A previously healthy 36-year-old Caucasian Portuguese male patient presented to the Dermatology clinic with a 5-day history of multiple painful and itchy papules on his feet. Two weeks earlier, he had travelled to Saint Thomas and Prince Islands, where he played football without wearing shoes. He had been observed four days earlier in another hospital for a similar lesion on his left ankle.
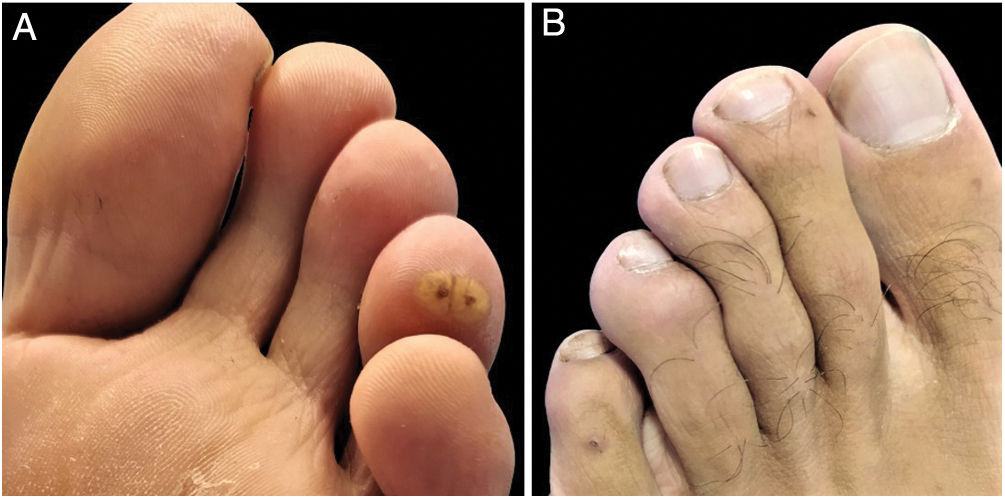
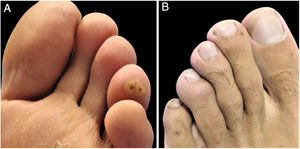
Physical examinationPhysical examination revealed three hyperkeratotic yellow-brown and two small red papules with dark central dots distributed over the ankle, sole and toes (Fig. 1 A and B).
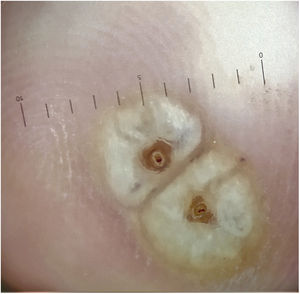
Additional testsDermoscopy revealed a white halo of hyperkeratosis and a dark central orifice surrounded by a white ovoid structure (Fig. 2).
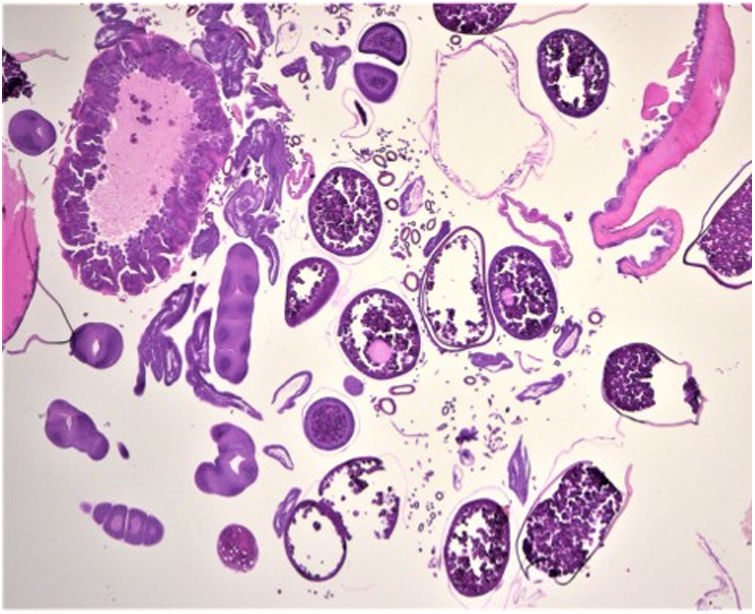
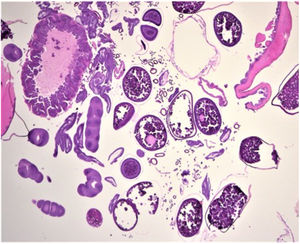
HistopathologySkin biopsy showed a collection of eggs at various maturation stages and sections of arthropod parasites, particularly reproductive and digestive portions and tracheal rings (Fig. 3).
