Patients with psoriasis often have comorbidities, including other immune-mediated inflammatory diseases (IMIDs), and cardiovascular risk factors. In this article we describe the baseline prevalence of comorbidities—including other IMIDs—in a cohort of patients with psoriasis.
Patients and methodsAQUILES was a prospective observational multicenter study of 3 patient cohorts (patients with psoriasis, spondyloarthritis, or inflammatory bowel disease) undertaken to investigate the prevalence of comorbidities, including other IMIDs, in these settings. The psoriasis cohort comprised patients aged at least 18 years who were seen in hospital dermatology clinics. A predefined protocol was used to collect demographic and clinical data.
ResultsThe study enrolled 528 patients with psoriasis (60.2% men and 39.8% women). Mean age was 46.7 years; 89.8% of the participants had plaque psoriasis, and the median (interquartile range) Psoriasis Area Severity Index was 3.2 (1.5-7.4). Comorbid IMIDs were present in 82 of the patients (15.5%; 95% CI, 12.7%-18.9%). Spondyloarthritis was observed in 14% of patients (95% CI, 11.3%-17.2%), mostly in the form of psoriatic arthritis, for which the overall prevalence was 13.1% (95% CI, 10.5%-16.2%). Inflammatory bowel disease was present in 1.3% (95% CI, 0.6%-2.7%) and uveitis in 0.2% (95% CI, 0.1%-1.4%). Psoriatic arthritis was associated with male sex (odds ratio, 1.75 [0.98-2.98]) and a disease duration of over 8 years (odds ratio, 4.17 [1.84-9.44] vs a duration of < 4 years). In 73.1%, at least 1 cardiovascular risk factor was identified: smoking (40.5%), obesity (26.0%), dyslipidemia (24.8%), hypertension (24.3%), and diabetes mellitus (12.3%).
ConclusionIn patients with psoriasis the prevalence of other IMIDs was 15.5%, a level slightly higher than that found in the general population. Nearly three-quarters of these patients had at least 1 cardiovascular risk factor.
Los pacientes con psoriasis presentan con frecuencia comorbilidades, incluyendo otras enfermedades inflamatorias mediadas por inmunidad (EIMI) y factores de riesgo cardiovascular (FRCV). El objetivo de este trabajo es describir la prevalencia basal de otras EIMI y comorbilidades en una cohorte de pacientes con psoriasis.
Pacientes y métodosAQUILES es un estudio observacional prospectivo multicéntrico de 3 cohortes de pacientes (psoriasis, espondiloartritis y enfermedad inflamatoria intestinal [EII]), para evaluar la coexistencia de EIMI y otras comorbilidades. En la cohorte con psoriasis se incluyeron pacientes ≥18 años atendidos en consultas hospitalarias de dermatología. Se recogió información sobre datos demográficos y clínicos de acuerdo a un protocolo preespecificado.
ResultadosSe incluyeron 528 pacientes con psoriasis (edad media: 46,7 años; 60,2% hombres; 39,8% mujeres; 89,8% psoriasis en placas; mediana de PASI 3,2 [1,5-7,4]). Presentaron otra EIMI 82 pacientes (15,5% [IC 95%: 12,7-18,9]). El 14,0% (IC 95%: 11,3-17,2) presentó espondiloartritis (la mayoría de estos artritis psoriásica [prevalencia 13,1%, IC 95%: 10,5-16,2), el 1,3% EII (IC 95%: 0,6-2,7) y el 0,2% uveítis (IC 95%: 0,1-1,4). La presencia de artritis psoriásica se asoció al sexo masculino (OR: 1,75 [0,98-2,98]) y a la duración de la psoriasis >8 años (OR: 4,17; [1,84-9,44]) respecto a <4 años. El 73,1% presentó al menos un FRCV: tabaquismo (40,5%); obesidad (26,0%); dislipidemia (24,8%); hipertensión arterial (24,3%) y diabetes mellitus (12,3%).
ConclusiónLos pacientes con psoriasis presentaron una prevalencia del 15,5% de otras EIMI, discretamente superior a la de población general. Casi tres cuartas partes tuvieron al menos un FRCV.
