We present the case of a 52-year-old woman with a history of pollen allergy and hand eczema. She was referred to our department with redness, itching, and inflammation of the hands that had first appeared 24 hours earlier after contact with raw shellfish. These episodes rarely appeared when her hand eczema was well controlled. The patient denied having experienced wheals or labial edema after intake of raw shellfish. She reported worsening of the condition after using latex gloves at work, which forced her to stop using them.
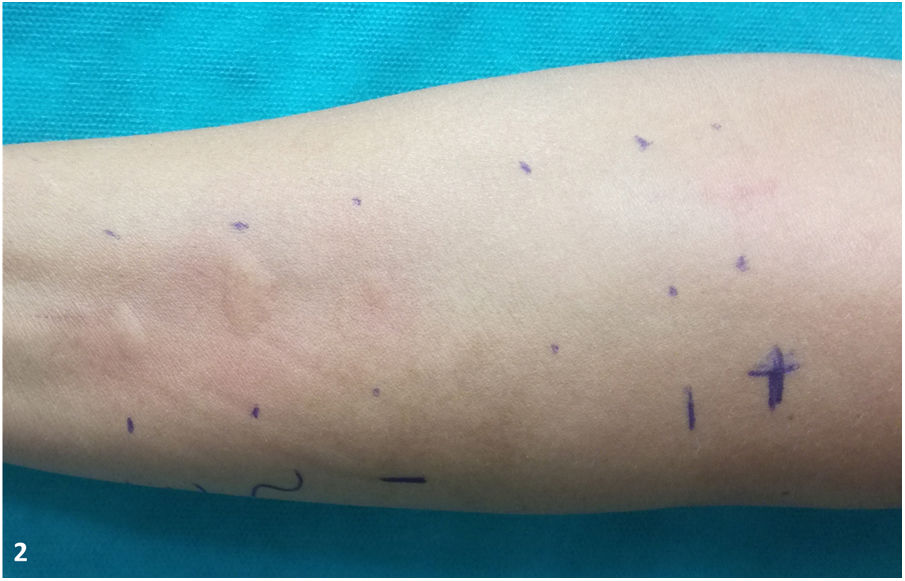
Physical examination revealed erythematous, scaly plaques with marked lichenification on the dorsa of the hands and lateral aspects of the fingers. Superficial fissures were also observed on the fingers (Fig. 1).
The initial suspicion was protein contact dermatitis (PCD) to shellfish. The additional tests performed to confirm the diagnosis were as follows:
- Skin biopsy, which revealed spongiotic dermatitis with a perivascular lymphocytic infiltrate in the papillary dermis and eosinophils.
- Rub test with the patient’s own products (prawn, king prawn, and shrimp), which led to pruritus and erythema after 10 minutes on the areas of the skin with eczematous lesions and no reaction on healthy skin.
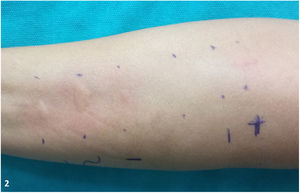
- Prick test (prick-by-prick test) with the patient’s own products (prawn, king prawn, shrimp, and latex): the reading at 20 minutes revealed positive results (> 3 mm), as follows: prawn, ++; king prawn, +++; shrimp, ++ (Fig. 2).
- Patch tests from the standard series of the Spanish Skin Allergy and Contact Dermatitis Research Group and the patient’s own products (prawn shell, prawn meat, king prawn shell, king prawn meat, shrimp shell, shrimp meat). A reading at 72 hours revealed a doubtful reaction (+/−, edge effect to prawn meat) (Fig. 3). The reading at 168 hours revealed no positive results.
Exogenous dermatitis is classed as irritant contact dermatitis and allergic contact dermatitis (ACD). ACD is mediated by a delayed hypersensitivity mechanism (type iv). Other clinical pictures are triggered by immediate hypersensitivity mechanisms (type i), such as allergic contact urticaria manifesting as wheals and/or urticaria or conditions triggered by a combination of both mechanisms, such as PCD.1
In the case of PCD, the allergens are high-molecular-weight proteins that are associated mainly with food (animal proteins, vegetable proteins, flours, cereals, and enzymes). Therefore, this type of dermatitis is more common in professionals working in this field (e.g., cooks, butchers, bakers), without forgetting homemakers and people who cook at home.
Onset of symptoms is minutes after exposure and is characterized by erythema, intense pruritus, and/or vesicular lesions on previous dermatitis lesions (i.e., on damaged skin, not healthy skin). PCD does not manifest as wheals, thus enabling it to be distinguished from chronic idiopathic urticaria.
The absence of symptoms after exposure in healthy skin can be explained by the fact that the allergens in PCD are high-molecular-weight proteins that do not come into contact with Langerhans cell receptors. In contrast, in ACD or chronic idiopathic urticaria, the allergens are low-molecular-weight haptens, which can cross the epidermal barrier easily.
Therefore, PCD leads to a positive result in the rub test on affected skin and a negative result on healthy skin, unlike ACD and chronic idiopathic urticaria, where the result is positive in both.
Patch tests are essential for distinguishing between these conditions and are negative in most cases of PCD. This makes it possible to establish a differential diagnosis with ACD. On the other hand, prick testing, which reproduces an IgE-mediated reaction, is positive in most cases of PCD and negative in ACD.
Treatment is based on 2 fundamental pillars: avoidance of the allergen involved in the reaction and treatment of the skin lesions, which depends on the degree of involvement and severity.
In the present case, the acute onset of symptoms, mainly pruritis after contact with shellfish, and the negative rub test result enabled us to reasonably rule out contact urticaria to shellfish.
This observation, together with the negative patch test results, made it possible to confirm the diagnosis of PCD to raw shellfish.2–4
The patient was recommended to avoid contact with shellfish and prescribed a topical corticosteroid. The lesions resolved after a few months, and the patient has not experienced new flare-ups after 8 months of follow-up.
This condition should be suspected in patients with hand eczema who handle food. Since patch test results are mostly negative, it is necessary to perform immediate-type tests, with prick-by-prick being the most sensitive approach in these cases.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Calleja Algarra A, Aragón Miguel R, Ortiz de Frutos FJ, Tous Romero F. Lesiones en manos tras contacto con marisco, más allá de las pruebas epicutáneas. Actas Dermosifiliogr. 2021;112:274–275.