What is the diagnosis?
DiagnosisClinical, dermoscopic and histopathological features allowed us to establish a diagnosis of tungiasis.
Clinical course and treatmentCurettage of the lesions was performed along with secondary bacterial infection prophylaxis with topical and systemic antibiotics (topical fusidic acid and oral amoxicillin–clavulanic acid) and treatment with topical ivermectin. The patient had previously received all the recommended tetanus vaccinations. Clinical resolution was observed in three weeks, with no complications at follow-up.
CommentTungiasis is a neglected ectoparasitosis caused by the penetration of the sand flea – Tunga penetrans or, less commonly, Tunga trimamillata – into the host's epidermis.1–5 It is endemic in sub-Saharan Africa, India, Latin America and the Caribbean, occurring in travellers returning from these regions.1–5 It is usually acquired from walking barefoot or with open-toed shoes.2,5 This parasite's primary habitat is sandy soils, but it can also be found in tropical forests and banana plantations.3,4 The patient usually complains of itch, pain and foreign body sensation.3 Lesions predominantly affect the feet, especially the periungual area of the toes, heels and soles, but it can affect any part of the body contacting with the infested soil.2–4 Skin findings differ, depending on the disease stage, and correlate with the embedded flea's life cycle.2,3 The female sand flea penetrates into the host's epidermis, leaving the posterior abdominal segment protruding, eliminating feces and laying eggs (100–200/week). This is followed by the development of a small red-brown macule, which evolves into the classic clinical presentation – a yellow papule with a dark central dot. The subsequent flea engorgement from egg production leads to swelling, erythema, pruritus and pain.1,2,4 If untreated, the flea's life cycle ends in about four to six weeks and forms a black-crusted papule.1,2,4 Although tungiasis diagnosis is clinical, dermoscopy can be a helpful tool, showing dark central pores, whitish oval structures, silver dendritic fibres and blue-black blotches in most cases.2 The differential diagnosis includes arthropod bite, abscess, wart, pyogenic granuloma, leishmaniasis, myxoid cyst, myiasis or a foreign body.2 Skin biopsy often reveals remnants of exoskeleton and egg shells.4 The sterile removal of each flea with sterile needles, shave or punch biopsies is the treatment of choice. After extraction, the sore should be treated with a topical antibiotic, and both oral antibiotic prophylaxis and tetanus vaccine should be considered.2,3,5 In patients with severe disease, topical ivermectin, topical dimethicone or oral thiabendazole may also be used.2,5 The most considerable complication is secondary bacterial infection such as cellulitis, necrotizing skin, soft tissue infection and tetanus.2 Tungiasis is an emerging infection in travellers to endemic areas, whose best preventive measure is to wear closed-toe shoes. Thus, it is essential to instruct travellers with these recommendations so as to avoid infestation by this parasite.2,3 Dermatologists must, therefore, be aware of it in order to promptly treat and prevent complications.
Conflict of interestsThe authors declare that they have no conflict of interest.
To Professor Soares-de-Almeida and doctors Marta Lobo and Pablo Espinosa for histopathological examination.