To determine the current practices of Spanish dermatologists performing home self-applied daylight photodynamic therapy (dPDT), and their experience with this treatment.
MethodologyWe conducted a retrospective, multicenter, cross-sectional observational study with participation from 100 dermatologists from public and private Spanish hospitals. Their practices were collected through an online questionnaire and prepared based on a literature review, including experience, climatology, advantages, disadvantages and satisfaction with the self-applied dPDT.
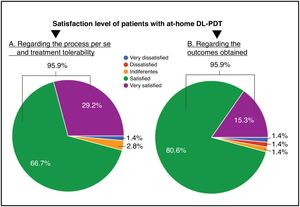
ResultsA total of 38.4% of dermatologists have >5 years of experience using dPDT and 72.7% alternate consultation and home self-application. A total of 61.1% of dermatologists do not have specific protocols for self-application and 69.4% explain instructions to their patients personally. A total of 50% prefer to apply dPDT in months of greater solar activity and 70.8% recommend treatment during the morning. A total of 95.9% of the patients are satisfied or very satisfied with the treatment.
Main conclusionsSelf-applied dPDT is an effective and well-tolerated option to treat AK, especially in patients who adequately follow instructions and have family support. It is necessary to protocolize the self-applied dPDT to guarantee a greater safety and efficacy profile in the home application format.
Determinar las prácticas actuales de los dermatólogos españoles para la realización de la terapia fotodinámica con luz de día (TFDLD) autoaplicada en el domicilio, y su experiencia con este tratamiento.
MetodologíaEstudio observacional transversal y multicéntrico, en el que participaron 100 dermatólogos de hospitales públicos y privados en España. Se recogieron sus prácticas a través de un cuestionario online, elaborado en base a una revisión de la literatura, incluyendo experiencia, climatología, ventajas, desventajas y satisfacción con la TFDLD autoaplicada.
ResultadosEl 38,4% de los dermatólogos acumula una experiencia de más de 5 años usando TFDLD y el 72,7% alterna entre consulta y autoaplicación en domicilio. El 61,1% de los dermatólogos no tiene un protocolo específico para la autoaplicación y un 69,4% explica personalmente las instrucciones. El 50% prefiere realizar la TFDLD en meses de mayor intensidad solar y un 70,8% recomienda el tratamiento por la mañana. El 95,9% de los pacientes están satisfechos o muy satisfechos con el tratamiento.
Conclusiones principalesLa TFDLD autoaplicada es una opción efectiva y bien tolerada para tratar la QA, especialmente en los pacientes que siguen adecuadamente las instrucciones y tienen apoyo familiar. Es necesario protocolizar la TFDLD autoaplicada para garantizar mayor eficiencia y seguridad en su aplicación domiciliaria.
Actinic keratoses (AKs) are premalignant skin lesions that occur frequently on areas exposed to ultraviolet (UV) radiation.1 In Spain, AK is the most common diagnosis in dermatology services, accounting for 6% of all visits, and its prevalence is estimated at 28.6% among people older than 45 years (95%CI, 27.2–30.1%).2,3
People with AK have a higher risk of developing cutaneous squamous cell carcinoma (SCC) and other malignant skin neoplasms.4 Reported malignant transformation rates range from 0.025% to 16%,5,6 and the risk of progression to SCC increases in patients with multiple AK lesions—fourfold in those with 6–20 lesions and up to elevenfold in those with more than 20 lesions.5,7
Among the available therapeutic options for AK, photodynamic therapy (PDT) is especially indicated for grade I and II AK and for field cancerization, particularly in photoexposed areas such as the face and scalp, with a grade A recommendation and level I evidence.8
Despite its benefits, one of the main drawbacks of PDT is pain—sometimes intense—during and after illumination. This concern largely motivated the development of daylight photodynamic therapy (DL-PDT) as a more comfortable, less painful alternative,9 with efficacy similar (non-inferior) to conventional PDT.10
A variant of hospital-based DL-PDT is patient self-applied DL-PDT at home. Some patients and specialists prefer this option because it can be adapted to individual lifestyle and schedule, allowing treatment where and when the patient chooses. Evidence shows that patient-applied DL-PDT achieves high levels of satisfaction, effectiveness, and tolerability.11–13
In 2015, the Spanish-Portuguese consensus document on methyl aminolevulinate (MAL) DL-PDT for AK was published,14 establishing a protocol for treating grade I and II AK suitable for the epidemiologic, meteorologic, and clinical characteristics of Spain and Portugal. However, several aspects of self-applied DL-PDT remain variable among dermatology services and merit clarification. In this context, our objective was to determine current practices of Spanish dermatologists regarding self-applied DL-PDT, as well as their personal experience with it.
Materials and methodsWe designed an observational, cross-sectional, prospective, multicenter study targeting dermatologists in Spain who perform hospital-based PDT. Considering that Spain has 162 dermatology departments in public hospitals,4 and that about 90% of them offer PDT,5 we invited a broad sample of dermatologists to participate. Fieldwork was conducted in the second half of 2022, and 100 dermatologists (10% private only, 25% public only, and 65% both public and private) completed an online questionnaire about their routine clinical practice in managing AK with self-applied DL-PDT.
