We report the case of an elderly man with a granulomatous variant of chronic pigmented purpura who presented with papular lesions on the lower legs.
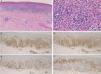
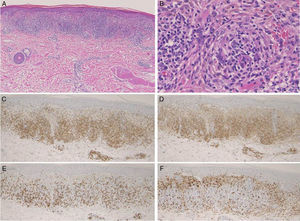
A 78-year-old Japanese man complained of asymptomatic eruptions of 2 years’ duration on his lower legs. He had no history of systemic granulomatous disease and had not taken any drugs. Physical examination showed a number of purpuric papular lesions on both shins (Fig. 1A and B). The lesions were tiny, ranging from the size of a pinhead to 5mm, and were both isolated and arranged in clusters. Laboratory data, which included blood cell counts, biochemical liver and renal function tests, and lipid, cholesterol, and triglyceride levels were normal. Histologic examination revealed extravasation of red blood cells, hemosiderin deposition, and dense inflammatory cell infiltration in the upper dermis (Fig. 2A). The infiltrate was composed of mononuclear cells, histiocytes, and giant cells (Fig. 2B), and immunohistochemistry revealed a number of CD3+ T cells, with a predominance of CD4+ cells. There were also CD8+ T cells scattered among the granulomatous lesions (Fig. 2C–E) and abundant CD68+ cells at the periphery of the cellular infiltrates (Fig. 2F). Vasculitis was not observed. Special stains for microorganisms were all negative. The purpuric lesions were resistant to treatment with topical corticosteroids.
Several cases of granulomatous pigmented purpura have been described since the entity was first reported by Saito and Matsuoka.1 Most of the cases have involved Asian people, but there have been few reports from Japan.2 Although the clinical features described in the original report included lichen aureus-like brown coalesced hemorrhagic papules on the dorsum of the feet,1 additional features such as macules, papules, plaques, and pigmentation have been reported. Apart from the typical clinical features of chronic pigmented purpura, our patient also had a number of papular lesions on both shins, similarly to a previously reported case.3 The age of the patients with granulomatous pigmented purpura described in the literature ranges from 22 to 78 years old (present case), with disease duration varying from 2 months to 20 years. In addition to the lower extremities, there have also been rare reports of lesions on the wrists,4 forearms, and lower back.5
In our case, histologic features showed dense cellular infiltrates composed of lymphocytes and histiocytes in the upper dermis. CD4+ cells were predominant among the CD3+ T cells, C, and CD68+ histiocytes surrounded the cellular infiltrates in the upper dermis. What triggered the granulomatous reaction is not clear, but the long-term chronic course may have had a role. Hyperlipidemia has been reported in several cases,6 and other studies have suggested that lipid microdroplets may induce an inflammatory reaction of the microvasculature.3 Drugs have also been suggested as possible triggers and have been implicated as causative factors of pigmented purpura. In addition, there have been reports of an association with antinuclear antibody and rheumatoid factor positivity, and regulatory T cells were attributed a possible role in the induction of granulomatous changes in pigmented purpura in a patient with Sjögren syndrome.2 In our case, associations with systemic autoimmune diseases, hyperlipidemia, and drug intake were all ruled out. Further studies are necessary to investigate the triggering events and etiology of granulomatous reactions in pigmented purpura.