Extramammary Paget disease (EMPD), first described by Crocker1 in 1889, is a form of intraepidermal adenocarcinoma that generally occurs in areas with a high density of apocrine glands. It presents as a scaly, erythematous lesion simulating inflammatory conditions, tumors, and infections. Isolated cases that occur in locations where there are usually no apocrine glands are called ectopic EMPD.2 We report a case of EMPD in the right frontotemporal region, which is only the third case of EMPD affecting the face that has been reported in the literature (Table 1).2,3
Literature Review of Cases of Extramammary Paget Disease Affecting the Face.
| Case | Author | Age/Sex | Clinical Diagnosis | Size | Location | Treatment |
| 1 | Chilukuri,2 2002 | 67/man | Bowen | 15×20 cm | Cheek | Mohs chemotherapy |
| 2 | Cohen,3 2004 | 61/man | -- | 2×1 cm | Right temporal region | Photodynamic therapy |
| 3 | Córdoba, 2011 | 64/woman | Bowen/seborrheic dermatitis | 5×6 cm | Right temporal region | Photodynamic therapy |
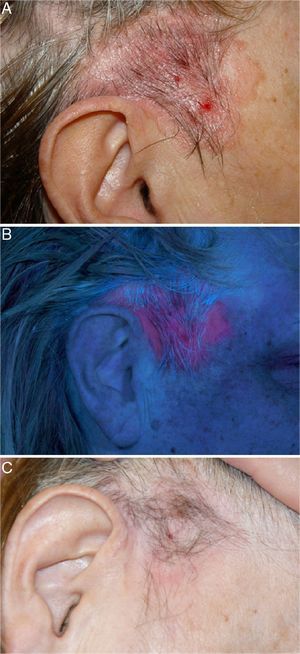
A 64-year-old woman presented with a plaque measuring 5cm in the right frontotemporal region that extended into the preauricular region; the lesion had appeared 3 years earlier. The plaque had an erythematous, slightly scaly center and slightly pigmented borders (Fig. 1A). A diagnosis of intraepidermal squamous cell carcinoma or seborrheic dermatitis was made and treatment with corticosteroids resulted in a slight improvement.
A, Erythematous plaque measuring 5cm located in the right temporal region and extending towards preauricular hairless skin, with a periphery marked by linear pigmentation. B, Plaque displaying intense red fluorescence after a 3-hour incubation period with methyl aminolevulinate. C, Complete remission 2 months after the second photodynamic therapy session.
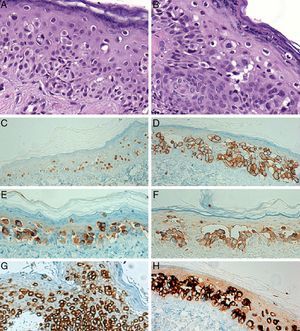
Histologic study of 2 biopsies, 1 from the center and 1 from the edge of the lesion, revealed the occupation of the epidermis by a population of large cells with clear cytoplasm and atypical nuclei, arranged singly or in nests and accompanied by little melanin pigment. These cells had spread to the adnexa but there was no dermal infiltration (Fig. 2 A and B). The atypical cells occupying the epidermis were positive for cytokeratin 7 (Fig. 2G) and cytokeratin CAM 5.2, but these markers were not expressed in the surrounding epidermis. The nuclei tested positive for estrogen receptors (Fig. 2C). Her2 membrane expression was intense and continuous (Fig. 2D). Other positive markers were carcinoembryonic antigen (Fig. 2E), gross cystic disease fluid protein 15 (Fig. 2H), and MUC-1 (Fig. 2F). The lesion was S-100 negative. These findings led to a diagnosis of ectopic EMPD.