The highly varied clinical manifestations of psoriasis range from small, reddish, scaly plaques to lesions that can cover a very large area of the body.1 The prevalence varies, as psoriasis is affected by climate, genetic susceptibility, and exposure to environmental antigens, among other variables.2,3 In Europe rates range from 1% to 6.5%4–6; in Spain an incidence of 14 cases per 10000 person-years has been described,4 and over half the cases are diagnosed before the age of 30 years.6
Psoriasis is categorized as an immune-mediated inflammatory disease (IMID) and cytokine dysregulation has been implicated in its pathogenesis.7–9 Both genetic and environmental factors have been shown to play roles in triggering these diseases,10 and an abnormal immune response is central to the pathogenesis of IMIDs such as psoriasis, inflammatory bowel disease (IBD), and spondyloarthritis.11,12 Patients who have any IMID are at higher risk of developing another one.12
Psoriasis tends to be associated with other conditions, among them cardiovascular diseases; obesity, metabolic syndrome, and other cardiovascular risk factors (CVRFs); tumor; fatty liver disease; and anxiety and depression.13–19
Although the exact mechanism underlying the association between psoriasis and cardiovascular disease are unknown, the humoral or cellular inflammatory mediators implicated in the development of atherosclerosis may be involved.20 The inflammatory process in psoriasis seems to be related to changes in interleukin levels and elevated tumor necrosis factor and C-reactive protein levels—signs that are often seen in patients with atherosclerosis.21–23
The AQUILES study was a 2-year prospective, noninterventional, multicenter observation of 3 independent cohorts of patients with psoriasis, spondyloarthritis, and IBD. The main purpose of the AQUILES study as a whole was to determine the prevalence of these IMIDs and the frequency of the clinical features in these cohorts. Its secondary aims were to determine 1) the incidence of the different IMIDs over the 2-year period, and 2) the prevalence and incidence rates of other concomitant diseases. The purpose of the present study was to determine the baseline characteristics and prevalence of IMIDs and other comorbidities in the cohort of patients with psoriasis enrolled from hospital dermatology clinics in Spain; CVRFs were of particular interest.
Material and MethodsStudy DesignThe AQUILES project was designed to follow 3 independent cohorts of patients with a principal diagnosis of psoriasis, spondyloarthritis, or IBD at the time of enrollment. Fifteen Spanish hospitals with departments of dermatology, rheumatology, and gastroenterology participated. All were invited to enroll patients aged 18 years or older who were diagnosed with one of the following IMIDs: psoriasis, spondyloarthritis (including ankylosing spondylitis, psoriatic arthritis, nonspecific spondylitis, or other forms), or an IBD. The patients were followed by the same physician for 2 years after enrollment.
Patient Selection and Data CollectionThe dermatology cohort included patients aged 18 years or older with a prior diagnosis of psoriasis or newly diagnosed with psoriasis at an initial dermatology visit. A dermatologist made the diagnosis in all cases. Patients were excluded if the researchers thought any circumstance might prevent completion of 2 years of follow-up. The protocol was approved by the ethics committees of the participating hospitals and the study was conducted in keeping with good clinical practice guidelines.24
Patients could be enrolled either consecutively or by random sampling. Random sampling could be done on records for patients previously diagnosed with psoriasis who were seen in the 6 months before the study began. Consecutive enrollment could be accomplished by inviting all eligible patients as they were seen, provided they were not already enrolled in other studies. Newly diagnosed patients were also eligible for consecutive enrollment. In fact, the entire dermatology cohort was enrolled consecutively in the following hospitals: 12 de Octubre (Madrid), Carlos Haya (Málaga), Reina Sofía (Córdoba), Gregorio Marañón (Madrid), General de Valencia (Valencia), del Mar (Barcelona), Santa Creu i Sant Pau (Barcelona), Donostia (San Sebastián), Marqués de Valdecilla (Santander), Príncipe de Asturias (Madrid), Virgen de la Arrixaca (Murcia), La Princesa (Madrid), and Infanta Sofía (Madrid).
