The incidence of urethritis due to Haemophilus species is increasing. The main aim of this study was to describe the clinical and microbiological characteristics of patients with this form of urethritis. A secondary aim was to discuss the adequacy of treatments in patients with different types of antibiotic resistance.
Material and methodsWe studied patients with a microbiologically confirmed diagnosis of urethritis seen at the Sexually Transmitted Infections Unit of our hospital between July 2015 and July 2018. We selected all patients in whom Haemophilus species were isolated on chocolate agar. Antibiotic resistance was tested using the disk-diffusion method. Cross-sectional data were collected prospectively during outpatient visits.
ResultsHaemophilus species were isolated in 33.6% of cases. The most common clinical manifestation was urethral discharge (57.6%); 60% of the patients were men who have sex with men and in this subgroup Haemophilus species were significantly more common than either Neisseria or Chlamydia species. Haemophilus species were found in isolation in 39.5% of patients and the most common one was Haemophilus parainfluenzae (isolated in 84.2% of cases). In total, 34.2% of patients were resistant to azithromycin and 26.3% were resistant to both azithromycin and tetracycline. Empirical treatment achieved clinical and microbiologic cure in 11 of the patients who were not lost to follow-up (n=17; 44.7%). The remaining 6 patients required treatment with a new antibiotic.
ConclusionsHaemophilus species are a new cause of nongonococcal urethritis, whose incidence is rising, particularly in men who have sex with men who engage in unprotected oral sex. The clinical manifestations are similar to those seen in gonococcal urethritis. Eradication of infection must be confirmed due to the high rate of antibiotic resistance associated with Haemophilus species.
La incidencia de uretritis por Haemophilus está aumentando. Nuestro objetivo principal es describir las características clínico-microbiológicas de estos pacientes. Como objetivo secundario discutiremos el tratamiento más adecuado en función de las resistencias antibióticas testadas.
Material y métodosSeleccionamos los pacientes de la Unidad de Infecciones de Transmisión Sexual diagnosticados microbiológicamente de uretritis entre julio de 2015 y julio de 2018. De ellos, seleccionamos aquellos en los que se aisló un Haemophilus mediante cultivo agar chocolate. Las resistencias antibióticas se testaron mediante método de difusión disco-placa. De estos pacientes se recogieron los datos de forma transversal y prospectiva durante las visitas en consultas externas.
ResultadosSe aisló un Haemophilus spp. en 33,6% de los pacientes diagnosticados de uretritis. De estos pacientes, la manifestación clínica más frecuente fue la supuración uretral (57,9%) y el 60% eran hombres que tienen sexo con hombres, siendo el aislamiento de este microorganismo más frecuente de forma estadísticamente significativa entre los hombres que tienen sexo con hombres que el aislamiento de Neisseria o Chlamydia. Haemophilus spp. se encontró de forma aislada en el 39,5% de los pacientes, siendo el más frecuente H. parainfluenzae en el 84,2%. El 34,2% de los casos de Haemophilus aislados fueron resistentes a azitromicina y el 26,3% eran resistentes tanto a azitromicina como a tetraciclinas. En los casos en los que no se perdió el seguimiento del paciente (n=17; 44,7%), el tratamiento administrado de forma empírica consiguió una remisión clínica y microbiológica en 11 pacientes, mientras que en 6 fue necesario administrar una pauta de un nuevo antibiótico.
ConclusionesHaemophilus es un nuevo agente etiológico de uretritis no gonocócicas cuya incidencia está en aumento, especialmente entre hombres que tienen sexo con hombres que practican sexo oral sin protección. Estos pacientes pueden presentar una clínica similar a una uretritis gonocócica. Es necesario confirmar la erradicación debido al elevado número de resistencias antibióticas testadas en Haemophilus spp.
