Neuroradiology intervention techniques are increasingly used for treatment and diagnostic purposes, but reports of adverse cutaneous effects are rare. Herein we report a case of transient alopecia related to endovascular procedures.
A previously healthy 26-year-old woman experienced sudden onset of severe occipital headache associated with vomiting approximately 3h prior to admission to the emergency room. The neurological examination revealed anisocoria and mild neck rigidity. The patient had no history of trauma or other symptoms.
A computed tomography scan showed a subarachnoid hemorrhage in the posterior fossae and a digital subtraction angiography revealed an aneurysm of the basilar artery.
The patient underwent 3 fluoroscopically guided angiographies, which resulted in successful endovascular coiling of the aneurysm. She recovered, without neurologic sequelae, within 2 days of these procedures, which in total lasted approximately 4h. The cumulative radiation dose was 5Gy.
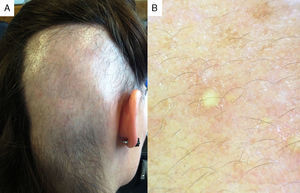
One week after the last angiography, the patient developed a sharply delineated rectangular alopecic area measuring 15×9cm on the right occipital-parietal region of the scalp. The bald patch was devoid of inflammatory signs and scaling (Fig. 1A), and the pulses of the occipital and superficial temporal arteries were bilaterally palpable. The results of the pull test were unremarkable.
Trichoscopy of the alopecic area revealed marked sparseness of terminal hairs and the presence of several vellus-type hairs and yellow dots. No dystrophic hairs or black dots were observed (Fig. 1B).
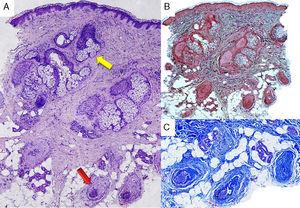
The histopathological examination of a biopsy specimen from the affected area revealed miniaturized hair follicles surrounded by fibrosis and atrophy of the sebaceous glands (Fig. 2).
Skin specimen biopsy of alopecic area. (A) Normal epidermis with no inflammatory infiltrate. Miniaturized hair follicles (red arrow), atrophy of the sebaceous glands (yellow arrow) (hematoxylin eosin, original magnification 100×). (B) Normal dermal elastic fibers (orcein, original magnification 40×). (C) Perifollicular fibrosis (trichome, original magnification 100×).
Radiation and pressure-induced types of alopecia, as well as alopecia areata and trichotillomania, were considered in the differential diagnosis. However, radiation-induced hair loss was the most plausible cause in the clinical setting of the patient. After 3 months of follow-up without treatment, the hair had regrown completely (Fig. 3).
Radiation-induced alopecia after fluoroscopically guided interventional procedures is a form of radiodermatitis.1,2 As occurred in our patient, exposure to a relatively low dose of radiation (3–7Gy) can lead to transient epilation caused by damage to the actively dividing matrix cells of the anagen hair follicles.1,3 Anagen effluvium develops within several days or weeks, and is usually followed by transient miniaturization of anagen hairs and the emergence of broken hairs as a result of the loss of follicle stem cells.1 Furthermore, the premature catagen entry of follicles in late anagen can also trigger observable telogen shedding 2.5–4 months after exposure.4 As occurred in our case, hair regrowth generally occurs 2–4 months after low radiation dose exposure and therefore no treatment is currently indicated. Nevertheless, permanent alopecia can be expected after radiation doses above 7Gy.2
Temporary alopecia following therapeutic embolization of aneurysms, arteriovenous malformations, and tumors has been previously reported.4–10 The complexity of posterior circulation aneurysm coiling procedures, such as those performed in our patient, has been linked to longer fluoroscopy time, increasing the risk of radiation-induced skin damage.8 Cumulative radiation dose, intervals between sessions, total irradiated area, and variations in the incidence angle are important determinants of injury severity.1 In our patient, the location and geometric configuration of the bald patch are consistent with prolonged radiation exposure in the same area with limited variation of the direction of application during the fluoroscopically guided interventions.
Our report emphasizes the need for awareness of the risk of alopecia originating from fluoroscopically guided techniques. While rare and probably underdiagnosed, this adverse effect may increase in incidence due to the growing use of minimally invasive endovascular procedures for the diagnosis and treatment of neurovascular disorders.
We thank E. Rios MD and J.M. Lopes PhD, from the Department of Pathological Anatomy, Centro Hospitalar São João EPE in Porto, Portugal and IPATIMUP (Instituto de Patologia e Imunologia Molecular da Universidade do Porto) in Porto, Portugal for providing the histologic images.