The acquisition of competences (the set of knowledge, skills and attitudes required to perform a job to a professional level) is considered a fundamental part of medical training. Dermatology competences should include, in addition to effective clinical interviewing and detailed descriptions of skin lesions, appropriate management (diagnosis, differentiation, and treatment) of common skin disorders and tumors.
Such competences can only be acquired during hospital clerkships. As a way of certifying these competences, we propose evaluating the different components as follows: knowledge, via clinical examinations or critical incident discussions; communication and certain instrumental skills, via structured workplace observation and scoring using a set of indicators; and attitudes, via joint evaluation by staff familiar with the student.
La adquisición de competencias (conjunto de conocimientos, habilidades y actitudes que conforman la actuación profesional) se considera un requisito necesario para la acreditación del grado de Medicina. Las competencias en Dermatología deberían ser, además de la realización de la entrevista clínica y la descripción precisa de las lesiones cutáneas, el correcto manejo (diagnosticar, diferenciar y tratar) de las dermatosis y tumores comunes. Estas habilidades solo pueden adquirirse durante una rotación especializada. Proponemos que para certificarlas debemos evaluar los conocimientos adquiridos con exámenes clínicos o mediante la discusión de incidentes críticos; mientras que, para la evaluación de las habilidades de comunicación y algunas habilidades instrumentales, podríamos poner en práctica la observación estructurada de la práctica clínica, tras elaborar indicadores para cada una de ellas; y para las actitudes, adoptar un consenso entre los miembros del servicio que han estado en contacto con el estudiante.
Adapting the curricula of Spanish medical schools to the principles of the European Higher Education Area (EHEA) has introduced the concept of competencies into our course syllabi. The EHEA, commonly referred to as the Bologna Process, or plan, was conceived to support freedom of movement for graduates. One consequence is that medical students now spend more hours doing clinical practice.
Not long ago clinical practice was considered a mere complement to undergraduate medical studies, since only knowledge was assessed. Clinical practice hours were often optional and specific learning objectives were not stated. Students accompanied a doctor on rounds or observed office visits and listened while the most important aspects of a case were explained. Learning was passive, and very little of what was available to be learned was absorbed. Today, undergraduate clinical practice clerkships have gained considerable importance through the specification of the competencies medical students must acquire in order to practice in the EHEA. Such clerkships are key to accrediting students’ acquisition of the clinical skills defined in the curriculum.
Some of the most prestigious medical training centers—Maastricht, Dundee, Manchester, and Hamburg for example—began to develop their catalog of basic clinical competencies in the 1990s. In 2001, the medical faculty at the Universitat de Lleida listed 396 skills. The catalog was revised in 2004 and now provides the basis for what students must gather into portfolios reflecting their clerkships. The acquisition of competencies has been enhanced by providing training in some skills in a laboratory setting and then monitoring progress regularly during clerkships within the context of a problem-based approach to education.1
Methods for Assessing Achievement in Clinical ClerkshipsAs competencies have acquired ever greater roles in the accreditation of faculties, a variety of assessment methods have been developed for certifying that a student has met the stipulated requirements. The most effective assessment is based on direct observation of performance, once standards have been set; alternatively, videotapes of the student at work can be evaluated. Medical simulation manikins should ideally be used when a student takes the first steps toward learning a technique in the skills laboratory; when the skill involves patient interaction, the first steps are best taken with professional actors.
The following sections discuss the various assessment methods we emphasize.