Urethritis is the syndrome most frequently associated with sexually transmitted infections (STIs),1 and is etiologically classified as either gonococcal urethritis (GU), caused by Neisseria gonorrhoeae, or nongonococcal urethritis (NGU), caused by other etiological agents, such as Chlamydia trachomatis, Mycoplasma species, or Ureaplasma species.2 However, the etiology of 30% to 40% of NGU cases is unknown.3 Bacteria of the genus Haemophilus are among several newly proposed etiological agents of NGU, especially among men who have sex with men (MSM).3
Here, we describe the clinical and microbiological characteristics of patients with urethritis caused by Haemophilus species, and discuss the most appropriate treatment strategies in patients with antibiotic resistance.
Material and MethodsThis was a descriptive, observational study, in which data were collected in a structured, prospective interview. The study included all patients with a microbiologically confirmed diagnosis of urethritis who were seen between July 2015 and July 2018 at the Sexually Transmitted Infections Unit of the Hospital General Universitario de Valencia, Valencia, Spain. From this group of patients we selected those in whom Haemophilus species were isolated on chocolate agar. Antibiotic susceptibility of the Haemophilus isolates was evaluated using the disc-plate diffusion method.
Cross-sectional clinical and epidemiological data were collected during the patients’ first visit. All patients were managed in accordance with the clinical guidelines of the Spanish AIDS Study Group (GeSIDA). During the first visit, a urethral exudate sample was taken from all patients with a clinical diagnosis of urethritis for bacterial culture and polymerase chain reaction testing for STIs. This same procedure was performed for all asymptomatic patients who were seen at the STI Unit for unprotected sexual contact with casual partners. Patients with a suspected diagnosis of urethritis were treated empirically with doxycycline (100 mg every 12 h) or a single dose of azithromycin (1 g) at the discretion of their physician. In cases in which GU was suspected owing to the presence of abundant urethral suppuration, a single dose of intramuscular ceftriaxone (250 mg) was also administered.
During a second visit 4 to 6 weeks later, patients were re-evaluated and a second sample collected for microbiological analysis. If the patient's clinical signs and/or the Haemophilus isolate proved resistant to the prescribed treatment, a new antibiotic treatment was selected according to the findings of the antibiogram. In such cases, patients were evaluated once again 4 to 6 weeks after the second visit.
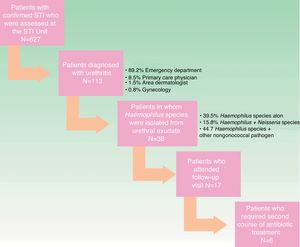
A flow chart illustrating the process of patient inclusion in the study is shown in Figure 1.
ResultsA total of 113 patients were diagnosed with microbiologically confirmed urethritis, of whom 31 (27.4%) were diagnosed with GU, 66 (58.4%) with NGU, and 16 (14.2%) with mixed urethritis (NG and NGU). Haemophilus species were isolated from 38 patients (33.6%). Clinical and epidemiological data for these patients are summarized in Table 1. Of the 38 patients diagnosed with urethritis due to Haemophilus species, 35 were male and 3 were heterosexual women. The mean age was 30.5 years. Of the 35 male patients, 21 (60%) were MSM. Among the MSM patients, Haemophilus species were isolated from the urethra significantly more often than either N gonorrhoeae (P=.017) or C trachomatis (P<.001).
Clinical and Microbiological Data for Patients Diagnosed With Urethritis Caused by Haemophilus Species
| Data | Number of Cases (%) |
|---|---|
| Sex | |
| Male | 35 (92.1) |
| Female | 3 (7.9) |
| Mean age, y; SD | 30.5; 8.7 |
| Sexual orientation | |
| Men who have sex with men | 21 (55.3) |
| Heterosexual men | 13 (34.2) |
| Heterosexual women | 3 (7.9) |
| Unknown | 1 (2.6) |
| Previous STI | 20 (57.1) |
| Syphilis | 8 (21) |
| Urethritis | 4 (11.4) |
| HIV infection | 5 (13.2) |
| Pediculosis pubis | 1 (2.6) |
| Condyloma acuminatum | 4 (11.4) |
| Chlamydia trachomatis proctitis | 1 (2.6) |
| Type of consultation | |
| Emergency department | 34 (85.7) |
| Primary care physician | 5 (14.3) |
| Clinical presentation | |
| Purulent urethral discharge | 22 (57.9) |
| Dysuria | 6 (15.8) |
| Asymptomatic / unsafe sexual contact | 10 (26.3) |
| Haemophilus species | |
| H parainfluenzae | 32 (84.2) |
| H influenzae | 5 (13.2) |
| H haemolyticum | 1 (2.6) |
| Coinfections | |
| Haemophilus species sole agent isolated | 15 (39.5) |
| Haemophilus + Neisseria | 6 (15.8) |
| Haemophilus + Chlamydia | 7 (18.4) |
| Haemophilus + Mycoplasma genitalium | 2 (5.2) |
| Haemophilus + Mycoplasma hominis/Ureaplasma species | 9 (23.6) |
| Treatment outcome | |
| Clinical signs resolved after antibiotic treatment | 11 (28.9) |
| Clinical signs resolved after treatment with more than one antibiotic | 6 (15.8) |
| Lost to follow-up | 21 (55.3) |
Abbreviations: HIV, human immunodeficiency virus; SD, standard deviation; STI, sexually transmitted infection.
