A 78-year-old woman presented lesions on the palms and soles that caused discomfort because they were exposed to constant friction. The lesions had first appeared several years earlier. The patient had a history of osteoarthritis, systemic hypertension, dyslipidemia, and atrial fibrillation. She was on treatment with acenocoumarol, carvedilol, atorvastatin, metamizol, paracetamol, and omeprazole.
Physical ExaminationPhysical examination revealed multiple brownish, filiform hyperkeratotic papules measuring only a few millimeters. The lesions were distributed across the entire surface of the palms (Fig. 1) and less densely on the soles.
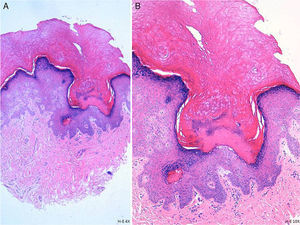
HistopathologyA 2mm punch biopsy that included a complete lesion was taken from one of the patient's palms. Histology revealed a column of parakeratosis in the stratum corneum with underlying focal hypogranulosis and a depressed epidermis (Fig. 2).
What Is Your Diagnosis?
DiagnosisSpiny keratoderma or filiform hyperkeratosis of the palms and soles.
Clinical Course and TreatmentBlood tests with tumor markers, chest radiograph, and abdominal ultrasound were requested. The only relevant findings were hepatic steatosis and the presence of renal cysts. Treatment with 0.1% tretinoin and 40% urea cream obtained a poor results. On further interrogation, the patient reported that several of her relatives had similar problems of “spines” on the hands.
CommentSpiny keratoderma is a rare condition; only around 30 cases have been reported in the literature. Most cases are acquired but there are also familial cases,1 like that of our patient. This skin condition is characterized by the appearance of small, filiform hyperkeratotic lesions distributed across the surface of the palms and/or soles.1 The lesions resemble the spines of an old-fashioned music box cylinder.2 Although they are usually asymptomatic, the lesions can make manual labor difficult and cause pain on pressure or walking. The condition is chronic and spontaneous remissions are rare.2
Spiny keratoderma can be hereditary, with an autosomal dominant inheritance pattern and onset in the second or third decades of life, or sporadic, with onset at a later age. In either case, it is more common in men.3
Histologically, spiny keratoderma is characterized by a compact, cornoid lamella–like column of parakeratosis that is clearly separated from the normal stratum corneum and the underlying granular layer is thin or absent.1 Like porokeratotic eccrine ostial and dermal duct nevi, the lesions are occasionally associated with hair follicles and acrosyringia.4
Spiny keratoderma has been found in association with various diseases, including polycystic kidney and liver disease, Darier disease, tuberculosis, epidermodysplasia verruciformis, and neoplasms. It was originally considered to be a paraneoplastic syndrome, but today, the most widely accepted opinion is that there is no clear association between spiny keratoderma and other diseases. Clinically and histologically, it is considered to be a distinct entity that should not be mistakenly identified as a variant of either punctate keratoderma or porokeratosis, which have respectively been associated with internal and cutaneous malignancies.
The pathogenesis of spiny keratoderma is poorly understood. It has been suggested, on the basis of the keratin patterns found in the column of parakeratosis, that it may be caused by anomalous ectopic hair formation.1
Spiny keratoderma has been treated with numerous agents, including topical and oral retinoids, emollients containing salicylic acid, urea, ammonium lactate, propylene glycol, and 5-fluorouracil5; the results have been variable.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Hiraldo-Gamero A, Gordillo Chaves J. Pápulas filiformes palmoplantares. Actas Dermosifiliogr. 2013;104:819–820.