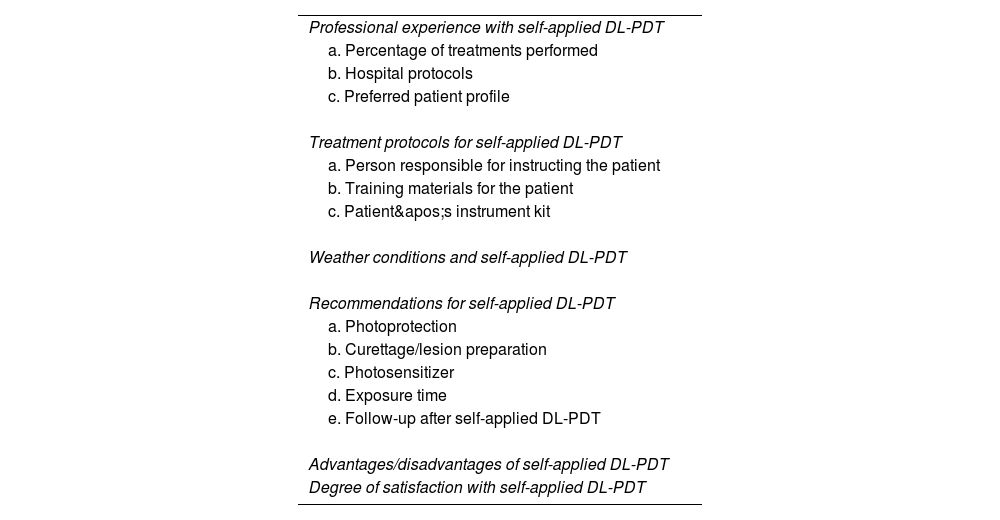
To develop the questionnaire, we performed a comprehensive literature review of hospital-based and self-applied DL-PDT in PubMed, Embase, and Cochrane over the past 20 years. Based on this review, 2 expert dermatologists in the topic drafted the questionnaire (Supplementary data). It covered: experience with self-applied DL-PDT; weather conditions during treatment; advantages and disadvantages of self-application; and levels of satisfaction among patients and dermatologists (Table 1). The Spanish-Portuguese DL-PDT consensus outlines the hospital protocol but does not address self-application at home,14 so we also collected the different protocols used (photoprotection, lesion preparation, photosensitizer, exposure time, and follow-up).
Topics addressed in the clinical-practice questionnaire on self-applied DL-PDT.
| Professional experience with self-applied DL-PDT |
| a. Percentage of treatments performed |
| b. Hospital protocols |
| c. Preferred patient profile |
| Treatment protocols for self-applied DL-PDT |
| a. Person responsible for instructing the patient |
| b. Training materials for the patient |
| c. Patient's instrument kit |
| Weather conditions and self-applied DL-PDT |
| Recommendations for self-applied DL-PDT |
| a. Photoprotection |
| b. Curettage/lesion preparation |
| c. Photosensitizer |
| d. Exposure time |
| e. Follow-up after self-applied DL-PDT |
| Advantages/disadvantages of self-applied DL-PDT |
| Degree of satisfaction with self-applied DL-PDT |
DL-PDT: daylight photodynamic therapy.
We conducted a descriptive statistical analysis using PSPP version 1.4.1, reporting categorical variables as percentages and quantitative variables as mean, percentages, and standard deviation.
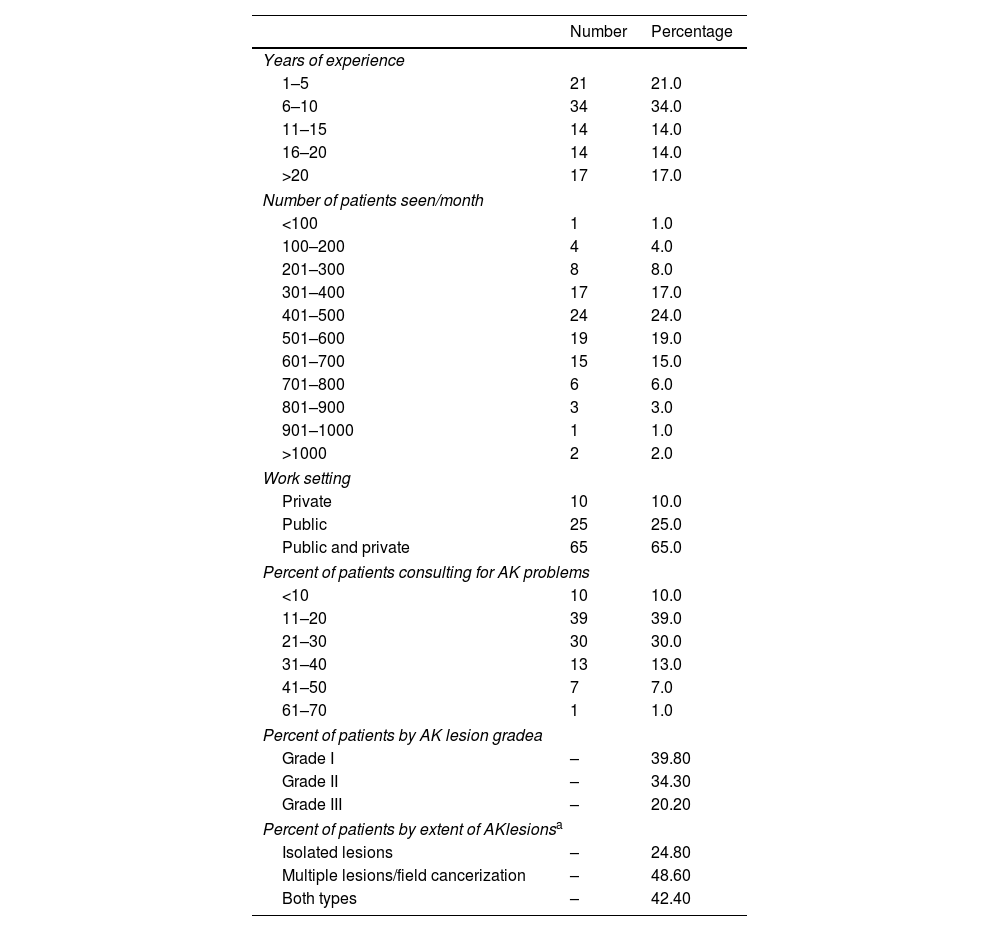
ResultsDermatologist characteristics and patient profileA total of 100 dermatologists participated; mean age was 40.6 years (SD, 9.79), with a mean of 12.8 (SD, 8.5) years in dermatology practice. Of these, 65% worked in both public and private settings, 25% public only, and 10% private only; most saw between 300 and 700 patients per week (Table 2). AK was a frequent reason for consultation: for 39% of dermatologists, it represented 11–20% of visits; for 30%, 21–30%.