The enrollment process took place from March 2008 through December 2010. The following information was gathered from patient records: type of psoriasis, location, severity according to the Psoriasis Area and Severity Index, family history of psoriasis, and comorbidities. The concomitant diseases of interest were mainly other diseases of the skin or cardiovascular system (and CVRFs), as well as rheumatic, respiratory, gastrointestinal, liver, and psychiatric diseases. The patients were weighed and their height was measured for this study, but blood pressure was not checked and no laboratory or imaging studies were ordered.
Statistical AnalysisSample size was calculated based on the primary objective, to determine the prevalence of IMIDs in each cohort; the same criteria were used for each cohort. Therefore, assuming a 3% prevalence of IMIDs in the psoriasis cohort it was calculated that a sample of 1075 patients should be enrolled for a 95% CI and 1% precision. Fewer patients than expected could be recruited, so the final sample of 528 patients provided a level of precision of 3% for the observed prevalence.
Continuous variables were described as mean (SD) or median (interquartile range). Categorical variables were reported as absolute frequency and percentage. IMID prevalence was analyzed for clinical and demographic subgroups of the cohort. Differences were compared with the ¿2 test. The characteristics of patients with and without a concomitant IMID were also compared, with the t test for means in independent groups or the ¿2 test for categorical variables. Later a logistic regression model was constructed to identify independent demographic and clinical variables associated with the presence of IMIDs; the results are reported as adjusted odds ratios (ORs) and their 95% CIs. In all tests, the null hypothesis was rejected when the ¿ error was less than .05. SPSS software (version 18.0) was used for all statistics.
ResultsPatient CharacteristicsBetween March 2008 and December 2010, the participating hospitals enrolled 528 patients with a mean age of 46.7 (15.3) years; 60.2% were men and 39.8% women. Most of the enrolled patients had a prior diagnosis of psoriasis (83.5%). The median duration of disease was 15 (7–25) years and 16.5% were newly diagnosed. A family history of psoriasis was recorded for 43.0% of the patients. The median Psoriasis Area and Severity Index at baseline was 3.2 (1.5–7.4), and 89.9% had plaque psoriasis, which was the only diagnosis in 86.0% of the cases and was combined with some other type (guttate, inverse, pustular, or erythrodermic) in 3.8% (Table 1). The main sites of involvement were the elbows (79.0%), the knees (67.2%), the trunk (59.7%), and the scalp (55.5%). The clinical features in men and women (Table 1) were similar except that men had a higher prevalence of plaque psoriasis, while women had a higher prevalence of guttate psoriasis. An inframammary location was more prevalent in women and nail involvement was more common in men.
Characteristics of Patients in the Psoriasis Cohort of the AQUILES Study.
| Total (n=528) | Men (n=317) | Women (n=210) | Pa | |
|---|---|---|---|---|
| Diagnosis | ||||
| New diagnosis | 16.5% | 15.8% | 17.6% | NS |
| Prior diagnosis | 83.5% | 84.2% | 82.4% | |
| Time since onset | ||||
| <4y | 28.2% | 26.6% | 30.3% | NS |
| 4–8 y | 13.3% | 15.2% | 10.6% | |
| >8y | 58.5% | 58.2% | 59.1% | |
| Family history of psoriasis | 43.0% | 40.8% | 46.0% | NS |
| PASI, median (IQR) | 3.2 (1.5–7.4) | 3.6 (1.5–7.7) | 2.9 (1.4–7.1) | NS |
| Type of psoriasis | ||||
| Plaque, or psoriasis vulgaris (including mixed forms) | 89.8% | 92.7% | 85.2% | .005 |
| Guttate | 10.2% | 6.9% | 15.3% | .002 |
| Inverse | 1.9% | 1.9% | 1.9% | NS |
| Pustular | 1.1% | 1.3% | 1.0% | NS |
| Erythrodermic | 0.8% | 1.3% | 0.0% | NS |
| Location of lesions | ||||
| Elbows | 79.0% | 79.8% | 78.1% | NS |
| Scalp | 55.5% | 52.4% | 60.5% | NS (.067) |
| Knees | 67.2% | 70.0% | 63.3% | NS |
| Sacrum | 42.6% | 42.6% | 42.9% | NS |
| Trunk | 59.7% | 57.4% | 63.3% | NS |
| Nails | 21.0% | 24.3% | 16.2% | .026 |
| Submammary fold | 6.6% | 3.5% | 11.4% | <.001 |
Abbreviations: IQR, interquartile range; PASI, Psoriasis Area and Severity Index.
