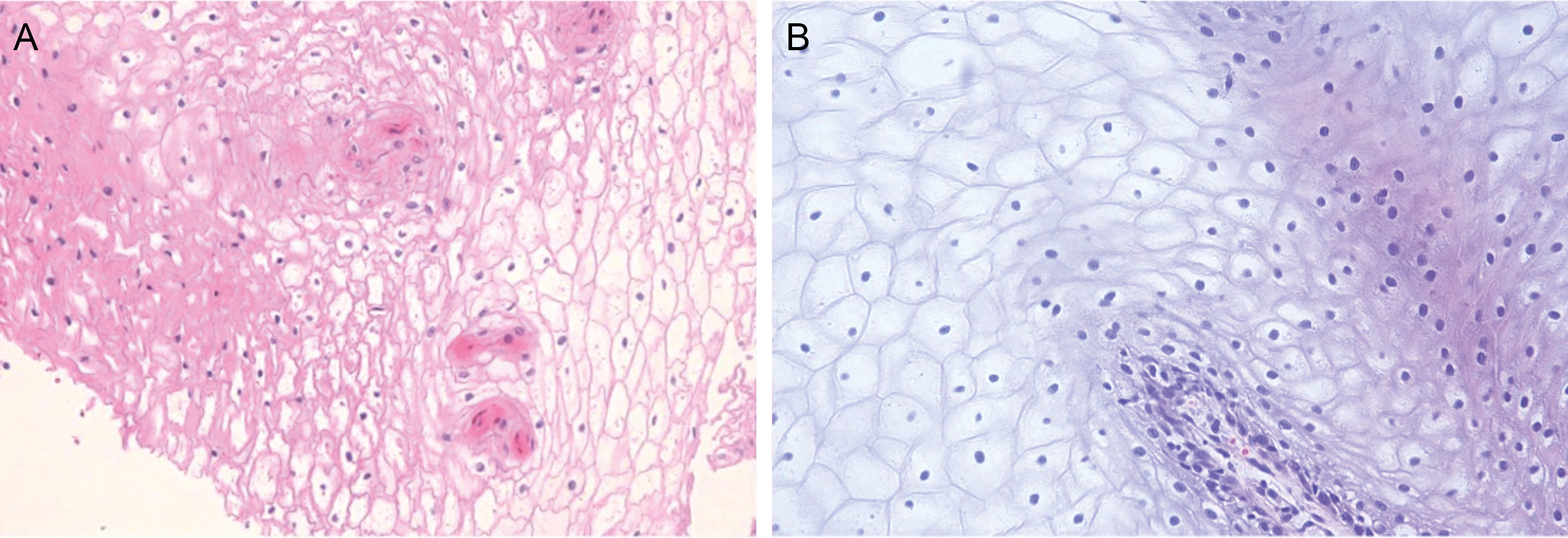
A healthy 5-month-old boy, with no relevant family history and an unremarkable pregnancy and delivery was evaluated due to the presence of whitish plaques located on the external and internal oral mucosa (fig. 1), which the parents reported as congenital. He exhibited a white-yellowish plaque affecting the external labial mucosa, and whitish, velvety plaques that did not detach with friction were observed on the lateral lingual mucosa and buccal mucosa. No other abnormalities were observed in the nails, hair, skin, or mucous membranes. He also did not present with stridor either. Neither parent had similar lesions. A laryngoscopy under sedation ruled out respiratory tract involvement. A biopsy of the buccal lesions revealed the presence of an acanthotic mucosa with clear cytoplasm keratinocytes, intracellular edema, and isolated dyskeratotic cells (fig. 2). No alterations were detected in the molecular study either. For the genetic study, the human exome was sequenced using Illumina DNA Prep with Exome v2.0 PLUS Enrichment with a total coverage of 37.5 Mb from a peripheral blood DNA sample. The Geneyx analysis software was used for tertiary test based on the following HPO phenotypes: nevus, white sponge nevus, and pachyonychia congenita. Additionally, the KRT13, KRT4, KRT6A, and KRT6B genes were specifically reviewed. Based on the clinical-histopathological findings and the absence of other associated signs, a diagnosis of white sponge nevus (WSN) was established.