Characteristics of the dermatologists participating in the study.
| Number | Percentage | |
|---|---|---|
| Years of experience | ||
| 1–5 | 21 | 21.0 |
| 6–10 | 34 | 34.0 |
| 11–15 | 14 | 14.0 |
| 16–20 | 14 | 14.0 |
| >20 | 17 | 17.0 |
| Number of patients seen/month | ||
| <100 | 1 | 1.0 |
| 100–200 | 4 | 4.0 |
| 201–300 | 8 | 8.0 |
| 301–400 | 17 | 17.0 |
| 401–500 | 24 | 24.0 |
| 501–600 | 19 | 19.0 |
| 601–700 | 15 | 15.0 |
| 701–800 | 6 | 6.0 |
| 801–900 | 3 | 3.0 |
| 901–1000 | 1 | 1.0 |
| >1000 | 2 | 2.0 |
| Work setting | ||
| Private | 10 | 10.0 |
| Public | 25 | 25.0 |
| Public and private | 65 | 65.0 |
| Percent of patients consulting for AK problems | ||
| <10 | 10 | 10.0 |
| 11–20 | 39 | 39.0 |
| 21–30 | 30 | 30.0 |
| 31–40 | 13 | 13.0 |
| 41–50 | 7 | 7.0 |
| 61–70 | 1 | 1.0 |
| Percent of patients by AK lesion gradea | ||
| Grade I | – | 39.80 |
| Grade II | – | 34.30 |
| Grade III | – | 20.20 |
| Percent of patients by extent of AKlesionsa | ||
| Isolated lesions | – | 24.80 |
| Multiple lesions/field cancerization | – | 48.60 |
| Both types | – | 42.40 |
AK: actinic keratosis.
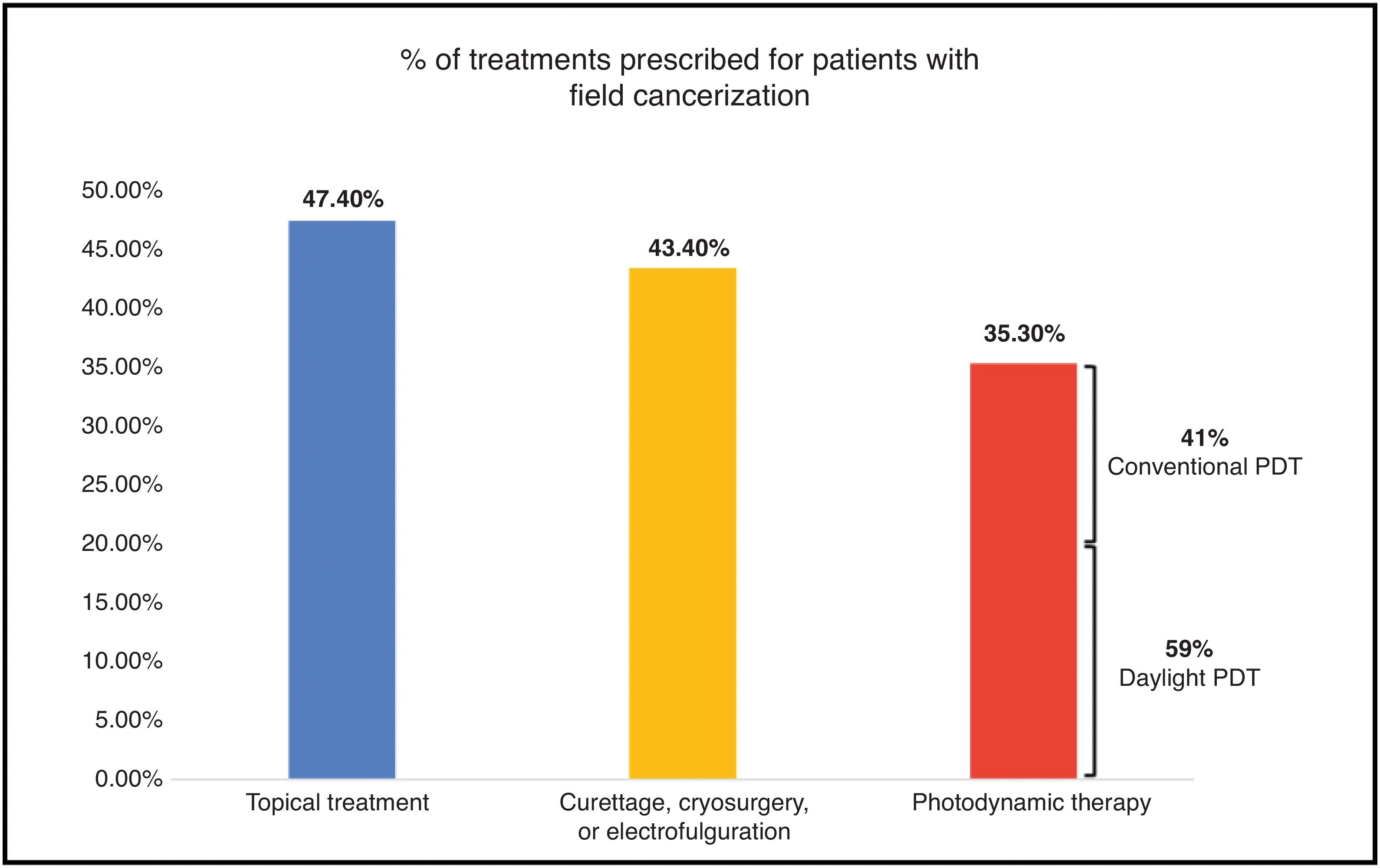
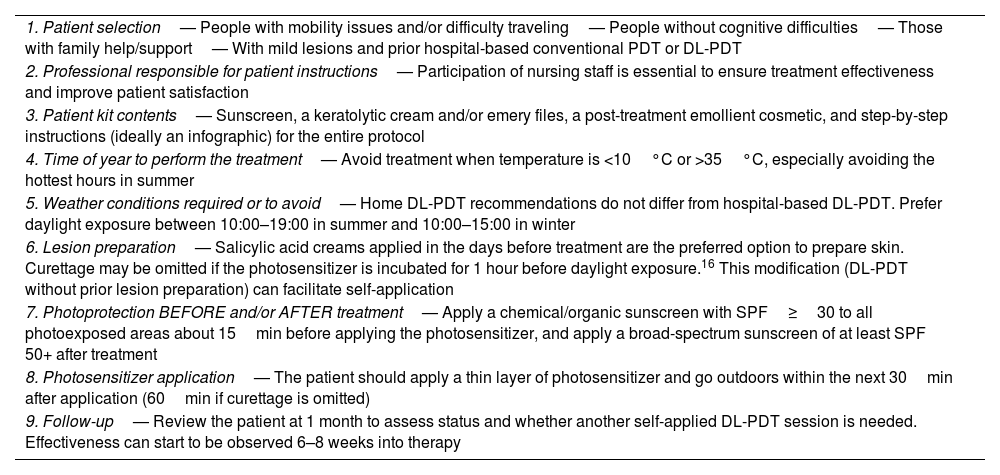