Comorbidity was observed in 15.5% (95% CI, 12.7%–18.9%; n=82). The distribution was as follows: 74 patients (14.0%; 95% CI, 11.3%–17.2%) had spondyloarthritis, and 69 (13.1%; 95% CI, 10.5%–16.2%) also had psoriatic arthritis. Two of these patients (0.4%; 95% CI, 0.1%–1.4%) also had ankylosing spondylitis, 1 (0.2%; 95% CI, 0.0%–1.0%) had enteropathic arthritis, and 2 (0.4%; 95% CI, 0.1%–1.4%) had nonspecific spondyloarthritis. Of the patients with psoriatic arthritis, 82.5% had been diagnosed a median of 12 years after psoriasis was first detected, and 6.3% were diagnosed with psoriatic arthritis before psoriasis itself was diagnosed (Table 2). Seven patients (1.3%; 95% CI, 0.6%–2.7%) had an IBD (4, ulcerative colitis [0.8%; 95% CI, 0.3%–1.9%]; 1, Crohn disease [0.2%; 95% CI, 0.0%–1.0%]; and 2, indeterminate colitis [0.4%; 95% CI, 0.1%–1.4%]). No pattern in the timing of diagnosis could be discerned (Table 2). Two patients (0.4%; 95% CI, 0.1%–1.4%) had uveitis. One patient had concomitant psoriasis, psoriatic arthritis, and ulcerative colitis.
Timing of Psoriatic Arthritis and IBD Diagnoses in Comparison With Psoriasis a
| IMID Diagnosis Compared to Psoriasis Diagnosis | |||
|---|---|---|---|
| IMID Diagnosed First, n(%) | IMID Diagnosed in Same Year, n(%) | IMID Diagnosed Later, n(%) | |
| Psoriatic arthritis, n=63 | 4 (6.3%)–3.0(–4to–1.3)y | 7 (11.1%) | 52 (82.5%)+12.0(6to24)y |
| IBD, n=7 | 3 (42.9%)–5.0(–10to–2)y | 1 (14.3%) | 3 (42.9%)+10.0(4to40)y |
Abbreviations: IBD, inflammatory bowel disease; IMID, immune-mediated inflammatory disease.
Prevalence data are number of cases and percentage of totals for each IMID. Time elapsing between diagnoses, on the line below, is expressed as median (interquartile range) whenever the group includes ≥4cases. The time of diagnosis was unknown for 6 patients with psoriatic arthritis. All patients with an IBD are grouped together. Other concomitant IMIDs are not shown because there were fewer than 2 cases.
Similar percentages of men and women in the cohort had psoriatic arthritis (15.1% of men and 10.0% of women; P=.087). The percentages were also similar in patients with or without a family history of psoriasis (14.9% vs 10.5%, P=.208). However, a significantly higher prevalence of psoriatic arthritis was seen in patients with a prior diagnosis of psoriasis than in patients who were newly diagnosed (15.0% vs 3.4%, P=.004). Psoriatic arthritis was also more prevalent in patients in whom psoriasis had been diagnosed more than 8 years earlier (18.9%) than in those with a duration of disease of less than 4 years or between 4 and 8 years (4.7% and 5.7%, respectively; P<.05, both comparisons). No significant differences in the prevalence rates for other IMIDs were detected between subgroups.
