A 39-year-old woman from Guatemala with a history of myomatosis presented with an asymptomatic nodular lesion of 2 years’ duration in the right frontal region; the nodule had grown progressively and changed size on exertion. The patient denied trauma in the area and was in good general health.
Physical ExaminationPhysical examination showed a firm, fixed lesion that was pulseless on palpation in the right frontal region (Fig. 1).
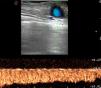
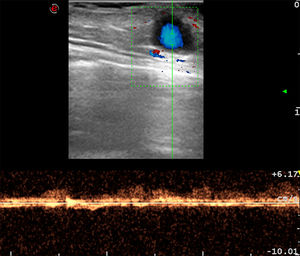
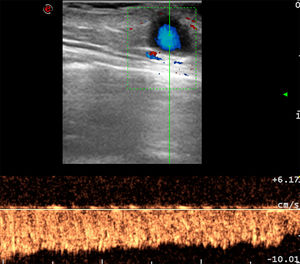
Additional TestsBased on the initial clinical suspicion of an epidermoid cyst or frontal lipoma, we performed a skin ultrasound examination using a linear transducer with a variable frequency of 10 to 22MHz. Scanning of the dermis-hypodermis in the longitudinal axis showed a well-delimited, hypoechogenic ovoid lesion with a diameter of 5mm with posterior reinforcement and an edge shadowing artifact. On the longitudinal axis, the lesion had a uniform, fusiform morphology.
Color Doppler ultrasound showed vascularization in the center of the lesion (Fig. 2). Pulsed-wave Doppler showed turbulent flow. The patient was asked to perform the Valsalva maneuver during the examination and we observed a noticeable increase in velocity in the Doppler spectrum (Fig. 3).
What Is Your Diagnosis?
DiagnosisFrontal phlebectasia.
Clinical Course and TreatmentThe lesion was surgically removed through ligation and excision. Complete excision was confirmed by ultrasound and a histologic examination was performed.
CommentA phlebectasia is a saccular or fusiform dilatation of a vein without tortuosity. The clinical presentation is generally that of a round, painless, pulseless mass with a smooth contour that does not affect the skin surface.1 Phlebectasias become apparent or grow in size with strain, crying, sneezing, coughing, or the Valsalva maneuver, and disappear or decrease in size when the patient is calm.2
Most cases of phlebectasia of the head and neck in the literature have involved the jugular vein.3 Jugular vein ectasia has been associated with connective tissue disorders, such as Menkes disease.4
Diagnosis by ultrasound tends to show a fusiform dilatation of the affected vein and changes in size during the Valsalva maneuver. The ratio between size at rest to size during the maneuver is approximately 1.5 to 2:1.5 Ultrasound can also be used to investigate thrombi and response to external compression. Color Doppler flow imaging shows turbulent vascular flow in the affected segment.5
Procedures such as fine needle aspiration and drainage should be avoided in phlebectasia due to the risk of complications.
Lesion growth and potential complications can be monitored by ultrasound. Surgery is indicated in cases of thrombi, phlebitis, aesthetic deformity, and rupture.5
We believe that phlebectasia of the head and neck is underdiagnosed and ultrasound skin imaging is very useful for diagnosis, evaluation of complications, and postsurgical and longer-term follow-up. The present case also shows that systematically using color Doppler to study dermatological lesions is a valuable technique for establishing a correct diagnosis.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Catalán Griffiths A, Alfagueme Roldán F, Salgüero Fernández I, Ragusa MG. Tumoración frontal que aumenta de tamaño con maniobra de Valsalva. Actas Dermosifiliogr. 2019;110:e7–e8.