Respondents estimated that nearly 75% of their patients with AK have Olsen grade I or II lesions—39.8% grade I and 34.3% grade II (Table 2)—and 48.6% present multiple lesions/field cancerization. Up to 35.3% of field-cancerization patients receive PDT, and in 59% of those cases the modality is DL-PDT (Fig. 1).
Dermatologists’ experience with DL-PDTAmong respondents, 38.4% had >5 years’ experience using DL-PDT and 35.4% had 3–5 years. Most (72.7%) alternate between in-clinic administration and self-application at home. When prescribing the latter, dermatologists typically prescribe partially self-applied DL-PDT in 49.44% of patients (the dermatologist performs lesion preparation in clinic; in subsequent days the patient applies the photosensitizer and performs daylight exposure) and fully self-applied DL-PDT in 61.11% (patients complete all steps, including lesion preparation).
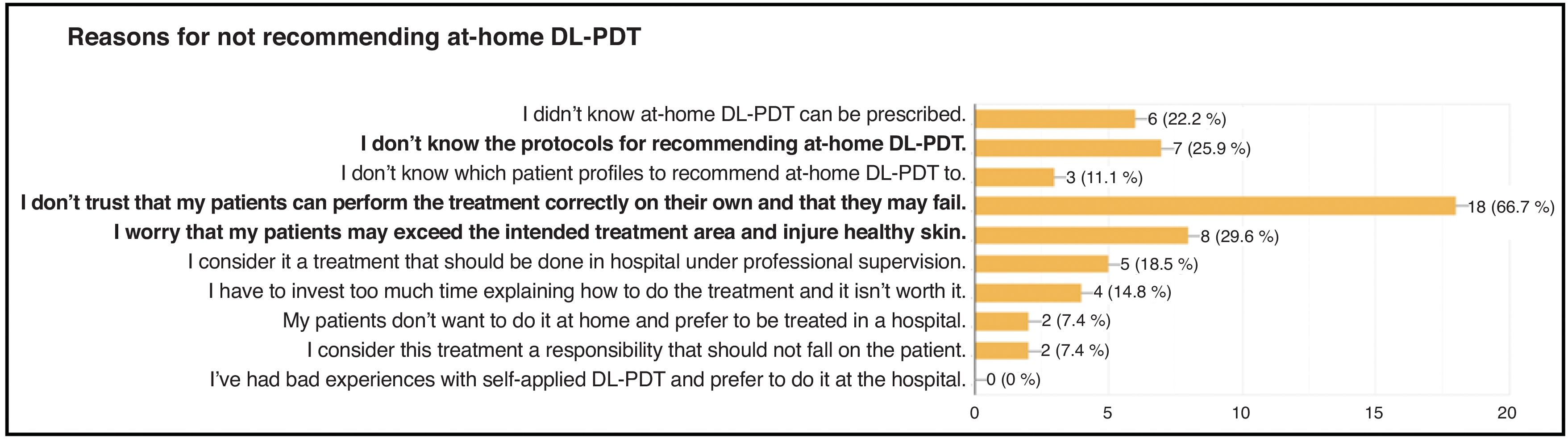
Among dermatologists who prescribe DL-PDT only at the hospital or their office (27.3%), common concerns include that patients “may not perform the treatment correctly on their own and fail,” or that they “may exceed the intended treatment area and damage healthy skin” (Fig. 2).