Assessment of Knowledge During a Clerkship: Analysis of Critical IncidentsIn keeping with our approach to providing both informative and formative education, we make use of undergraduate clerkships to help students consolidate their knowledge by analyzing critical incidents. Both types of learning can be assessed through this exercise. Candidate incidents are situations that lead the student to pose questions or become aware of a doubt during routine practice and that stimulate learning as a result. It is the analysis of the incident, which includes a detailed description of the event and structured reflection on it in context, that facilitates learning.2 The student notes down a question or doubt when the incident takes place and then enters it into a standard form (Appendix 1, Online Supplementary Material in Spanish). Questions generally refer to what the student knows about the problem at the time of the incident, what needs to be found out and how; together, they give rise to learning objectives. For example, a student faced with a patient hospitalized with chest pain might ask, “How can I tell the difference between coronary chest pain and pain from a pulmonary thromboembolism?” A student seeing a patient who has been running a fever for 3 weeks might ask, “What infectious diseases can cause a long-running fever?” or “What diseases can make a fever so persistent?” The student might even write, “Why is that patient so angry about having to wait a bit before coming into the office?” The student feels motivated to analyze the incident since the reflections have immediate relevance.3 Writing up the analysis is considered important because knowledge is more fully integrated through writing. At the end of the clerkship the student and supervisor can assess the knowledge acquired by analyzing these critical incident reports together.
Observation of an Objective Structured Clinical Examination in the Context of Workplace-Based AssessmentObservation of student–patient interaction in an objective structured clinical examination (OSCE) during the clerkship involves the evaluation of previously specified criteria using a workplace-based assessment (WPBA) approach.4–6 OSCE/WPBA is particularly appropriate for clinical interviews, although it can also be used for diagnostic and therapeutic procedures. Once the visit or procedure is finished, the supervisor gives feedback that leads to both formative and summative assessment.
Objective Structured Assessment of Technical SkillsObjective structured assessment of technical skills (OSATS) is very similar to the previous method but is mainly used to evaluate the student's skill in instrumental procedures according to a checklist of previously established criteria. Once the student has completed the procedure and errors have been noted, the supervisor and student proceed to formative feedback.7
Educational Use of VideotapesVideotapes can be used for the same purposes as direct observation. Analysis of videotapes is retrospective but has the advantage that time is saved because the patient is not present. The supervisor and student analyze a taped interview with a patient, dubbing their comments about deficits and errors onto the tape itself, always for formative purposes. The patient must consent to being taped and, as with direct observation methods, the criteria for assessment must be set beforehand. Videotaping can also be used to analyze surgical competencies and public speaking skills. After students at the University of Dundee were videotaped while suturing in a simulation, they proceeded to self-assessment of the suture using a video dubbing function developed specifically for the study.8 Student self-assessments correlated highly with expert assessments (r=0.83; P<.0001).
AuditsAn audit consists of analyzing patient charts, clinical courses, and reports for summative assessment of the acquisition of training goals. Audits also provide a way to retrospectively assess clinical practice. The supervisor reviews documents written by the student to locate deficiencies and propose changes. When it is the student who examines the collected material, the procedure is a self-audit.
SimulationsManikins can be used for simulations in the skills laboratory or standardized patients (actors) can be trained to play a specific role (a pregnant woman, a patient with hypertension or acute abdomen) to provide students with communication practice. Moulage has even been used to simulate a melanoma9,10 or a psoriatic plaque. The training efficacy of such simulations has been widely studied. One group assessed how well urinary catheter insertion was learned using a pretest, immediate posttest, and a patient-based transfer test of skills a week later.11 The researchers recorded the number of times antisepsis was violated and the assessment of a blinded expert. This study showed that results on the pretest and immediate posttest were similar after computer-assisted learning, peer-assisted learning, and expert-assisted learning, but that transfer of the skill to patient care was significantly better for the group assisted by an expert than for those who learned with either peer or computer assistance. An expert's help, therefore, has a significant effect on the ability of students to transfer skills to real situations.
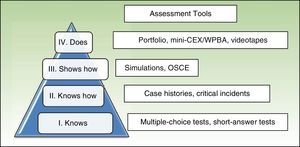
Using Multiple Forms of Evaluation in an Approach to Holistic Assessment of LearningTo evaluate the various dimensions of clinical competence, several assessment methods should be combined, especially if we wish to evaluate the third (“shows”) and fourth (“does”) levels of Miller's pyramid of learning (Fig. 1). Combining complementary approaches has been shown to efficiently assess all aspects of clinical competence.12,13 The 3 tools most widely adopted are observation of an OSCE, the mini-clinical evaluation exercise (mini-CEX), and portfolios.
