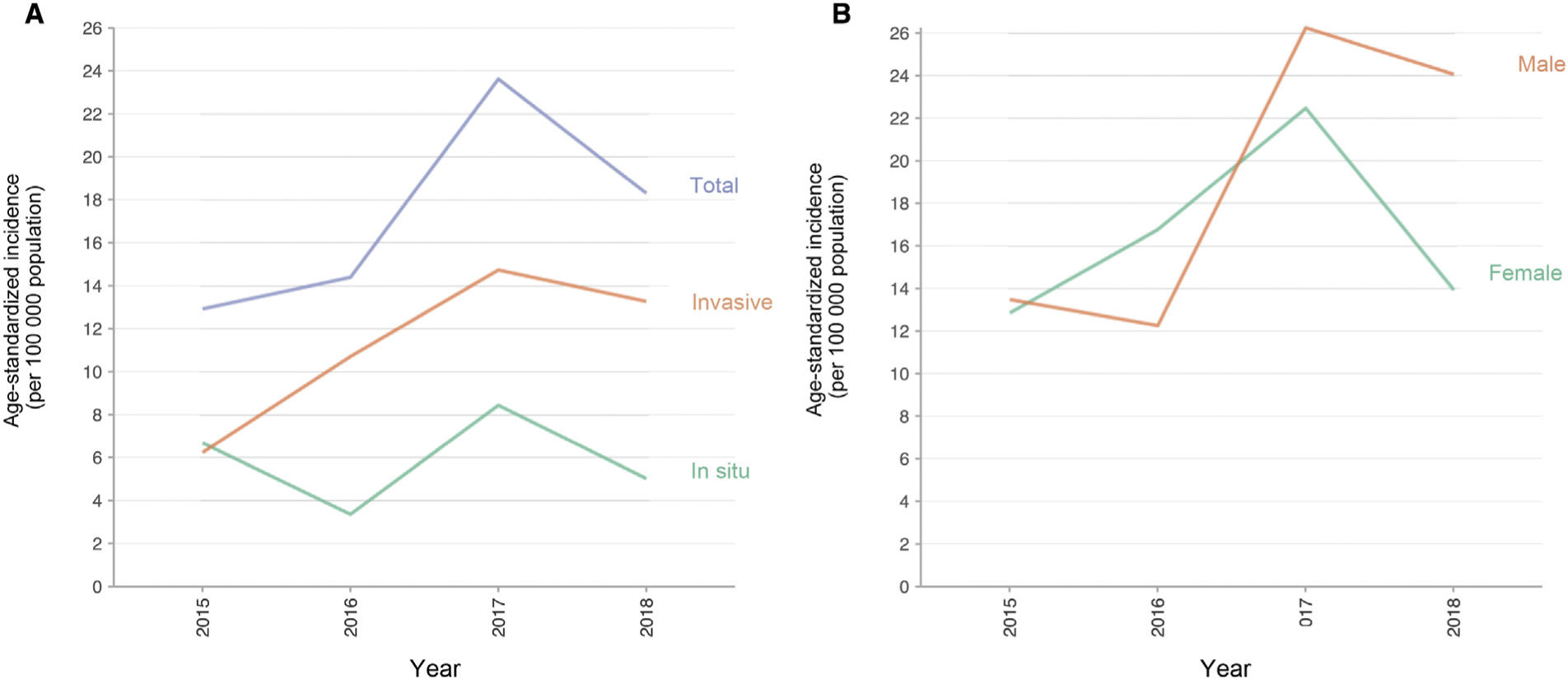
A descriptive analysis was performed and the crude and age-adjusted incidence was calculated relative to the European reference population.8 We analyzed all cases of invasive and in situ cutaneous melanoma in patients of any age (Fig. 1). To analyze differences over time, incidence was compared at 2-year intervals. Categorical variables were compared using Pearson’s χ2 test. Continuous variables were analyzed by comparing the mean and standard deviation using a linear model analysis of variance (ANOVA).
Annual incidence rates were age-standardized to the standard European population.8 The direct method was used to eliminate the confounding effect of age and to ensure valid comparisons between the incidence rates of different countries. The 95% confidence intervals for age-adjusted rates were calculated using the Fay and Feuer method.
Statistical analyses were performed using R and RStudio software. Two-tailed tests were used for all statistical analyses, and P-values <0.05 were considered statistically significant.