Protocols used and preferences for self-applied DL-PDTCurrently, 61.1% of dermatologists who do prescribe at-home DL-PDT do not have a clinic-specific protocol for self-application; they only have a hospital-based DL-PDT protocol.
In 69.4% of cases, the same dermatologist who prescribes and follows the treatment is responsible for instructing patients on self-application; 27.8% report that nursing staff provides these instructions.
A total of 83.3% give patients written materials to review outside the clinic (100% paper format—leaflet, sheets, etc.). In 36.1% of cases, these materials are complemented by a kit with items needed for treatment, most commonly sunscreen (88.5%) and sandpaper/emery files (53.8%).
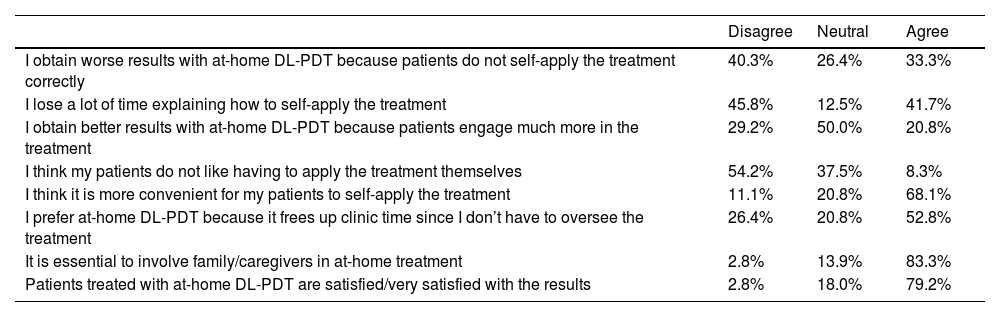
Dermatologists who prescribe self-applied DL-PDT showed high agreement (83.3%) that “it is essential to involve family/caregivers in at-home treatment,” and that “patients treated with self-applied DL-PDT are satisfied/very satisfied with the results” (79.2%). Agreement levels regarding DL-PDT are shown in Table 3.
Levels of agreement regarding preferences in self-applied DL-PDT.
| Disagree | Neutral | Agree | |
|---|---|---|---|
| I obtain worse results with at-home DL-PDT because patients do not self-apply the treatment correctly | 40.3% | 26.4% | 33.3% |
| I lose a lot of time explaining how to self-apply the treatment | 45.8% | 12.5% | 41.7% |
| I obtain better results with at-home DL-PDT because patients engage much more in the treatment | 29.2% | 50.0% | 20.8% |
| I think my patients do not like having to apply the treatment themselves | 54.2% | 37.5% | 8.3% |
| I think it is more convenient for my patients to self-apply the treatment | 11.1% | 20.8% | 68.1% |
| I prefer at-home DL-PDT because it frees up clinic time since I don’t have to oversee the treatment | 26.4% | 20.8% | 52.8% |
| It is essential to involve family/caregivers in at-home treatment | 2.8% | 13.9% | 83.3% |
| Patients treated with at-home DL-PDT are satisfied/very satisfied with the results | 2.8% | 18.0% | 79.2% |
DL-PDT: daylight photodynamic therapy.
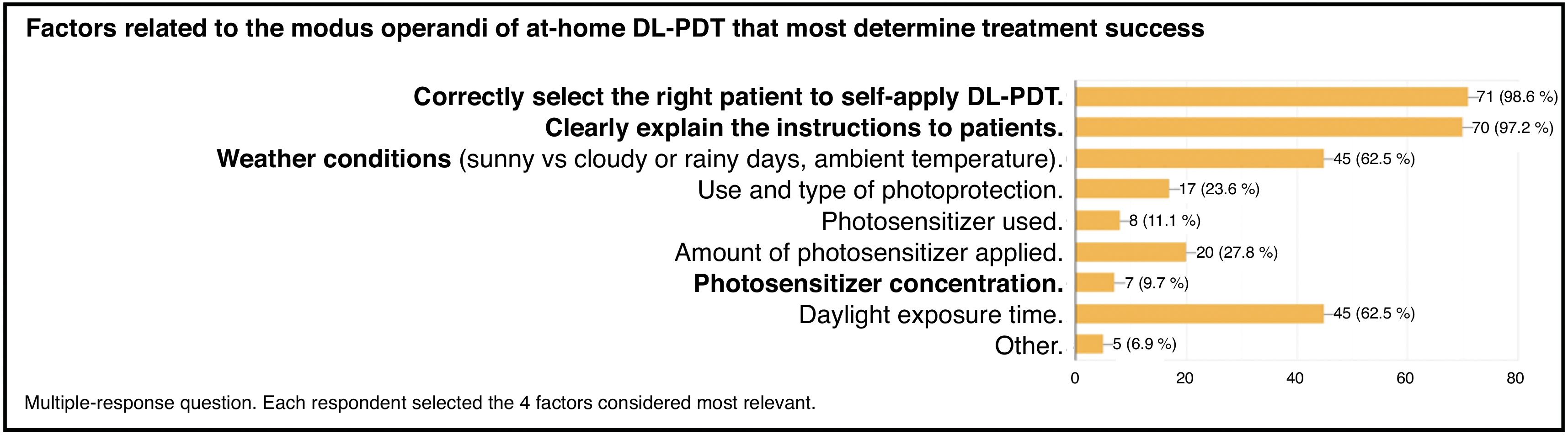
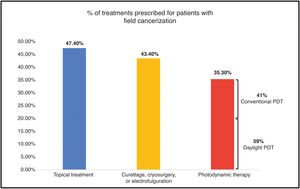
Although most dermatology services lack specific protocols for self-applied DL-PDT, there is broad agreement on the key operational factors that determine treatment success at home (Fig. 3). The 4 most relevant ones were (1) appropriately selecting eligible patients for self-applied DL-PDT (98.6%); (2) providing clear instructions (97.2%); and (3) weather conditions (sunny vs cloudy/rainy, ambient temperature, etc.) and (4) total daylight exposure time (both at 62.5%).