Miller's pyramid of learning, adapted from Fornells-Vallés.17 The mini-CEX is the mini-clinical evaluation exercise; OSCE refers to objective structured clinical evaluation; WPBA, workplace-based assessment.
OSCEs in a circuit of several stations with simulations appropriate for demonstrating specific clinical skills can be used to assess competence. The stations have manikins on which invasive techniques (e.g., inserting a nasogastric or genitourinary tube) can be performed or patient–actors are present. This approach is becoming more widely used for skills assessment in medical faculties in Spain and many other countries: the method is powerful and scores correlate with undergraduates’ average grades on theory examinations, indicating that there is a relation between knowledge acquisition and the development of clinical skills.13 To move beyond OSCEs, some faculties have added intensive instruction in performing physical examinations and they report improvement in outcomes.14 OSCEs have also been used to assess surgical skills,15 and this method has been seen to be a good way to standardize student–patient interaction; moreover, this assessment facilitates discrimination between different levels of achievement.16
Mini-CEXThe mini-CEX makes it possible to assess the fourth level on Miller's pyramid of learning (“does”). Direct structured observation is guided by a checklist, and feedback is given immediately.17 The mini-CEX is usually used to assess skill in taking patient histories and performing clinical examinations, although it can also be adapted to assess clinical judgment and communication skills. Evaluation involves interaction with real patients who have a variety of conditions of differing levels of complexity. Feedback sessions should be interactive and facilitate the student's self-assessment, which in turn furthers reflective capability. The observer tries to reinforce positive aspects observed during the clinical encounter and proposes targets for improvement. This approach is typically used in medical clerkships but has also been applied in surgical settings.18 The number and wide-ranging nature of comments made during feedback sessions make the mini-CEX a particularly rich assessment tool. Using the mini-CEX in combination with a test of knowledge acquisition and another test with standardized patients has been found to cover the range of dimensions in clinical skills.19
PortfoliosPortfolios allow for holistic assessment, given that various evaluation approaches can be incorporated in order to explore all types of competence. The content of a portfolio reflects the skills the student must acquire in each clerkship as well as the tasks to be completed to demonstrate that competence has been achieved. Specifically, the portfolio is composed of learning sheets that reflect the student's training itinerary. The medical faculty in Lleida has adopted this method for evaluating clerkships and certifying the acquisition of competencies.
Clinical Clerkships at the Faculty of Medicine, Universtat de Lleida: The Clinical Practice CoursesAs we have explained, students’ acquisition of clinical skills can be verified with a variety of approaches. The faculty of medicine in Lleida has designed a portfolio to contain a learning sheet for each clerkship the student takes during a training itinerary. Each sheet lists the targeted competencies, which are understood to be the combination of knowledge, skills, and attitudes that provide a professional with the ability to act in the best way possible when faced with a medical event (e.g., detect and treat hypertension or respond to acute chest pain). Also listed are learning objectives, which should be easily evaluable. Examples are to correctly measure blood pressure, to recognize electrocardiographic signs of acute myocardial infarction, or to differentiate one pigmented tumor from another. Finally, the sheet specifies tasks to be completed during the clerkship and how they will be assessed. Evaluation provides the basis for the supervisor's report, which counts for 40% of the grade in the course on patient care. The OSCE circuit of stations at the end of the course provides the remaining 60% of the grade.
