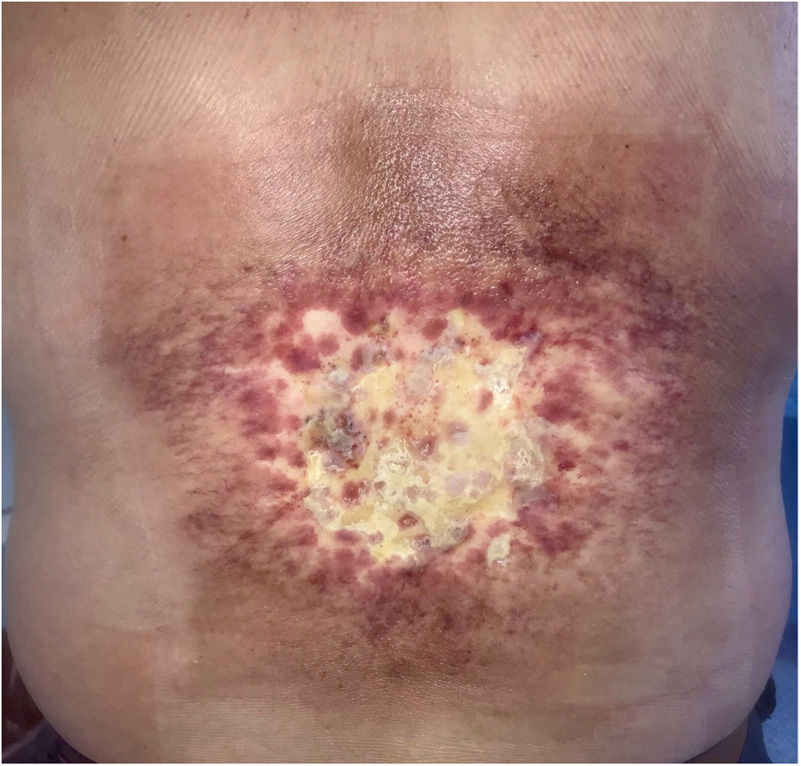
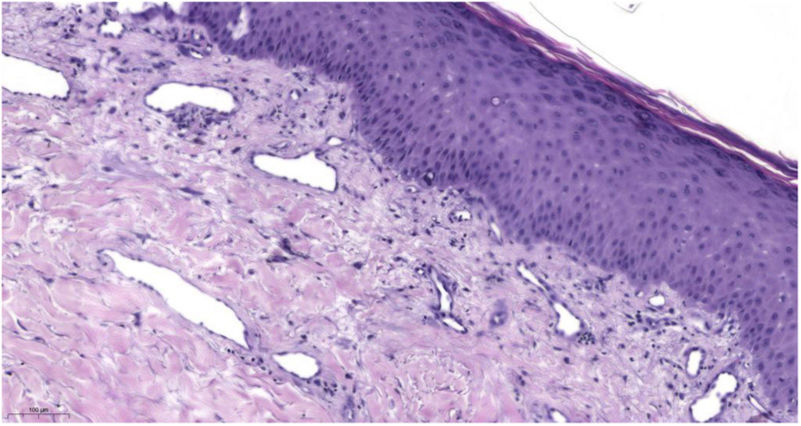
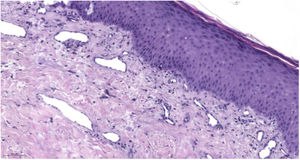
A 57-year-old man was referred to dermatology for assessment of a hyperpigmented sclerodermiform plaque measuring 30 × 20cm in the form of an exudative ulcer with indurated borders surrounded by a poorly defined erythematous area. The plaque was located on the lower back and had first appeared 5 months previously (Fig. 1). The patient had a personal history of type 2 diabetes mellitus and arterial hypertension and had recently been diagnosed with myelolipoma. This was treated with superselective embolization of the right phrenic artery, right suprarenal artery, and L2 lumbar artery 6 months before attending the clinic. The patient reported having initially experienced pruritus and reddening of the dorsolumbar region some 15 days after the operation. The lesion subsequently began increasing in size and became ulcerated. Histology only revealed enlarged lymph nodes caused by radiotherapy (Fig. 2).
After a review of the literature and taking into account the history of transarterial embolization and the characteristics and location of the skin lesion, the patient was diagnosed with fluoroscopy-induced radiation dermatitis. Diagnosis is based mainly on clinical findings. Fluoroscopy is an imaging modality used for real-time assessment of the movement of internal body systems and apparatuses. As is the case when obtaining x-ray images, the minimum necessary exposure for all types of images depends on the specific information required or to be analyzed. Therefore, the time needed to form series of images may be long. Most procedures of this type do not induce skin lesions, although in more complex cases, the risk of fluoroscopy-induced radiation dermatitis is increased by the greater frequency of sessions, longer exposures (doses >15Gy), and new indications for these therapeutic interventions.