Time of year and time of dayAlthough in Spain the irradiance threshold for DL-PDT (≈130W/m2) is readily met year-round,13 50% of dermatologists who prescribe self-applied DL-PDT prefer the months with higher solar intensity (April–October), though they also prescribe it during November–March.
Regarding time of day, 70.8% recommend performing treatment in the morning from 10:00, 19.4% at any time of day, and 9.8% around midday.
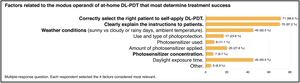
Sunscreen use with self-applied DL-PDTThe DL-PDT consensus recommends applying a broad-spectrum sunscreen SPF≥30 with organic/chemical filters at least 15min before starting treatment.14
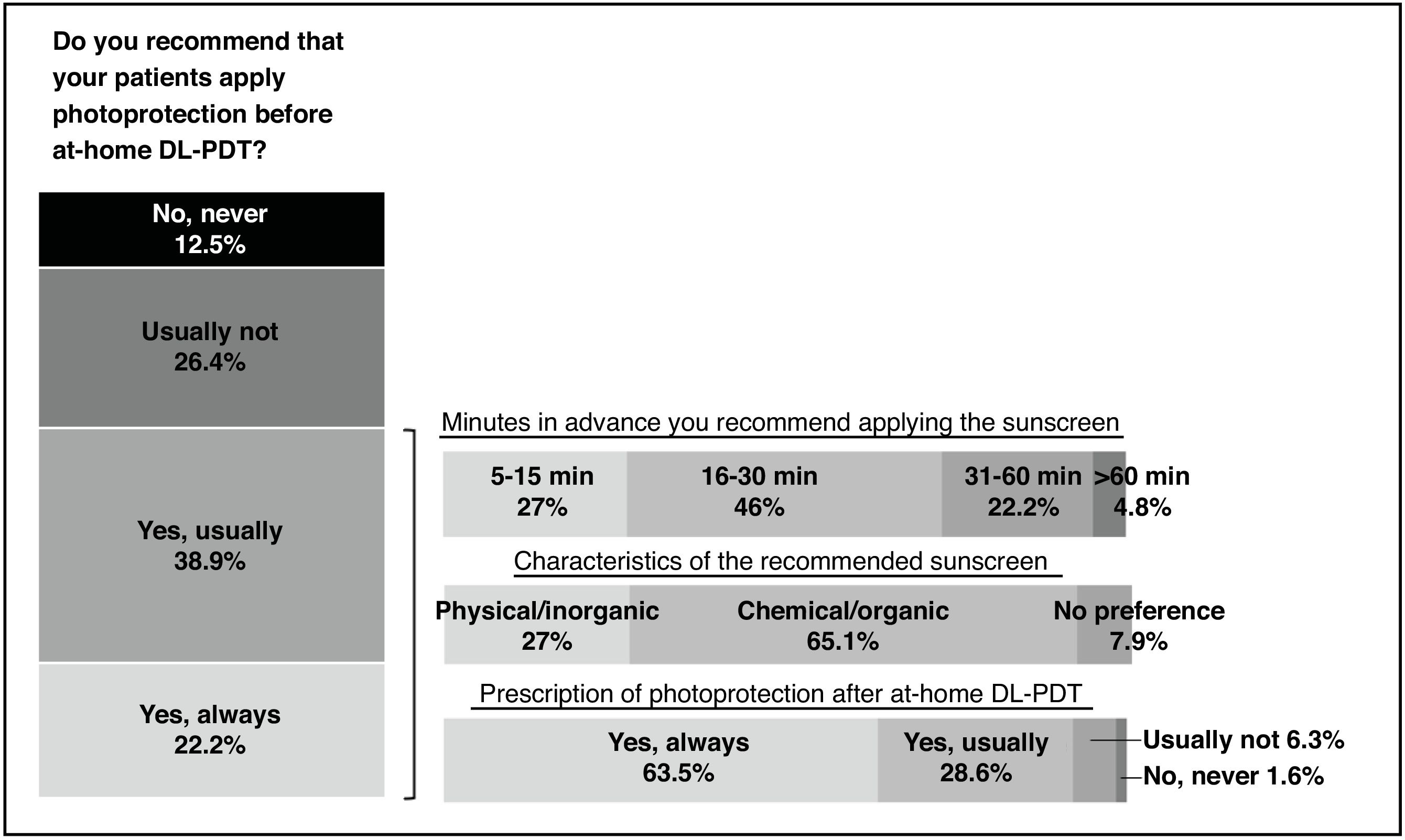
Among prescribers of self-applied DL-PDT, 61.1% advise sunscreen before treatment. Of these, 46% recommend applying it 16–30min before the photosensitizer; 65.1% recommend a chemical/organic sunscreen; while 92.1% recommend post-treatment photoprotection (Fig. 4).
Curettage/lesion preparation for self-applied DL-PDTThe DL-PDT protocol stipulates preparing the treatment area before applying the photosensitizer by removing scales or crusts. Options include sandpaper/emery, curettes, keratolytic creams with urea or salicylic acid, microneedling, and even laser.14
For self-applied DL-PDT, 79.2% of prescribers perform some form of curettage or lesion preparation in clinic before patients self-apply treatment; nearly half (47.2%) do this 1–3 days beforehand.