All student clerkships in hospitals or primary care clinics have been bundled into courses (Clinical Practice I through IV). In each academic year the clinical practice course carries a total of 9 ECTS credits (standardized units in the European Credit Transfer and Accumulation System). From the second through the fifth year of studies students have 1-month clerkships (6 ECTS credits) in major departments to which are assigned the largest number of clinical competencies and which have the largest numbers of supervisors (e.g., internal medicine, primary care, general surgery, and cardiology). The additional 3 ECTS credits are earned in 2-week clerkships in areas with lower caseloads and fewer clinical supervisors (e.g., vascular surgery, rheumatology, endocrinology, and dermatology). Sixth-year clerkships require periods in internal medicine, primary care, general surgery, pediatrics, and obstetrics. During the 3 remaining months the students choose 2 specialties for month-long clerkships and 1 clerkship in a surgical specialty not chosen in previous years. Clinical clerkships not only help the students to integrate knowledge but also to acquire communication and interpersonal skills for working with patients (clinical interview, physical examination) and colleagues; they also learn to write up patient histories. Clinical judgment also improves, since they must explain alternative diagnoses and list laboratory tests and treatments used in each clerkship. Technical skills with instruments used in each specialty are also covered.
Dermatology is an optional clerkship. Students can choose between taking a 2-week session during their fifth year or doing a full 1-month optional clerkship. There are 5 dermatologists in the department, so around 90 students can be taught in their fifth year (45 in supervised clerkships). As in clerkships in other specialties, each student receives a syllabus (Appendix 2, Online Supplementary Material in Spanish) for the portfolio. The syllabus specifies the learning objectives, tasks, and assessment approach used.
At the end of the year each student completes an OSCE circuit with stations corresponding to the clerkships done that year. As mentioned above, this assessment counts for 60% of the final grade in the clinical practice course. One of the OSCE stations for fifth-year students displays clinical images and poses questions about them.
Assessing Students in the Dermatology ClerkshipThe preferred assessment approach for clerkships, as mentioned above, combines methods for evaluating knowledge with others that involve direct observation of clinical skills. Students must receive formative assessment regularly so that they can progress. Assessment should “balance validity (testing what is important) and reliability (providing inferences about the student's competence).”20 Some assessment tools are the same ones we use to evaluate residents in training, although a lower level of accomplishment is obviously required of undergraduates.21,22 The dermatology portfolio contains 5 critical incident reports for evaluation. An OSCE/WPBA observation tool is used to evaluate the student's oral communication with the patient during a clinical interview and in a presentation during a departmental session. It is also used to assess technical skills, such as the application of cryotherapy and electrocoagulation. The student's attitude and desire to learn, critical thinking, attendance, and punctuality are also evaluated by consensus.
Some authors believe that learning objectives in dermatology should consist of being able to accurately describe skin lesions and record the findings of physical examination.23 According to a survey of university instructors of dermatology in 19 Spanish teaching hospitals (unpublished data presented to a meeting of the education interest group at the national conference of the Spanish Society of Dermatology and Venereology [AEDV], Barcelona, 2008), nearly all Spanish curricula specify the teaching of knowledge about skin cancer, acne, and psoriasis as well as basic clinical skills such as history taking and examination of the skin, even though student contact with our specialty is not great. These objectives are also specified in other countries.24 We believe that students should also learn to manage dermatoses (diagnosing, differentiating, and treating them) and common skin tumors. It is our experience that it is easier to acquire these skills with a case-based approach, which includes case presentation and discussion in seminars. For facilitating acquisition, this approach seems to us to be superior to lectures. However, to integrate knowledge and skills, students need a dermatology clerkship in which they come into contact with patients and their skin diseases. A 1-month clerkship is best but is difficult to provide in many Spanish medical faculties and affiliated hospitals. Some skills, however, can be acquired in a 2-week clinical practice module. One study of whether an optional sixth-year 2-week clerkship was sufficient gave students a pretest (using slides), an immediate posttest, and a second posttest several months later.25 The mean scores on the pre- and posttests were 39.73% and 72.46%, respectively, and the mean scores on the follow-up posttest were 80.22% for students who had done the optional clerkship and 46% for those who had not.