Multivariate Analysis: Variables Associated With IMIDsTo assess the relationships between the presence of other IMIDs in patients with psoriasis and patient characteristics, a multiple regression model was constructed with the following variables: age, sex, diagnosis (prior or de novo), time since onset of symptoms (<4 years, 4 to <8 years, or ≥8 years), and a family history of psoriasis. Of particular interest was any association between IBD and psoriatic arthritis. No patient variable was correlated with the presence of an IBD, but independent variables associated with the presence of psoriatic arthritis were male sex (OR, 1.75; 95% CI, 0.98–2.98; P=.058) and more than 8 years since onset of psoriasis symptoms (OR, 4.17; 95% CI, 1.84–9.44, P<.001 vs patients who reported presentation of symptoms <4 years earlier). Table 3 shows the characteristics of patients with or without psoriatic arthritis.
Characteristics of Psoriasis Patients With or Without Psoriatic Arthritis.
| With Psoriatic Arthritis (n=69) | Without Psoriatic Arthritis (n=459) | Pa | |
|---|---|---|---|
| Mean (SD) age, y | 49.0 (12.2) | 46.3 (15.8) | NS (.084) |
| Sex | NS (.093) | ||
| Men | 69.6% | 58.9% | |
| Women | 30.4% | 41.1% | |
| Diagnosis | .004 | ||
| New diagnosis | 4.3% | 18.3% | |
| Prior diagnosis | 95.7% | 81.7% | |
| Time since onset | <.001 | ||
| <4y | 10.1% | 30.8% | |
| 4–8 y | 5.8% | 14.6% | |
| >8y | 84.1% | 54.5% | |
| Family history of psoriasis | 50.0% | 41.9% | NS |
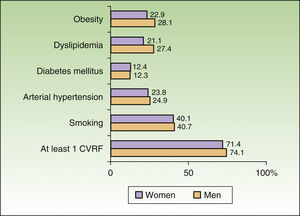
The most frequent comorbidities were depression (12.9%), seborrheic dermatitis (8.0%), asthma (4.7%), chronic liver disease (4.2%), and CVRFs. At least 1 CVRF was identified in 73.1% of the patients (38.1% had 1, 19.7% had 2, 11.7% had 3, 3.0% had 4, and 0.6% had 5). Smoking was the most common CVRF (40.5%; 95% CI, 36.4%–44.8%), followed by obesity (26.0%; 95% CI, 22.4%–30.0%), dyslipidemia (24.8%; 95% CI, 21.3%–28.7%), arterial hypertension (24.3%; 95% CI, 21.0%–28.3%), and diabetes mellitus (12.3%; 95% CI, 9.8%–15.4%). The rates were statistically similar in men and women, although a slight nonsignificant trend toward a higher prevalence of obesity and dyslipidemia was observed in men (Fig. 1). Obese patients also had a higher prevalence of other CVRFs (Table 4). The rates for all risk factors except smoking increased with age; the prevalence of smoking, on the other hand, decreased with age for both men and women (Table 5).
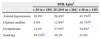
Prevalence of Cardiovascular Risk Factors Stratified by BMI.
| BMI, kg/m2 | |||
|---|---|---|---|
| <25 (n=183) | 25–29.9 (n=201) | ≥30 (n=135) | |
| Arterial hypertension | 10.9% | 24.4%a | 43.7%a,b |
| Diabetes mellitus | 6.0% | 12.9%a | 20.7%a,b |
| Dyslipidemia | 14.2% | 27.9%a | 34.8%a |
| Smoking | 50.3%b,c | 38.3% | 31.9% |
Abbreviation: BMI, body mass index.
Prevalence of Cardiovascular Risk Factors by Age Range and Sex.