Additionally, 76.4% also recommend that patients perform their own lesion preparation (to remove scales/crusts) before self-applying treatment—most frequently with a salicylic acid cream (78.2%).
Photosensitizers used with self-applied DL-PDTFor hospital-based DL-PDT, a thin layer of photosensitizer is applied over the AKs without occlusion, and the patient should proceed to daylight exposure within the next 30min (not later).14
In line with these recommendations, 80.8% of dermatologists who prescribe self-applied DL-PDT instruct patients to apply the photosensitizer no more than 30min before exposure, and 70.8% specify applying a thin layer.
Sunlight exposure time with self-applied DL-PDTAs a rule, patients should remain outdoors for 2h to allow adequate protoporphyrin IX (PpIX) accumulation and achieve satisfactory PDT.14 DL-PDT is not recommended at temperatures below 10°C (discomfort outdoors and hindered photosensitizer metabolism) or above 35°C (excessive sweating and heat).
Available evidence indicates that the DL-PDT response rate for mild-to-moderate AK is not influenced by weather on the treatment day (sunny, cloudy, or partly cloudy).14 However, 62.5% of prescribers vary daylight exposure recommendations according to weather conditions, and 65.3% usually check the forecast before prescribing self-applied DL-PDT.
On a sunny summer day, 63.9% recommend 2h of exposure and 36.1% recommend less. On a sunny winter day, the proportion recommending 2h rises to 86.1%, and 12.5% would recommend more than 2h; only 1.4%advise less than 2h in that scenario.
On a cloudy day (10–35°C), 79.2% recommend 2h of daylight exposure and 19.4% recommend more than 2h.
Follow-up for self-applied DL-PDTThe hospital-based DL-PDT consensus recommends assessing treated lesions after 3 months.13 In keeping with this, for self-applied DL-PDT, 76.4% of respondents schedule follow-up one month or more after treatment.
Overall, 62.5% consider that the effectiveness of self-applied DL-PDT can be meaningfully assessed starting 6–8 weeks into therapy.
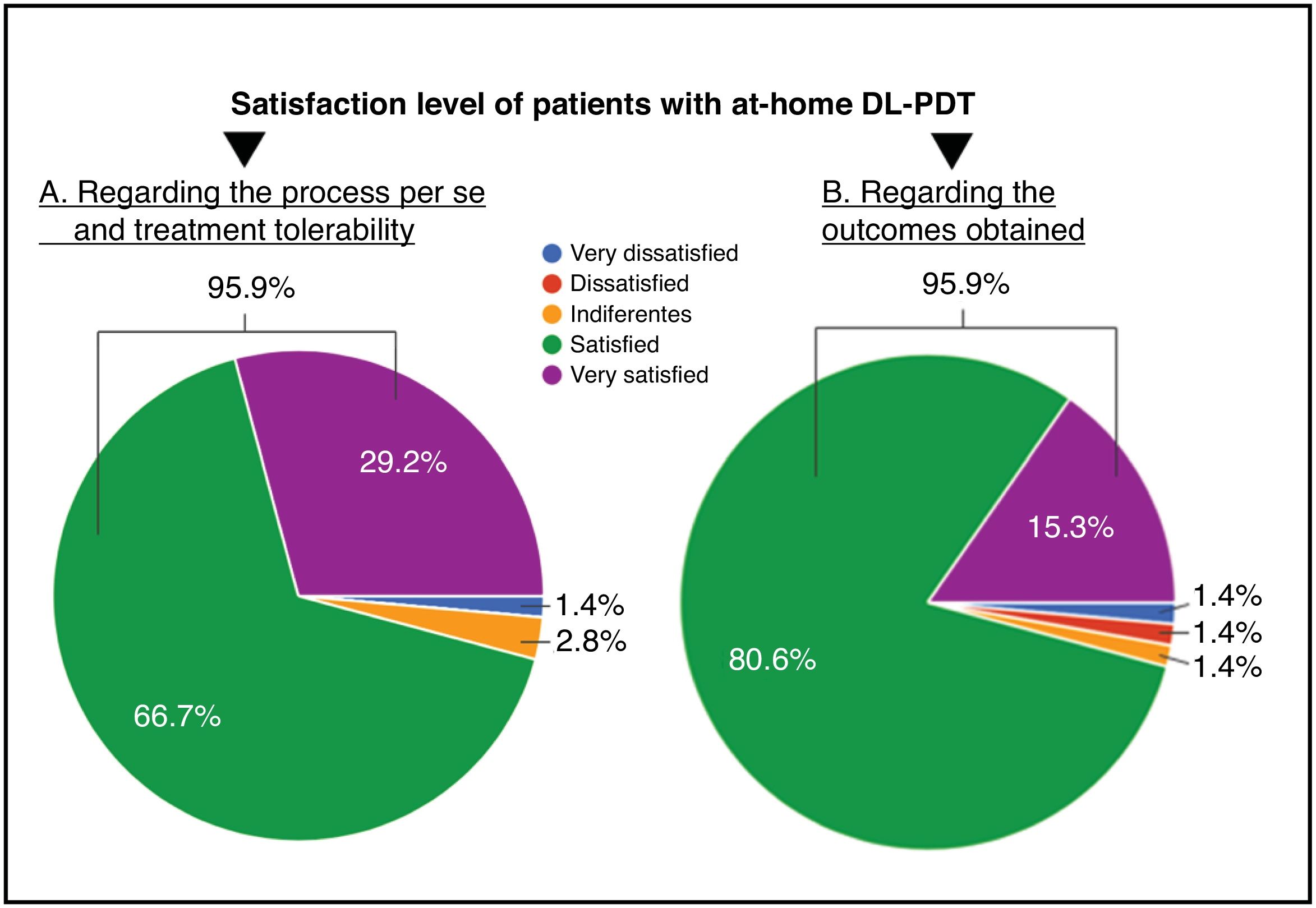
Satisfaction with self-applied DL-PDTAmong dermatologists who prescribe self-applied DL-PDT, 95.9% report that patients are satisfied or very satisfied with the process per se, tolerability, and outcomes (Fig. 5).