Another learning objective that is inherent to dermatology is knowledge of quality-of-life issues for patients with chronic skin diseases. The students must become aware of the psychological and social impact of psoriasis and display sensitivity when examining the skin, for example. To this end, an effort should be made to involve patients with chronic conditions when teaching dermatology.26
Assessing KnowledgeThe dermatology content taught at the Universitat de Lleida is distributed between 2 courses. Following the practice of many other medical faculties in Spain and abroad,27 we have a 12-ECTS course encompassing skin diseases, autoimmune systems, and the musculoskeletal system; the portion on dermatology accounts for 3.5 ECTS credits, corresponding to 87.5hours. Forty percent of that total (35hours) is devoted to direct instruction (5 lectures, 15 clinical presentations,28 and 15 problem-based seminars featuring up-to-date clinical cases. The remaining 52.5hours are devoted to study, when the student works on case problem-solving and prepares for examinations. Competencies and knowledge can both be acquired through this combination of classes and study, while the problem-solving exercises improve clinical judgment. We have developed a website (www.dermatoweb.net) to support e-learning.29 Most of the students studying medicine in Lleida use the website, which is also accessed by students at many other universities in Spain and Latin America. This online resource gives the syllabus for the clerkship, provides an atlas with over 7000 photographs, and contains some 100 clinical cases with test questions and annotated answer keys. We also have over 50 cases followed by short-answer questions for discussion in seminars the day after they are posted. The students’ solutions to problems posed in these cases are counted in the final assessment for the course. Their answers must be handwritten, as students using a word processor have been found to turn in excessively long answers to questions and to abuse the strategy of copy–paste.20 The considerable increase in the number of medical students currently enrolled in many countries, including Spain, has led to the development of alternative teaching materials, such as online resources. Such resources have been shown to facilitate the acquisition of knowledge and skills, as well as the ability to manage common skin diseases and skin cancer.31 Even diagnostic skills acquired during dermatology clerkships have been found to improve with the use of online resources.32
Knowledge, the first level on Miller's pyramid, can be assessed during clerkships. Most universities administer multiple choice tests, and students in Lleida likewise take an 80-item test of this type. We use a 50-item short-answer test to assess diagnostic skills and clinical judgment (ability to consider differential diagnoses, choose additional diagnostic tests, and propose a therapeutic regimen). The questions refer to cases presented with slides. Knowledge acquired through clerkships can also be verified by means of critical incident analysis, as that method encourages reflection.3 A real incident is described in detail and analyzed in context. We ask students to analyze a critical incident every day and comment on it the following day. Five critical incidents are chosen for evaluation at the end of the clerkship. Critical incidents that can serve as examples can be provided. One might begin, “It seemed to me that the patient had ringworm but the attending said it was eczema,” followed by a question like “How can these 2 conditions be distinguished?” Or after a young girl presents with extensive psoriasis, the student might decide to find an answer to a question like “How will psoriasis affect her quality of life?” or even “Why was the patient so angry on having to wait a bit before being called in?” Analyzing such incidents motivates the student to study because the knowledge gained has immediate relevance.
Assessing SkillsSkills students are expected to acquire during a 1-month dermatology clerkship at the Universitat de Lleida are as follows: communicating with a patient, communicating with peers through a presentation during a departmental session, applying cryotherapy and electrocoagulation, and performing a small wedge resection and suturing the wound. The wedge resection is not included in 2-week clerkships.
Communication SkillsOne of the essential competencies stipulated for dermatology clerkships would be the ability to appropriately carry out a clinical interview in dermatology. The student must become familiar with the questions the attending asks during the first week, and starting in the second week the student will complete 5 case histories for patients with skin diseases or tumors. These histories will be kept in the portfolio. We provide students with a template (Appendices 3 and 4, Online Supplementary Material in Spanish) for history taking. The templates help students learn to structure a case history properly and reduce the amount of time dedicated to writing up each case.30 One aspect of communication that can be assessed is how well the student meets the aims of providing health care education about behaviors to prevent contagion of sexually transmitted diseases and tracing sexual contacts; a comparable scenario would be educating the patient about sun protection and avoidance behaviors in relation to skin cancer.