Thirty-three (86.8%) of the 38 patients had visited the emergency department. The most common presenting complaint was marked urethral suppuration (22 patients [57.9%]). Ten patients (26.3%) were asymptomatic and consulted for unsafe sexual contact; 2 patients reported contact with a person diagnosed with NGU, and the other 8 were seen because they had unsafe sexual contact with a casual partner. The remaining 15.8% were seen for dysuria without evident urethral discharge. In total, 57.1% of patients had a prior STI, the most frequent of which were syphilis, human immunodeficiency virus infection, urethritis, and condylomata acuminata. All patients had received unprotected oral sex within a mean of 22.7 days before the consultation. The most commonly isolated Haemophilus species was H parainfluenzae, which was isolated in 32 patients (84.2%), followed by Haemophilus influenzae (5 patients [13.2%]).
Haemophilus species were found in isolation in 15 (39.5%) of the 38 patients, 9 of whom (60%) presented with marked urethral suppuration. Urethritis caused by Haemophilus species was associated with GU in 6 patients (15.8%). One or more classical etiological agents of NGU were detected in 17 patients (44.7%): C trachomatis in 7 patients (18.4%); Mycoplasma genitalium in 2 patients (5.2%); Mycoplasma hominis in 4 patients; and Ureaplasma species in 5 patients. Triple coinfection with H parainfluenzae, N gonorroheae, and C trachomatis was detected in 1 patient.
Information on all antibiotic-resistant strains of Haemophilus species isolated from patients is provided in Table 2. Eight patients were sensitive to all drugs tested, and all cases that were resistant to tetracycline (10 patients) were also resistant to azithromycin. Seventeen patients (44.7%) were treated empirically with a combination of intramuscular ceftriaxone (250 mg) and a single oral dose of azithromycin (1 g), and 12 patients (31.5%) were treated with a combination of intramuscular ceftriaxone (250 mg) and oral doxycycline (100 mg every 12 h) for 7 days. The remaining patients were treated with azithromycin (5 patients) or doxycycline (4 patients) in monotherapy. In total, 21 patients (55.2%) were lost to follow-up. Microbiological eradication of the pathogen was confirmed in the 17 patients (44.8%) who attended follow-up visits, although 6 required treatment with a second, distinct antibiotic, which was selected according to antibiogram results. Of the 21 patients lost to follow-up, 4 (19%) were carriers of Haemophilus species that were resistant to the empirical treatment prescribed at the first visit according to antibiogram results.