Comparing dermatologist satisfaction between hospital-based and self-applied DL-PDT, 47.2% are equally satisfied with both, 37.5% are more satisfied with hospital-based DL-PDT, and 15.3% prefer self-applied DL-PDT. In any case, 97.2% consider that self-applied DL-PDT is a treatment they will expand in their service.
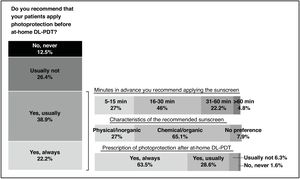
Queries on best practices for at-home self-applied DL-PDTFinally, dermatologists were asked how certain aspects of self-applied DL-PDT should be handled to help draft a protocol. The most frequent responses are summarized in Table 4.
Most relevant topics to consider when drafting a best-practice protocol for self-applied DL-PDT.
| 1. Patient selection— People with mobility issues and/or difficulty traveling— People without cognitive difficulties— Those with family help/support— With mild lesions and prior hospital-based conventional PDT or DL-PDT |
| 2. Professional responsible for patient instructions— Participation of nursing staff is essential to ensure treatment effectiveness and improve patient satisfaction |
| 3. Patient kit contents— Sunscreen, a keratolytic cream and/or emery files, a post-treatment emollient cosmetic, and step-by-step instructions (ideally an infographic) for the entire protocol |
| 4. Time of year to perform the treatment— Avoid treatment when temperature is <10°C or >35°C, especially avoiding the hottest hours in summer |
| 5. Weather conditions required or to avoid— Home DL-PDT recommendations do not differ from hospital-based DL-PDT. Prefer daylight exposure between 10:00–19:00 in summer and 10:00–15:00 in winter |
| 6. Lesion preparation— Salicylic acid creams applied in the days before treatment are the preferred option to prepare skin. Curettage may be omitted if the photosensitizer is incubated for 1 hour before daylight exposure.16 This modification (DL-PDT without prior lesion preparation) can facilitate self-application |
| 7. Photoprotection BEFORE and/or AFTER treatment— Apply a chemical/organic sunscreen with SPF≥30 to all photoexposed areas about 15min before applying the photosensitizer, and apply a broad-spectrum sunscreen of at least SPF 50+ after treatment |
| 8. Photosensitizer application— The patient should apply a thin layer of photosensitizer and go outdoors within the next 30min after application (60min if curettage is omitted) |
| 9. Follow-up— Review the patient at 1 month to assess status and whether another self-applied DL-PDT session is needed. Effectiveness can start to be observed 6–8 weeks into therapy |
SPF: sun protection factor; PDT: photodynamic therapy; DL-PDT: daylight photodynamic therapy.
For AK and field cancerization, the advent of hospital-based DL-PDT represented a significant advance over conventional PDT.14 In recent years, enabling patients to perform DL-PDT at home has added advantages for dermatologists and for selected patients. Dermatologists recognize that similar outcomes can be obtained with self-applied DL-PDT when patients or their family/caregivers are engaged. However, loss of control over protocol execution, uncertainty about meteorologic variables, and the inability of some patients to proceed without supervision create concerns—highlighting the need for tools that improve oversight and guide patients simply through the process.
A hospital-based DL-PDT protocol was published in 2015.14 Although hospital and at-home procedures are similar, it is important to standardize at-home DL-PDT so dermatologists can more efficiently select treatments for different AK patients and achieve safe, satisfactory outcomes when patients self-apply.15
AK is a chronic disease, and treatment should be individualized to patient needs and expectations.11 The option of at-home DL-PDT effectively converts a hospital therapy into another topical treatment—with the added advantage of being completed in a single day.16 Simpler, shorter regimens improve adherence, patient satisfaction, and overall quality of life in AK.13
Recently, self-applied DL-PDT using BF-200 ALA gel was compared with hospital-based DL-PDT, showing an equivalent safety and efficacy profile for AK treatment; high satisfaction and convenience at home may further enhance adherence.17
The main limitation of this study is sampling: participants were not randomly selected, and data were available only from dermatologists who agreed to participate.
In conclusion, this study describes current clinical practice of at-home DL-PDT in Spain—its advantages and uncertainties. Based on respondent opinions, we provide recommendations that may assist in patient selection and treatment execution. Together, these findings aim to serve as the basis for an at-home DL-PDT protocol adapted to our patients and national weather conditions.
FundingGalderma supported project funding. The sponsor did not participate in manuscript writing.
Conflicts of interestFor this article, none of the authors reports conflicts of interest related to the topics discussed, which they address solely from their clinical experience.
Dr. Tamara Gracia-Cazaña has collaborated with SiHealth, Galderma, Cantabria Labs, Almirall, and Isdin. Dr. Yolanda Gilaberte has collaborated with SiHealth, Galderma, Isdin, La Roche-Posay, IFC, Rilastil, Uriage, AbbVie, and Cantabria Labs.
The authors thank the participant dermatologists for their invaluable collaboration, and Galderma for logistical support with participant recruitment/contact and for financial support.