We use an OSCE/WPBA checklist (Table 1) to assess communication skills. The points to assess include physical examination and closing the session with an explanation of the diagnosis as well as the need to order tests and treatment or not. Students are advised to take specific communication skills courses that have proven very effective, especially during the early years of medical studies or when an individual finds communication particularly difficult.33,34 Another aid to improvement is interaction with patient simulators (actors). Joint student and supervisor analysis of videotaped interviews, with feedback, provides another way to advance. A student can also be instructed to watch a standardized interview conducted by an expert in order to facilitate self-assessment.33
Quality Indicators for OSCE/WPBA Assessment of a Clinical Interviewa
| The interview | |
| 1. Student introduces him or herself. | 1–2–3–4–5 |
| 2. Expresses empathy, facilitates the patient's explanations. | 1–2–3–4–5 |
| 3. Conducts an exhaustive structured interview. | 1–2–3–4–5 |
| 4. Asks appropriate questions to gather information. Listens attentively. | 1–2–3–4–5 |
| 5. Gives appropriate response to the patient's questions. Notices body language. | 1–2–3–4–5 |
| Directed physical examination | |
| 6. Examines skin, mucosa, and adnexa. | 1–2–3–4–5 |
| 7. Conducts a general physical examination (in the presence of systemic diseases and tumors with metastatic ability). | 1–2–3–4–5 |
| Closing the interview | |
| 8. Gives a clear explanation of the diagnosis, need for additional tests, and treatment. Educates the patient about health. | 1–2–3–4–5 |
| 9. Manages time effectively (10–20 min, depending on disease). | 1–2–3–4–5 |
| Score for overall quality | 1–2–3–4–5 |
Abbreviations: OSCE, objective structured clinical examination; WPBA, workplace-based assessment.
Among the written communication skills to acquire, we emphasize the ability to properly write a case history in dermatology.
Giving a presentation before an audience is another communication skill included in the syllabus. Students must search the literature on a topic, review it, and finally present the findings at a departmental session, for evaluation using an OSCE/WPBA checklist of criteria covering verbal and nonverbal aspects of the talk and the quality of slides (Table 2).
Quality Indicators for OSCE/WPBA Assessment of an Oral Presentation in a Departmental Session.
| Type of session (underline one): literature review, case report, original research report |
| Name |
| The student |
| Knows the material. |
| Speaks clearly, audibly. |
| Modulates the voice, appropriate intonation. |
| Controls nervousness. |
| Makes eye contact. |
| Presents the material that was announced for the session. |
| Displays a natural, professional demeanor. |
| The slides |
| Readability (number of words/slide; fonts and sizes are easy to read). |
| Overall quality (colors of lettering and background, arrangement of information). |
| Number appropriate to time allotted. |
| Emphasis is on important points |
| Makes key points clear. |
| Presents evidence. |
Abbreviations: OSCE, objective structured clinical interview; WPBA, workplace-based assessment.
Dermatology has a large number of practical skills for students to acquire. The potassium hydroxide (KOH) test is one of the most commonly ordered laboratory procedures in some countries, to the point where computer simulations have been developed to serve as teaching aids.35 The ability to discern hyphae is an optional competency in our program, as we do not always have patients with a positive KOH test at our disposal during a clerkship.
The number of procedures that can be practiced will depend on whether the clerkship lasts 2 or 4 weeks. For the 2-week period, we target learning how to perform cryotherapy or electrocoagulation, whose assessment criteria are described in Tables 3 and 4. For the 1-month period, we also ask students to perform small wedge resections and suture them at the end of the clerkship, at which point they will have observed several; the students always perform under direct supervision. They must become familiar with the OSATS checklist (Table 5) before they perform.
