Kaposi’s sarcoma (KS) is considered to be a slowly progressive multifocal tumor of the endothelial cells. Four clinical subtypes have been described: a) classic (in elderly Mediterranean men); b) endemic (in Africa); c) HIV-associated; and d) iatrogenic, which affects immunodepressed patients and recipients of organ transplants.1All the subtypes of KS have a common etiology: infection with human herpesvirus-8 (HHV-8), which may be considered to be a necessary though not sufficient condition for developing the disease. Other factors (genetic, hormonal, and environmental) are also necessary, together with immunosuppression. The latency period from infection to development of KS may vary depending on the clinical type.1–3
A 70-year-old woman was referred to our outpatient dermatology department with ahistory of primary hypothyroidism, partial epilepsy, myoclonic tremor, moderate cognitive deterioration, osteoporosis, bronchial asthma, and giant cell arteritis that had appeared a year earlier and was treated with prednisone, 7.5 mg/d and methotrexate, 10 mg/d. The patient complained of multiple purplish papules that caused discomfort, plaques, and dome-shaped nodules measuring between 0.4 and 0.5 cm distributed over the earlobes, cheeks, cervical, periumbilical, and sacral regions, and both members (Figs. 1 and 2).
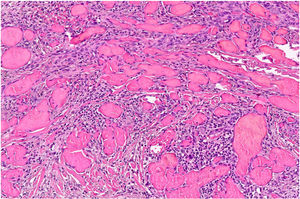
Clinical examination revealed no enlarged lymph nodes or splenomegaly. Histology was compatible with KS. The histologic study revealed a tumor composed of fusiform cells with cytologic atypia demarcating the vascular spaces, with some mitotic figures (Fig. 3). Immune staining showed proliferative cells positive for CD31, CD34, and HHV-8. Immune staining of β-adrenergic receptors was positive for B2-AR. B2-ARP and B3-AR immune-staining techniques were not available. The blood count, globular sedimentation rate, coagulation profile, general biochemistry and full-body CT scan were normal. Serology for HIV was negative. Treatment with methotrexate was stopped and a combination of cryotherapy and imiquimod cream, 5% was instated with a good response after 10 weeks of uninterrupted treatment. Three months later, despite the reduced immunosuppression, small bluish-purple plaques appeared on the lower limbs and spread slowly over the middle part of the ankle and left foot (Fig. 3). All the lesions resolved completely after 16 weeks of treatment with timolol gel, 0.5% twice daily, and prednisone was reduced to 5 mg/d. No recurrences were observed after 6 months of follow-up. The patient used 2 30-mg containers and did not finish the second container. Local toxicity (allergic contact dermatitis) and systemic toxicity were monitored and no adverse effects were observed during treatment.
KS is an angioproliferative disease, first described by Moritz Kaposi in 1872. It is classified into 4 subtypes: classic, endemic, HIV-associated, and iatrogenic, with different courses and epidemiology, but with similar histology. The iatrogenic form of KS appears in patients who are immunodepressed due to organ transplant (particularly kidney transplants), chemotherapy, or rheumatologic disease.4 In these cases, the disease usually appears a year after the first administration of the drugs. It has been reported with use of cyclosporin, oral corticosteroids, and other oral immunosuppressive agents.4–6 The pathogenic mechanism involved is still unknown, but it is linked to the inhibition of TGF-β and reactivation of infection with HHV-8, which leads to the induction of angiogenesis. The lesions have a multifocal clinical presentation. The course is variable, from an indolent form, with cutaneous manifestations only, to a disseminated form with extension to the mucous membranes and visceral involvement. Where the disease is localized on the skin, various treatment options are available, such as local resection, cryosurgery, photodynamic therapy, laser, imiquimod, alitretinoin gel, or radiation therapy.7,8 There is no cure and the objective of all these approaches is to manage the symptoms. If systemic dissemination appears, chemotherapy with liposomal doxorubicin is required.7 KS that appears in patients with significant immunosuppression will resolve, in most cases, when the immunosuppressive therapy is changed, reduced, or stopped.
Timolol is a nonselective β-adrenergic antagonist that exhibits antiangiogenic effects on topical administration for superficial infantile hemangioma. Its mechanism of action is not fully understood. The hypothesis has been suggested that beta blockers produce three consecutive steps (vasoconstriction, inhibition of proangiogenic signals, and induction of apoptosis of the endothelial cells) that lead to the regression of the hemangioma. By extrapolation to other proliferative vascular diseases, it has become an emerging alternative for localized KS (Table 1).9,10 No differences exist in the response rate of iatrogenic KS treated with timolol between immunocompetent and immunosuppressed patients. The main advantages of this treatment are the cost, ease of administration, and minimal adverse effects. Response time varies between 5 and 24 weeks (possibly related to the size of the lesion or lesions). Once the lesion has resolved, close vigilance is required, as only 2 of the 9 cases published in the literature have a follow-up period of more than 18 months.
Clinical Characteristics of Patients with Kaposi’s Sarcoma Treated With Topical Timolol.
| Patient | Age, y | Sex | Area Involved | Clinical Type | Size, cm | Associated Disease | Time to Remission, mo | Follow-Up, mo |
|---|---|---|---|---|---|---|---|---|
| 1 | 52 | M | Left leg | Plaque | 9 × 4 | None | 5 | 10 |
| 2 | 70 | F | Left foot | Plaque | 14 × 62.5 × 2.5 | Hypertension | 5 | 9 |
| 3 | 65 | M | Right leg | Plaque | 12 × 5 | None | 4 | 6 |
| 4 | 45 | M | Right arm | Plaque | 11 × 4 | HIV-TB | 6 | 4 |
| 5 | 78 | M | Right foot | Nodular | NA | None | 12 | 22 |
| 6 | 94 | F | Right leg | Nodular | NA | None | 12 | 20 |
| 7 | 89 | M | Both feet | Nodular | NA | Hypertension | 12 | 5 |
| 8 | 83 | M | Right hand | Nodular | NA | None | 18 | 4 |
| 9 | 71 | M | Penis | Nodular | NA | None | 24 | 10 |
Abbreviations: M indicates male; F, female; NA, not available; TB, tuberculosis; HIV, human immunodeficiency virus.
This case highlights the therapeutic challenge posed by iatrogenic KS. Reduction or elimination of immunosuppression does not always lead to resolution of KS and local treatment with topical timolol may be an effective, painless, simple, and economic option.
Please cite this article as: Espadafor-López B, et al. Sarcoma de Kaposi iatrogénico tratado con éxito con timolol tópico. Actas Dermosifiliogr. 2020;111:176–178.