Cutaneous larva migrans is a parasitic disease caused by the penetration of hookworms that migrate across the epidermis. It usually occurs when the skin comes into contact with soil contaminated with animal feces containing these worms. The vast majority of larva migrans cases are imported from tropical or subtropical countries, and very few autochthonous cases have been reported in Europe.1 Six recent cases have been reported in Spain (in Burgos, Gipuzkoa, and Asturias).2–4 We describe what we believe is the first case of autochthonous larva migrans in the autonomous community of Cantabria in northern Spain.
A 4-year-old girl presented in early summer with a 5-day history of a pruritic, migratory cutaneous lesion in the nasal region. The girl's mother confirmed that they had not travelled outside Cantabria in the past few months but mentioned that her daughter had been in contact with sand at a local beach on several sunny days. The skin examination showed an erythematous, slightly raised, serpiginous lesion on the nasal dorsum extending into the left paranasal region (Fig. 1). In view of these characteristic findings, we established a diagnosis of larva migrans and started treatment with albendazole 400mg/d for 3 days. The lesion improved gradually and cleared completely within a week.
Ancylostoma braziliense is the main parasite responsible for cutaneous larva migrans. Most hookworm species live in warm, wet climates and are therefore found more often in the digestive system of animals (mainly dogs and cats) living close to the equator.1
Diagnosis is essentially clinical and is based on the detection of pruritic, serpiginous lesions that creep forward at one end. The larva is located approximately 1 or 2cm ahead of the advancing lesion and biopsy samples are therefore unlikely to show parasite structures.3 Cutaneous larva migrans mainly affects the lower extremities and is generally more common in children than in adults.5 There have been very few reports of lesions involving the face.6
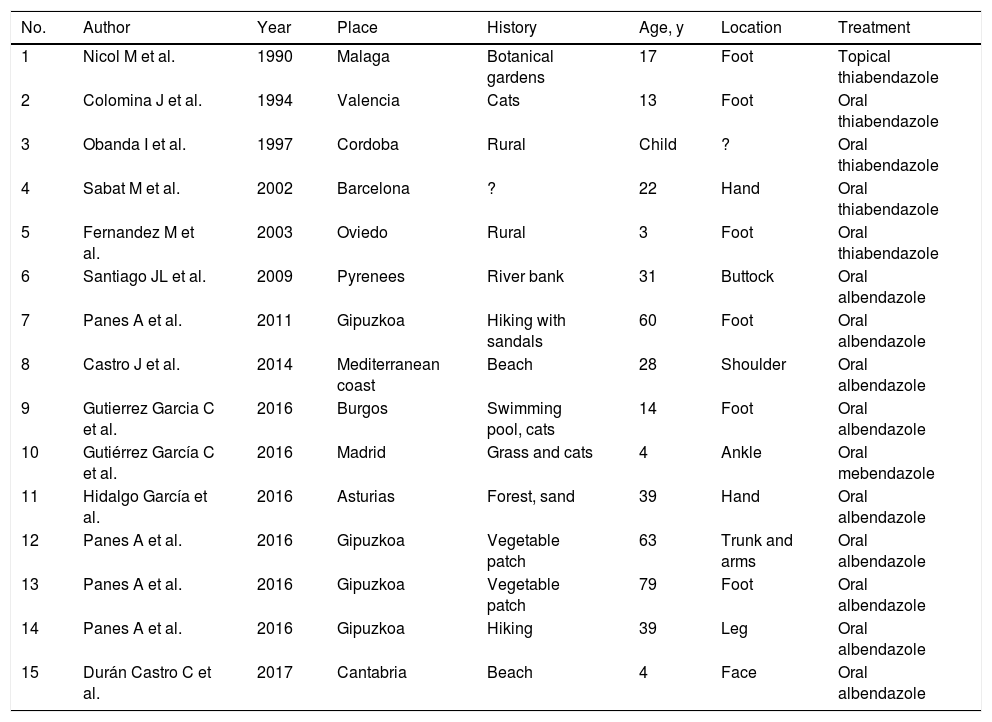
The current case prompted us to review the literature, dating mainly from the past decade, in search of other autochthonous cases. We identified 15 cases (Table 1), none involving the face. One interesting observation is that all the recent cases were from the north of Spain.3,4 It is also noteworthy that over 20 autochthonous cases of larva migrans have been reported in Europe in recent years,2 suggesting that the temperate ocean climate might be conducive to the biological cycle of these nematodes.
Autochthonous Cases of Larva Migrans in Spain Between 1990 and 2017.
| No. | Author | Year | Place | History | Age, y | Location | Treatment |
|---|---|---|---|---|---|---|---|
| 1 | Nicol M et al. | 1990 | Malaga | Botanical gardens | 17 | Foot | Topical thiabendazole |
| 2 | Colomina J et al. | 1994 | Valencia | Cats | 13 | Foot | Oral thiabendazole |
| 3 | Obanda I et al. | 1997 | Cordoba | Rural | Child | ? | Oral thiabendazole |
| 4 | Sabat M et al. | 2002 | Barcelona | ? | 22 | Hand | Oral thiabendazole |
| 5 | Fernandez M et al. | 2003 | Oviedo | Rural | 3 | Foot | Oral thiabendazole |
| 6 | Santiago JL et al. | 2009 | Pyrenees | River bank | 31 | Buttock | Oral albendazole |
| 7 | Panes A et al. | 2011 | Gipuzkoa | Hiking with sandals | 60 | Foot | Oral albendazole |
| 8 | Castro J et al. | 2014 | Mediterranean coast | Beach | 28 | Shoulder | Oral albendazole |
| 9 | Gutierrez Garcia C et al. | 2016 | Burgos | Swimming pool, cats | 14 | Foot | Oral albendazole |
| 10 | Gutiérrez García C et al. | 2016 | Madrid | Grass and cats | 4 | Ankle | Oral mebendazole |
| 11 | Hidalgo García et al. | 2016 | Asturias | Forest, sand | 39 | Hand | Oral albendazole |
| 12 | Panes A et al. | 2016 | Gipuzkoa | Vegetable patch | 63 | Trunk and arms | Oral albendazole |
| 13 | Panes A et al. | 2016 | Gipuzkoa | Vegetable patch | 79 | Foot | Oral albendazole |
| 14 | Panes A et al. | 2016 | Gipuzkoa | Hiking | 39 | Leg | Oral albendazole |
| 15 | Durán Castro C et al. | 2017 | Cantabria | Beach | 4 | Face | Oral albendazole |
Environmental parasitology studies have identified changes in the frequency and geographic distribution of hookworms, probably in response to climate change and the “tropicalization” of the European climate.7,8
In conclusion, this new case of cutaneous larva migrans in Spain highlights the need to establish opportune preventive measures to prevent a greater incidence of autochthonous cases.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Durán-Vian C, Vilanova-Udaniz I, Castro-Gutierrez B, González-López MA. Larva migrans cutánea facial de origen autóctono en España. Actas Dermosifiliogr. 2018;109:659–660.