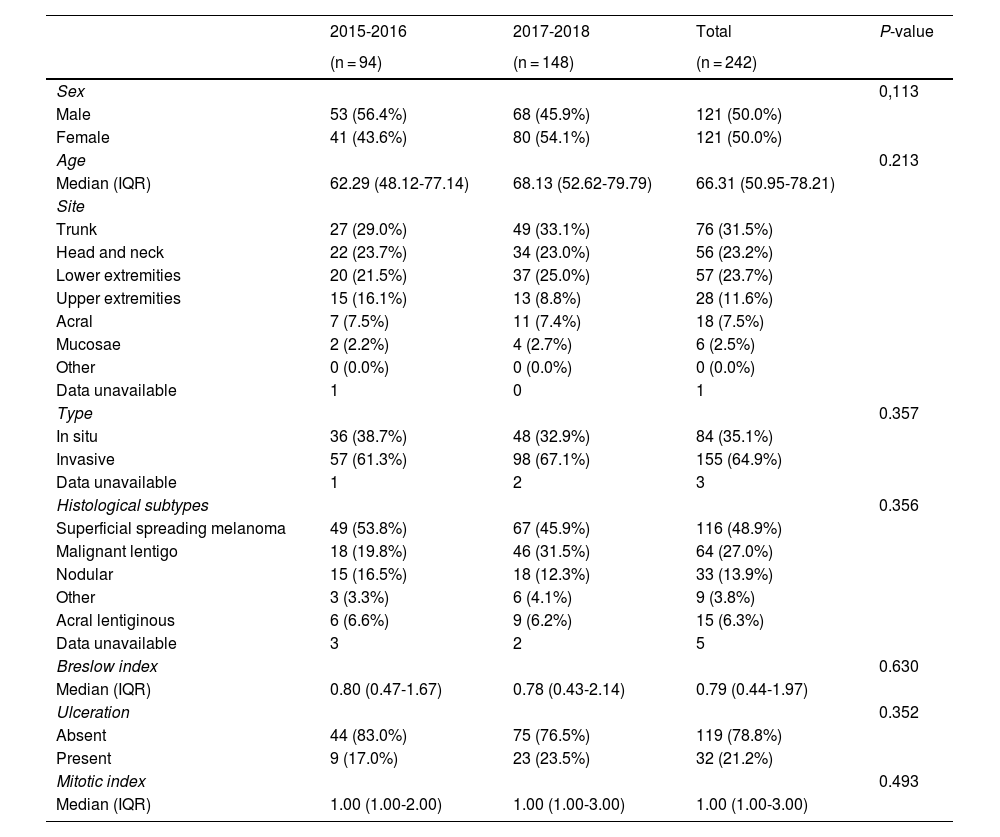
ResultsA total of 242 new cases of melanoma were recorded between 2015 and 2018, and were assigned to one of 2 time periods (2015-2016 or 2017-2018). Of the total melanoma cases, 35.1% were in situ and 64.9% were invasive. No sex-related differences were observed between the 2 periods. The median age for the entire series was 66.1 years. The most frequent site of melanoma was the trunk (31.5%) and the most frequent histological subtype was superficial spreading melanoma (48.9%), followed by lentigo maligna (27.0%). The median Breslow index was 0.79 mm and ulceration was present in 21.2% of invasive melanomas (Table 1).
Baseline Characteristics of a Patient Cohort Diagnosed with Melanoma Between 2015 and 2018.
| 2015-2016 | 2017-2018 | Total | P-value | |
|---|---|---|---|---|
| (n = 94) | (n = 148) | (n = 242) | ||
| Sex | 0,113 | |||
| Male | 53 (56.4%) | 68 (45.9%) | 121 (50.0%) | |
| Female | 41 (43.6%) | 80 (54.1%) | 121 (50.0%) | |
| Age | 0.213 | |||
| Median (IQR) | 62.29 (48.12-77.14) | 68.13 (52.62-79.79) | 66.31 (50.95-78.21) | |
| Site | ||||
| Trunk | 27 (29.0%) | 49 (33.1%) | 76 (31.5%) | |
| Head and neck | 22 (23.7%) | 34 (23.0%) | 56 (23.2%) | |
| Lower extremities | 20 (21.5%) | 37 (25.0%) | 57 (23.7%) | |
| Upper extremities | 15 (16.1%) | 13 (8.8%) | 28 (11.6%) | |
| Acral | 7 (7.5%) | 11 (7.4%) | 18 (7.5%) | |
| Mucosae | 2 (2.2%) | 4 (2.7%) | 6 (2.5%) | |
| Other | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | |
| Data unavailable | 1 | 0 | 1 | |
| Type | 0.357 | |||
| In situ | 36 (38.7%) | 48 (32.9%) | 84 (35.1%) | |
| Invasive | 57 (61.3%) | 98 (67.1%) | 155 (64.9%) | |
| Data unavailable | 1 | 2 | 3 | |
| Histological subtypes | 0.356 | |||
| Superficial spreading melanoma | 49 (53.8%) | 67 (45.9%) | 116 (48.9%) | |
| Malignant lentigo | 18 (19.8%) | 46 (31.5%) | 64 (27.0%) | |
| Nodular | 15 (16.5%) | 18 (12.3%) | 33 (13.9%) | |
| Other | 3 (3.3%) | 6 (4.1%) | 9 (3.8%) | |
| Acral lentiginous | 6 (6.6%) | 9 (6.2%) | 15 (6.3%) | |
| Data unavailable | 3 | 2 | 5 | |
| Breslow index | 0.630 | |||
| Median (IQR) | 0.80 (0.47-1.67) | 0.78 (0.43-2.14) | 0.79 (0.44-1.97) | |
| Ulceration | 0.352 | |||
| Absent | 44 (83.0%) | 75 (76.5%) | 119 (78.8%) | |
| Present | 9 (17.0%) | 23 (23.5%) | 32 (21.2%) | |
| Mitotic index | 0.493 | |||
| Median (IQR) | 1.00 (1.00-2.00) | 1.00 (1.00-3.00) | 1.00 (1.00-3.00) |
Breslow index, ulceration, and mitotic index were only evaluated for invasive melanomas.