| Age Range, y | ||||
|---|---|---|---|---|
| <45 (n=245) | 45–54 (n=110) | 55–64 (n=88) | ≥65 (n=77) | |
| Entire cohort | ||||
| Obesity | 18.4% | 25.7% | 34.5% | 40.3% |
| Arterial hypertension | 4.1% | 23.6% | 44.3% | 68.8% |
| Diabetes mellitus | 2.0% | 11.8% | 25.0% | 31.2% |
| Dyslipidemia | 14.7% | 23.6% | 38.6% | 44.2% |
| Smoking | 51.0% | 39.1% | 29.5% | 22.1% |
| Men | <45(n=144) | 45–54(n=71) | 55–64(n=52) | ≥65(n=47) |
| Obesitya | 22.9% | 25.4% | 34.6% | 40.4% |
| Arterial hypertension | 3.5% | 26.8% | 46.2% | 66.0% |
| Diabetes mellitus | 2.8% | 11.3% | 25.0% | 29.8% |
| Dyslipidemiab | 20.1% | 26.8% | 38.5% | 40.4% |
| Smokingc | 47.2% | 38.0% | 34.6% | 31.9% |
| Women | <45(n=101) | 45–54(n=38) | 55–64(n=36) | ≥65(n=30) |
| Obesity | 12.1% | 27.0% | 34.3% | 40.0% |
| Arterial hypertension | 5.0% | 18.4% | 41.7% | 73.3% |
| Diabetes mellitus | 1.0% | 13.2% | 25.0% | 33.3% |
| Dyslipidemia | 6.9% | 18.4% | 38.9% | 50.0% |
| Smoking | 56.4% | 39.5% | 22.2% | 6.7% |
The ¿2 test for linear trend was used for all comparisons; P<.001 in all cases except the following:
The results of this study show that a moderate percentage of patients with psoriasis also had another IMID, predominantly spondyloarthritis (14.0%) and within that group, the most common subtype was psoriatic arthritis (13.1% of the whole sample). Other IMIDs, such as IBD (1.3%) and uveitis (0.2%) were much less prevalent. However, other types of comorbid conditions, particularly CVRFs, were very common.
Psoriatic arthritis is the most frequent IMID in psoriasis patients. One systematic review of the literature found that psoriatic arthritis can affect 24% of psoriasis patients.25 The AQUILES study findings are very similar to those reported by García-Díez et al.26 after a cross-sectional study that evaluated the characteristics of patients with moderate or severe psoriasis in Spain and Portugal. The authors found that 13% of these patients had psoriatic arthritis. Although psoriatic arthritis usually develops after psoriasis, a small percentage of patients may develop it earlier or simultaneously (6% and 11%, respectively, in our study). It is therefore essential to inspect the skin of patients with arthritis. Our findings for IBD are consistent with those of other studies, which have reported relatively low prevalence rates of IBD in psoriasis patients; however, the rates are higher than in the general population, where ulcerative colitis and Crohn disease occur in around 0.3% and 0.1% to 0.2%, respectively.27,28
Nearly three quarters of the concomitant conditions found were some type of CVRF, and obese patients had higher rates of other CVRFs than normal-weight patients. These findings should be interpreted in the light of the relatively young average age of this cohort (46.7 years), in which there was a higher prevalence of CVRFs than in the 2006 national survey.29 Like our study, the 2006 survey was based on prior diagnoses and required neither blood pressure measurement or laboratory testing. Thus, while both studies suggest that the CVRF prevalence is higher in patients with psoriasis than it is in the general Spanish population, they may both have underestimated the prevalence since they were similarly based on reviews of patient records, without additional diagnostic testing. The DARIOS study (on dyslipidemia, atherosclerotic risk, elevated C-reactive protein, and inflammatory and oxidative status in Spain), which sought to determine the prevalence of CVRFs in the population between the ages of 35 and 74 years in 10 Spanish autonomous communities, did include the measurement of blood pressure, along with weight, height, and blood sugar and lipid levels.30 The CVRF rates were similar in the DARIOS study and ours, which both saw higher rates than the national survey of 2006.
