A 57-year-old woman with hypertension (in treatment with enalapril) and without any known drug allergies or family history of interest attended our dermatology clinic for diffuse hair loss with onset 1 year earlier and inflammatory plaques that had recently appeared in the alopecic areas.
Clinical examination of the scalp revealed a slightly receding frontal hairline, isolated or lonely hairs, of different diameters, perifollicular hyperkeratosis, and mild erythema (Fig. 1A). The patient also showed hair loss on the arms and total alopecia of the eyebrows although the eyelashes were unaffected (Figs. 1B and C). Trichoscopy of the frontal area showed white patches, arborizing vessels, hairs of different diameters, and follicular hyperkeratosis (Fig. 1D). Atrophic plaques of alopecia with areas of erythema and inflammation were present in temporal and occipital regions (Fig. 2A). Trichoscopy of the temporal area showed the presence of red dots, white cicatricial patches, prominent branched capillaries (megacapillaries), and keratin plugs (Fig. 2B).
Facial papules and frontal vein depression were not present. She did not have skin lesions in other regions or nail or mucosal lesions.
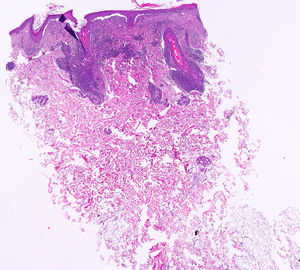
Histopathological examination of a biopsy taken from the inflammatory area of the parietal area showed the presence of chronic perifollicular and periadnexal inflammatory infiltrate with vacuolar thickening and degeneration of the basal layer and mucin deposition consistent with discoid lupus erythematosus (DLE) (Fig. 3). Direct immunofluorescence (DIF) was positive for immunoglobulin G and C3 with depositions throughout the basement membrane of the skin of affected areas of the scalp and follicular epithelium. Histology of the frontal alopecic region showed a dense chronic lichenoid infiltrate with interface dermatitis in the area of the follicular epithelium free of mucin. DIF was negative.
Complementary tests, including hematology workup, general biochemistry, antinuclear antibodies and extractable nuclear antigens, thyroid hormones, proteinogram, and complement reported normal values.
The simultaneous presence of frontal fibrosing alopecia (FFA) and DLE is an association rarely described in the literature. This association has been reported more frequently in women,1 although cases have been occasionally reported in men.2 FFA is a lymphocytic primary cicatricial alopecia of growing importance given its increasing prevalence in recent years, as reflected by the large number of articles published recently about its clinical presentation, diagnosis, and treatment. The most recent lines of investigation point to pathogenesis and pathophysiology related to application of certain hair products and sunscreens. We should also not forget the theories that point to a clear hormonal imbalance, more frequent in postmenopausal women, in the development of this disease. Recently, new diagnostic criteria have been proposed to facilitate identification of this condition. These are divided into major criteria (frontal or temporal cicatricial alopecia without keratotic papules on the body and diffuse and bilateral alopecia of the eyebrows) and other minor criteria (typical trichoscopy, occipital involvement, facial or body hair, and facial papules).3 Our patient presented with 2 major criteria and 2 minor ones. Likewise, severity scales have been validated4 and the trichoscopic features have been defined in large series of patients led by Spanish working groups.5
Although the association of FFA with other types of alopecia has been reported several times in the literature, no series have been published of cases that study the characteristics of these patients. An association has been reported with lichen planopilaris,6 androgenic alopecia,7 and DLE.1,2,8 Not all patients with both types of cicatricial alopecia (FFA and DLE) have a history of cutaneous lupus erythematosus.2 Our patient was also taking enalapril among her medications. This drug has been linked to lichenoid eruptions9 and cutaneous lupus.10 We could not find any cases in the literature supporting a relationship with FFA.
In the context of cicatricial alopecia, DLE and FFA show subtle histologic differences based on presence or absence of mucin and differences in the characteristics of the lymphocytic infiltrate. In DLE, there is a greater lymphoplasmacytic predominance and presentation is usually at perifollicular, perivascular, and adnexal sites, whereas FFA is usually confined to perifollicular presentation.11 However, it seems clear that concurrent presentation should point us to the presence of a common immunological pathway of the innate type that is responsible for the appearance of both processes in genetically predisposed individuals.
The use of hydroxychloroquine or chloroquine as monotherapy does not appear to be effective as therapy.8 We should proceed to joint treatment of both entities using topical/intralesional corticosteroids and the combination of antimalarial agents with 5-alfa-reductase inhibitors to ensure a more complete therapeutic coverage in these patients.12
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Fernández-Crehuet P, Ruiz-Villaverde R. Alopecia frontal fibrosante y lupus eritematoso discoide: más allá de la coexistencia. Actas Dermosifiliogr. 2019;110:419–420.