Abbreviation: IQR, interquartile range.
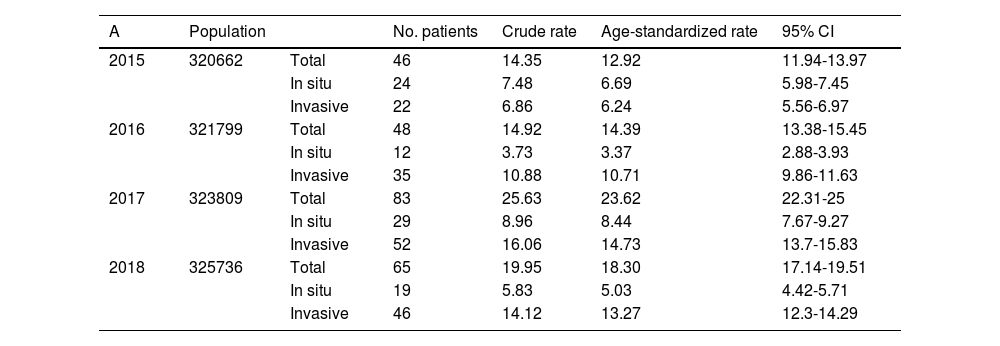
The age-standardized incidence is summarized in Table 2A. The age-standardized incidence of invasive and in situ melanoma per 100000 inhabitants per year increased from 12.92 in 2015 (95% CI, 11.94-13.97) to 18.30 in 2018 (95% CI, 17.14-19.51). This effect was largely accounted for by the invasive melanoma group, in which incidence increased from 6.24 (95% CI, 5.56-6.97) in 2015 to 13.27 (95% CI, 12.3-14.29) in 2018. After adjusting for age and stratifying by sex (Table 2B), incidence was higher in men than women, particularly in 2018, at 24.06 (95% CI, 22.24-25.99) in men versus 13.93 (95% CI, 12.51-15.46) in women.
Age-Adjusted Melanoma Incidence Rates. A, Incidence of Total, in Situ, and Invasive Melanoma in the Province of Álava. B, Incidence of Melanoma in the Province of Álava, Stratified by Sex.
| A | Population | No. patients | Crude rate | Age-standardized rate | 95% CI | |
|---|---|---|---|---|---|---|
| 2015 | 320662 | Total | 46 | 14.35 | 12.92 | 11.94-13.97 |
| In situ | 24 | 7.48 | 6.69 | 5.98-7.45 | ||
| Invasive | 22 | 6.86 | 6.24 | 5.56-6.97 | ||
| 2016 | 321799 | Total | 48 | 14.92 | 14.39 | 13.38-15.45 |
| In situ | 12 | 3.73 | 3.37 | 2.88-3.93 | ||
| Invasive | 35 | 10.88 | 10.71 | 9.86-11.63 | ||
| 2017 | 323809 | Total | 83 | 25.63 | 23.62 | 22.31-25 |
| In situ | 29 | 8.96 | 8.44 | 7.67-9.27 | ||
| Invasive | 52 | 16.06 | 14.73 | 13.7-15.83 | ||
| 2018 | 325736 | Total | 65 | 19.95 | 18.30 | 17.14-19.51 |
| In situ | 19 | 5.83 | 5.03 | 4.42-5.71 | ||
| Invasive | 46 | 14.12 | 13.27 | 12.3-14.29 |
| B | Sex | Population | No. patients | Crude rate | Age-standardized rate | 95% CI |
|---|---|---|---|---|---|---|
| 2015 | Female | 162560 | 24 | 14.76 | 12.85 | 11.46-14.36 |
| Male | 158103 | 22 | 13.91 | 13.48 | 12.11-14.96 | |
| 2016 | Female | 163432 | 29 | 17.74 | 16.76 | 15.24-18.41 |
| Male | 158372 | 19 | 12.00 | 12.26 | 10.99-13.64 | |
| 2017 | Female | 164625 | 42 | 25.51 | 22.47 | 20.64-24.42 |
| Male | 159185 | 41 | 25.76 | 26.25 | 24.37-28.23 | |
| 2018 | Female | 165943 | 26 | 15.67 | 13.93 | 12.51-15.46 |
| Male | 159794 | 39 | 24.41 | 24.06 | 22.24-25.99 |
Abbreviation: CI, confidence interval.