Quality Indicators for Assessing a Cryotherapy Procedure.
| 1. Student introduces him or herself. |
| 2. Expresses empathy. |
| 3. Explains the usefulness of the procedure. |
| 4. Explains the adverse effects (pain, inflammation). |
| 5. Sprays the lesion from a distance of 1–2cm, holding the nozzle perpendicular to the skin and pressing the trigger intermittently to avoid accidental spills. |
| 6. Sprays lightly until the whole lesion is frozen and there is a target-shaped frozen ring 1–2mm around it; or for larger lesions sprays in a spiral pattern or uses the paint-brush method, repeating the spray cycle 1–3 times, as appropriate for the type of lesion |
Quality Indicators for Assessing a Curettage Procedure With or Without Electrocoagulation.
| 1. Student introduces him or herself. |
| 2. Expresses empathy. |
| 3. Asks if the patient is allergic to the anesthetic. Explains the usefulness of the procedure. Calms the patient. |
| 4. Prepares the necessary material (alcohol or povidone–iodine, sterile gauze, gloves, insulin syringe and anesthetic, electric scalpel, and a recipient with formalin for collecting samples) |
| 5. Washes hands. |
| 6. Puts nonsterile latex gloves on. |
| 7. Cleans the skin with sterile gauze soaked in povidone–iodine. |
| 8. Inserts the needle of the syringe to the intradermal level for slow infiltration of the anesthetic. Infiltrates in a fan-shaped pattern for lesions > 1cm. Injects enough of the anesthetic to raise an intradermal wheal. |
| 9. Electrocoagulates the base of pedunculated lesions. Shaves domed lesions and then electrocoagulates to completely remove the lesion. |
| 10. Cleans the area with povidone–iodine and covers the wound with a sterile dressing. Explains how to care for the wound at home. |
| 11. Washes hands again. |
Quality Indicators for Performance of a Wedge Resection Using an OSATS Checklist.a
| Student puts on a surgical cap and mask. |
| Scrubs in (surgical hand scrub). |
| Prepares the surgical field. |
| Administers the anesthetic. |
| Selects suture material and technique. |
| Performs the wedge resection. |
| Sutures the dermal and superficial layer of the skin. |
| Dresses the wound. |
| Overall skill. |
| Duration of the procedure. |
Abbreviation: OSATS, objective structured assessment of technical skills.
Attitude is the most difficult aspect to assess. The student should demonstrate a desire to learn, express opinions and points of view, and demonstrate critical thinking. An attitude of consideration and respect for patients and colleagues must also be evident. The student is awarded a grade for attitude on the basis of consensus between the supervisor and the other physicians in the department. Attendance at over 80% of the clerkship sessions and punctuality are required.
ConclusionsInclusion of the concept of professional competency in the new syllabi for all Spanish medical faculties obliges us to reflect on the material taught in undergraduate clerkships and how to certify the acquisition of competencies. The medical faculty at the Universitat de Lleida has chosen a portfolio-based assessment method, in which materials from undergraduate clerkships are collected. Individual supervision is a fundamental aspect of this method.
The competencies the student must consolidate during a full clerkship in the dermatology department involve managing, at a basic level, common skin diseases and tumors; carrying out a clinical interview and examining the patient properly according to standard criteria, and describing lesions precisely; presenting information to an audience during a departmental session according to standards; and applying cryotherapy and electrocoagulation as well as performing a wedge resection. We also assess whether the student has a desire to learn and treats patients and colleagues with respect. Various assessment tools are included in a portfolio to facilitate holistic evaluation of the student's work: written analyses of critical incidents for assessing knowledge and the results of OSCE circuit testing of skills. The grade for attitude is the result of agreement between the supervisor and the other physicians in the department. The supervisor's report accounts for 40% of the final clinical practice course grade (10% each for knowledge, communication skills, technical skills, and attitude). The remaining 60% comes from the OSCE circuits that are set up at the end of an academic year. That circuit includes a station with clinical images.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed the protocols of their hospitals concerning the publication of patient data and that all the patients included in this study were appropriately informed and gave their written informed consent.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Casanova JM, Sanmartín V, Martí RM, Morales JL, Soler J, Purroy F, et al. Evaluación de las prácticas clínicas de Dermatología en el grado de Medicina. Actas Dermosifiliogr. 2014;105:459–468.
First presented in workshop form at the national conference of the Spanish Academy of Dermatology and Venerology, Oviedo, Spain, June 8, 2012.