A and B, Histologic images of the lesion showing isolated clear cells in the epidermis (hematoxylin-eosin, original magnification ×400). C, Nuclear expression of estrogen receptors in the atypical cells (hematoxylin-eosin, original magnification ×200). D, Intense Her2 membrane staining (hematoxylin-eosin, original magnification ×200). E, The intraepidermal tumor cells were positive for carcinoembryonic antigen (hematoxylin-eosin, original magnification ×200). F, Cytoplasmic staining for MUC1 (hematoxylin-eosin, original magnification ×200). G, Cytoplasmic staining for cytokeratin 7 (hematoxylin-eosin, original magnification ×200). H, Gross cystic disease fluid protein 15 is positive in EMPD (hematoxylin-eosin, original magnification ×200).
In view of the size of the plaque, we considered that surgery as a first choice would probably be disfiguring or offer unsatisfactory esthetic results for a 64-year-old patient. Photodynamic therapy was performed in 2 sessions with a week between them. Topical methyl aminolevulinate was applied in accordance with the protocol of the dermatology department. Under Wood light, fluorescence was observed in the lesion (Fig. 1B). A very good response to treatment was observed in the follow-up visit 2 months after the second session of photodynamic therapy (Fig. 1C). The lesion recurred partially 18 months after treatment. We therefore prescribed a second cycle of 2 sessions of photodynamic therapy, which led to a partial response. On the last visit imiquimod treatment was added to the regimen.
EMPD affecting facial skin was first described in 2002 by Chilukuri et al.2 in a 67-year-old male patient who had an erythematous plaque on the cheek that had appeared 10 years earlier and had been treated as Bowen disease. In 2004 another case affecting the face was reported,3 presenting in a 61-year-old man in the form of a pink plaque in the frontotemporal region near the left lateral canthus. In both cases the treatment chosen was Mohs micrographic surgery.The differential diagnosis of EMPD in the frontotemporal area should be established with seborrheic dermatitis, nummular eczema, Bowen disease and, less frequently, with lichen-sclerosus et atrophicus and lichen simplex chronicus. The histological differential diagnosis should be made with other malignancies that occupy the epidermis and are characterized by cells with clear cytoplasm and patchy distribution, mainly superficial spreading melanoma and malignant lentigo, in which case the epithelial markers would be negative and the melanocytic markers (S-100, Melan-A, HMB-45, etc.) positive. P63 can be used to differentiate EMPD from the Pagetoid variant of Bowen disease.4–8
In general, EMPD is only locally aggressive. However, in cases of advanced or metastatic EMPD,7 systemic chemotherapy is indicated.5,7,9
Surgery is the treatment of choice in EMPD.2,3 However, recurrence rates are high even when the lesions are removed with wide surgical margins. Recurrence is probably due to the multifocal nature of the disease and subclinical involvement of skin that is apparently unaffected. Recurrence rates are higher in cases of invasive disease.5,7 The use of Mohs micrographic surgery improves cure rates but does not prevent recurrence. Radiation therapy may be useful as adjuvant therapy in patients at high risk of recurrence.5
Because EMPD has a patchy distribution and the affected area often extends beyond the clinically visible tumor, photodynamic therapy may be a useful treatment when there is intraepithelial involvement and surgery is high-risk or when there is a high risk of morbidity due to the anatomical location of the lesion. However, because of the small number of studies and case reports of patients treated with this technique, photodynamic therapy should only be used when other approaches are not feasible.
We report the third case of EMPD affecting the face (the frontotemporal region). We call attention to the need to include this disease in the list of lesions that simulate other dermatoses and to the fact that its diagnosis requires immunohistochemical evaluation of the usual breast tumor markers. Ours is the first case treated with photodynamic therapy. The patient achieved complete temporary remission, so this treatment may be a good therapeutic option when involvement is exclusively intraepidermal and when a surgical approach is difficult.
Please cite this article as: Córdoba A, et al. Enfermedad de Paget extramamaria con afectación de la región fronto-temporal. Presentación de un caso y revisión de la bibliografía. Actas Dermosifiliogr. 2013;104:355–7.