Antibiotic Resistance of Isolated Haemophilus Species
| Antibiotic Tested | Number of Resistant Cases (%) |
|---|---|
| Cotrimoxazole | 20 (53.6) |
| Azithromycin | 13 (34.2) |
| Tetracyclines | 10 (26.3) |
| Amoxicillin | 8 (21) |
| Cefotaxime | 1 (2.6) |
| Ceftriaxone | 3 (7.9) |
| Cefuroxime | 3 (7.9) |
| Ciprofloxacin | 6 (15.8) |
| Levofloxacin | 1 (2.6) |
Of the patients diagnosed with microbiologically confirmed urethritis in our STI Unit, we detected Haemophilus species in urethral exudate samples from approximately one third, a greater proportion than that previously reported in Spain.4
H influenzae and H parainfluenzae are microorganisms commonly found in the normal microflora of the human upper respiratory tract.5 Urethritis caused by these microorganisms has been described in patients with STIs. The last decade has seen an increase in the incidence of urethritis caused by Haemophilus species, especially among MSM, owing to an increase in the practice of unprotected oral sex within this group.6 Because this microorganism has been detected in the urethra of 3% to 9.3% of asymptomatic men,6 its role as a causative agent of urethritis is controversial. We identified Haemophilus species as the sole causative agent of urethritis in 15 of 38 patients (39.5%). A previous study reported detection of Haemophilus species in up to 53% of urethritis patients.4 In our study, 57.9% of patients presented with purulent urethral syndrome that was characterized by spontaneous abundant whitish-green suppuration and was clinically indistinguishable from GU (Fig. 2). In 36.7% of our patients, a Haemophilus species was the only etiological agent isolated, suggesting that this microorganism was the causative agent of acute urethritis in these patients.
H parainfluenza was isolated in 84.2% of our patients, and H influenzae in only 13.2%. These proportions, and the distribution of Haemophilus species among MSM described here, are similar to those previously reported,4 and demonstrate that Haemophilus species are etiologic agents of urethritis mainly among MSM, owing to the low level of condom use during orogenital sexual practices within this group.
Of particular interest was the resistance of the isolated microorganisms to multiple antibiotics. This finding suggests that extra caution is required when selecting empirical adjuvants to intramuscular ceftriaxone when treating urethritis patients. Of the pathogens isolated in our study, 53.6% were resistant to cotrimoxazole and 34.2% were resistant to azithromycin. Furthermore, 26.3% of cases were resistant to both azithromycin and tetracyclines, both of which are recommended first-line drugs for the treatment of NGU.7 While greater proportions of antibiotic-resistant strains have been reported elsewhere, particularly for azithromycin resistance in East Asia,8 monitoring of these patients is nonetheless necessary owing to the high risk of treatment failure. Another drug combination that may be of interest in clinical practice is amoxicillin and clavulanic acid, against which we detected no resistance. We found only 7 cases of resistance to quinolones, suggesting that drugs of this class may be useful adjuvants for the treatment of urethritis, although higher rates of resistance have been reported among MSM patients with urethritis.9 It should be noted that 5 of the H parainfluenzae isolates showed resistance to 5 or more of the drugs tested, and were therefore considered multidrug-resistant.10 It is thus fundamental to confirm microbiological cure and to remind patients of the importance of follow-up visits.
Limitations of this study include its observational nature and the lack of a control group, which would be required to demonstrate a true pathogenic role of Haemophilus species in urethritis. Furthermore, it is difficult to draw precise conclusions regarding the therapeutic outcomes owing to the small sample size and the large number of cases lost to follow-up. It is also unknown whether antibiotic treatment was effective in patients in whom antibiotic-resistant Haemophilus species were isolated but who were subsequently lost to follow-up.
In summary, our findings underscore the importance of Haemophilus species as an etiological agent of NGU, especially among MSM patients with a history of unprotected oral sex. Patients may present with urethral discharge similar to that caused by N gonorrhoeae, and cure must be confirmed owing to the possibility of Haemophilus species antibiotic resistance. Although in theory this ailment is easily treated, dermatologists must take responsibility for the management of urethritis and other STIs.
In this study we describe the presence of Haemophilus species in the urethral exudate of approximately one third of patients diagnosed with microbiologically confirmed urethritis in our STI Unit, a greater proportion than that reported to date in Spain.4
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Magdaleno-Tapial J, Valenzuela-Oñate C, Giacaman-von der Weth MM, Ferrer-Guillén B, Martínez-Domenech Á, García-Legaz Martínez M, et al. Haemophilus Species Isolated in Urethral Exudates as a Possible Causative Agent in Acute Urethritis: A Study of 38 Cases. Actas Dermosifiliogr. 2019;110:38–42.