WSN is a rare disease of autosomal dominant inheritance and variable penetrance and expressivity1,2. Germline mutations in the keratin 4 and 13 genes have been isolated in patients with this condition. Despite this, Liu et al. conducted a molecular study on peripheral blood in 5 patients with sporadic WSN, and only 1 was found to have a mutation in 1 of these cytokeratins, as opposed to the 3 patients with familial WSN analyzed, all of whom had mutations in keratin 4 or cytokeratin 133,4.
The most common location is the buccal mucosa, followed by other parts of the oral or labial mucosa. However, it can also damage the esophagus, respiratory tract, rectum, or genitals. Clinically, it shows as thickened, whitish, bilateral, and symmetrical plaques with a velvety surface that do not disappear with friction2,5. Histopathologically, it is characterized by the presence of acanthosis, hyperparakeratosis, vacuolization of keratinocytes in the suprabasal layers, and ocasionally perinuclear eosinophilic deposits of cytokeratin tonofilaments.
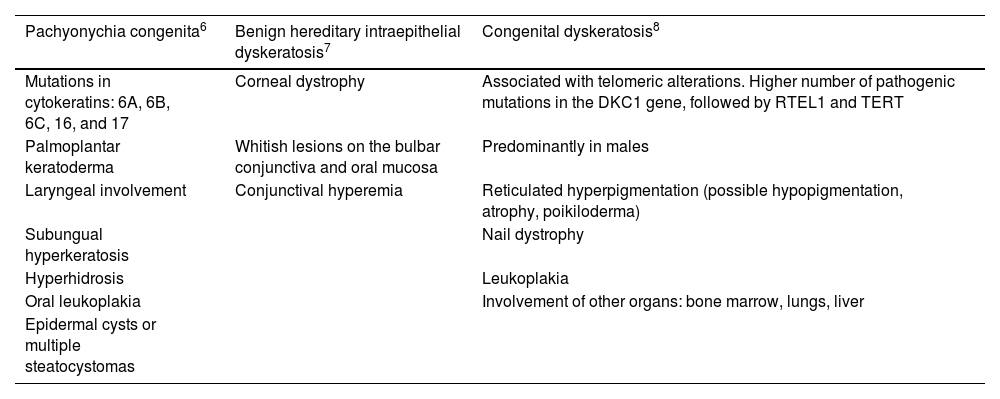
Although WSN often develops in early childhood, with a clinical diagnosis, it can also be detected in adults, for whom histopathological tests are advised to rule out the presence of any other possible etiologies1. In children, candidiasis should be ruled out and differentiated from other entities such as pachyonychia congenita, benign hereditary intraepithelial dyskeratosis, and congenital dyskeratosis (Table 1). If WSN is suspected in adulthood, the differential diagnosis should include lichen planus, squamous cell carcinoma, linea alba, frictional leukoplakia, Darier disease, lupus erythematosus, or secondary syphilis1,2.
Differential diagnosis of leukoplakia in childhood.
| Pachyonychia congenita6 | Benign hereditary intraepithelial dyskeratosis7 | Congenital dyskeratosis8 |
|---|---|---|
| Mutations in cytokeratins: 6A, 6B, 6C, 16, and 17 | Corneal dystrophy | Associated with telomeric alterations. Higher number of pathogenic mutations in the DKC1 gene, followed by RTEL1 and TERT |
| Palmoplantar keratoderma | Whitish lesions on the bulbar conjunctiva and oral mucosa | Predominantly in males |
| Laryngeal involvement | Conjunctival hyperemia | Reticulated hyperpigmentation (possible hypopigmentation, atrophy, poikiloderma) |
| Subungual hyperkeratosis | Nail dystrophy | |
| Hyperhidrosis | Leukoplakia | |
| Oral leukoplakia | Involvement of other organs: bone marrow, lungs, liver | |
| Epidermal cysts or multiple steatocystomas |
Multiple treatments with variable effectiveness for WSN have been described, such as topical or oral tetracyclines, surgery, CO2 laser, beta-carotenes, chlorhexidine rinses, and others. The therapeutic goal is primarily aesthetic since it is a benign and asymptomatic condition2,3.
In conclusion, a sporadic WSN with extensive involvement of the oral mucosa has been described. Notably, there was significant involvement of the external labial mucosa, which is uncommon for this entity.
Conflicts of interestNone declared.