This study describes the population of melanoma patients within the catchment area of the Araba University Hospital. We analyzed all cases of de novo melanoma diagnosed during the study period. The findings reveal a high total incidence (in situ and invasive melanoma) in the last 2 years studied (23.62 and 18.30 cases per 100 000 inhabitants per year in 2017 and 2018, respectively). Analysis of invasive melanoma cases shows that the incidence was slightly higher than that observed in other areas of Spain.6 Similar findings were reported in a study conducted in another Spanish region in which up to 30% of patients were non-Spanish nationals of central and northern European origin.9 This may explain why the incidence of melanoma is more similar to that of European Nordic countries.10 Another possible explanation for the higher incidence of melanoma in Álava is that the study population is relatively closed: most melanomas are referred to the hospital and the number of annual cases can be adequately accounted for. Finally, other regions of Spain, such as Barcelona, have significant African, Asian, and South American immigrant communities, which may dilute the incidence of melanoma.6 This phenomenon is not observed in the province of Álava, which has much lower rates of immigration.11
During the period 2015-2016 the incidence of invasive melanoma was lower than that observed in the rest of Spain (6.24 and 10.71 cases per 100 000 inhabitants per year in 2015 and 2016, respectively). This difference may be due to the loss of patients during the first time period due to the retrospective nature of the recruitment process.
The cancer registry of the Spanish Basque Country only contains data on incidence in the male population from 1986 to 2009. These data reveal an incidence of 3 and 8 cases per 100 000 inhabitants per year in 1986 and 2009, respectively. The present findings update this information and confirm a continued increase in the incidence of melanoma.12
The descriptive findings for our cohort are all in line with those previously reported.6 The median age at presentation was 66.31 years and the main site of melanoma was the trunk (31.5%), followed by the lower limbs (23.7%) and the head and neck (23.2%). The most frequent histological subtype was superficial spreading melanoma (48.9%) followed by lentigo maligna melanoma (27.0%). Podlipnik et al.6 have emphasized the growing importance of lentigo maligna melanoma, the incidence of which has increased from 13.9% to 22.6% in Catalonia over the last 9 years. This increase could be related to accumulated sun exposure throughout life, but may also reflect the increased sensitivity of methods for melanoma diagnosis introduced in the last decade, such as dermoscopy, which allows earlier detection of these lesions.
In our cohort the proportion of invasive melanomas was higher than that of in situ melanomas, with a ratio of approximately 2:1, in line with the proportions reported in other European cohorts.13
Stratification by sex revealed that the incidence of melanoma was higher in men than in women in all years except 2016. These data are also in agreement with the incidence observed in other European countries.10
The main limitation of this study is the retrospective inclusion of patients diagnosed with melanoma, which may have led to exclusion of melanoma patients. Furthermore, in the province of Álava there is only one private dermatologist for every 100 000 inhabitants. This implies that most melanomas are diagnosed within the public health system, although we do not have definitive evidence to support this claim.
We conclude that the population with melanoma in Álava has demographic characteristics similar to those of the rest of Spain. However, we observed a slightly higher incidence of invasive melanoma in the last 2 years, possibly due to the fact that the studied population includes a low proportion of immigrants and the vast majority of cases are treated via the public health system. Understanding the epidemiology of melanoma in the Spanish population has important implications for clinical practice, allowing us to better identify patients who are predisposed to this disease and thus develop primary and secondary strategies for the prevention and early detection of melanoma. We did not identify any external factor that could justify an increase in the incidence of melanoma in this population.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Rosés-Gibert P, Podlipnik S, de la Torre Gomar FJ, Saenz Aguirre A, Gimeno Castillo J, González Pérez R, et al. Estudio descriptivo de los pacientes diagnosticados de melanoma en la provincia de Álava (País Vasco) entre los años 2015 y 2018. Actas Dermosifiliogr. 2022;113:178–182.