We would like to highlight the relevance of our findings for dermatologists, in the context of the Spanish national survey of 2006 and the DARIOS study. Patients with psoriasis have a higher CVRF prevalence than might be expected for their age or sex. Many of these patients are young and may never have had their blood pressure taken or cardiovascular risk evaluated before they consult a dermatologist. Thus, the dermatologist may play a key role in detecting CVRFs simply by checking blood pressure and ordering basic blood tests. A recent study of 368 patients with psoriasis found that the dermatologist had detected at least 1 previously undiagnosed CVRF in 27% of these patients by simply taking these two steps.31 It is also important to bear in mind that some psoriasis treatments can affect CVRFs,32,33 and that obesity can alter the response to biologics because the effects of drugs administered at fixed doses may be attenuated in heavier patients.34
We must underline the limitations of the AQUILES study. As mentioned, data were collected by reviewing clinical records, and no blood pressure or other diagnostic tests were done; therefore the prevalence of comorbidities such as hypertension, high cholesterol levels, and diabetes may have been underestimated. Second, the sample studied was smaller than targeted, affecting the precision of the prevalence rates calculated; the sample size finally enrolled allows us to assume a precision of 3%. Third, as the patients enrolled were found through hospital clinics, the data cannot be extrapolated to the general population of patients with psoriasis. Two additional limitations affecting the interpretation of the data should also be taken into consideration. One is that the hospital clinics did not use a randomized patient selection method but rather enrolled participants consecutively, an approach that favors the inclusion of more seriously ill patients or those with more comorbidities, as such individuals are the ones who consult hospital specialists for chronic diseases. The second is that the presence of a chronic disease such as psoriasis may hasten the diagnosis of other diseases, such as axial spondyloarthritis, which is usually detected 6 to 9 years after onset of symptoms in the general population35; consulting a dermatologist can contribute to the likelihood of early diagnosis, since psoriasis usually develops at an earlier age. Within the constraints of these limitations, the AQUILES study provides a useful portrait of a typical hospital psoriasis caseload in dermatology, where there are comorbidities the specialist can help to identify early.
Based on our findings, we conclude that the prevalence of other IMIDs is moderate in patients seen for psoriasis in hospital dermatology clinics, and the main concomitant IMID is psoriatic arthritis. The prevalence of IBD is low; although it is higher than in the general population27,28 few cases are involved. The prevalence of CVRFs, on the other hand, is high. The dermatologist should, therefore, take a more active role in detecting comorbidity and CVRFs, since psoriasis patients are usually young and no other condition has been diagnosed. In fact, these patients have often never been evaluated for other possible diseases prior to their dermatologic diagnosis.
Ethical DisclosuresProtection of Human and Animal SubjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of DataThe authors declare that they followed their hospitals’ regulations regarding the publication of patient information and that written informed consent for voluntary participation was obtained for all patients.
Right to Privacy and Informed ConsentThe authors declare that no private patient data are disclosed in this article.
FundingThe AQUILES study was funded by Merck Sharp & Dohme, Spain.
Conflicts of InterestCristina Sancho, Berta Juliá, and Luis Cea-Calvo are full-time employees of Merck Sharp & Dohme, Spain. The authors of this manuscript also took part in the study as investigators, and they or the institution they were affiliated with received fees for enrolling patients. The following authors declare conflicts of interest relevant to this study: Lluís Puig (presentations for Merck Sharp & Dohme), Marta Ferrán (presentations and consulting for Merck Sharp & Dohme, Pfizer, AbbVie, and Novartis), José L. Sánchez-Carazo (consultant for Merck Sharp & Dohme), Ignacio Marín-Jiménez (presentations for Merck Sharp & Dohme, AbbVie, and Shire and consultation for Merck Sharp & Dohme, Ferring, Dr. Folk Pharma, AbbVie, FAES, and Shire), and Rosario García-Vicuña (consultant for the OpenSER project for allied health professionals). The other authors declare that they have no conflicts of interest.
Investigators from 15 hospitals participated in the study; we thank them for their help with enrolling and following patients. We thank Sofía Perea of Pipeline Biomedical Resources SL for her help in writing the manuscript.
Please cite this article as: Vanaclocha F, Crespo-Erchiga V, Jiménez-Puya R, Puig L, Sánchez-Carazo J, Ferrán M, et al. Enfermedades inflamatorias mediadas por inmunidad y otras comorbilidades en pacientes con psoriasis. Características basales de la cohorte de pacientes con psoriasis del estudio AQUILES. Actas Dermosifiliogr. 2015;106:35–43.