We report the case of a 56-year-old man with a history of chronic obstructive pulmonary disease and hypertension who was being treated with eprosartan/hydrochlorothiazide and atorvastatin/amlodipine. He presented with an eczematous, pruritic skin condition that had developed 2 months previously.
Physical examination revealed coalescing erythematous plaques on the upper limbs, face, and the upper third of the trunk, affecting approximately 25% of the body surface. There was no palmoplantar or mucosal involvement (Fig. 1). A skin biopsy of the affected area showed a superficial perivascular dermatitis with eosinophils and intraepidermal necrotic keratinocytes, suggesting drug-induced skin disease. Blood tests revealed leukocytosis (15 330×109/L), with a predominance of neutrophils (82.2%), and increases in the erythrocyte sedimentation rate and in the levels of C-reactive protein and immunoglobulin E (>5000 IU/mL).
After diagnosis of drug-induced skin disease antihypertensive treatment was discontinued and a tapering dosage of prednisone was prescribed, starting at 1mg/kg/d. After 40 days of treatment the dose of corticosteroids was reduced to 10mg/d due to the development of cushingoid habitus. Given the progression of the skin lesions to erythroderma, affecting almost 90% of the body surface, the patient was treated with acitretin (25mg/d), which stabilized the symptoms and reduced the intensity of the erythroderma and pruritus. The patient's baseline hypertension was controlled by dietary measures after a relapse induced by temporary treatment with enalapril.
Laboratory workups and monthly imaging studies revealed no differences as compared with the initial findings. Eight months later eosinophilia was detected (20.8%; 2310×109/L). A new skin biopsy revealed no additional findings and bone marrow aspiration was normal.
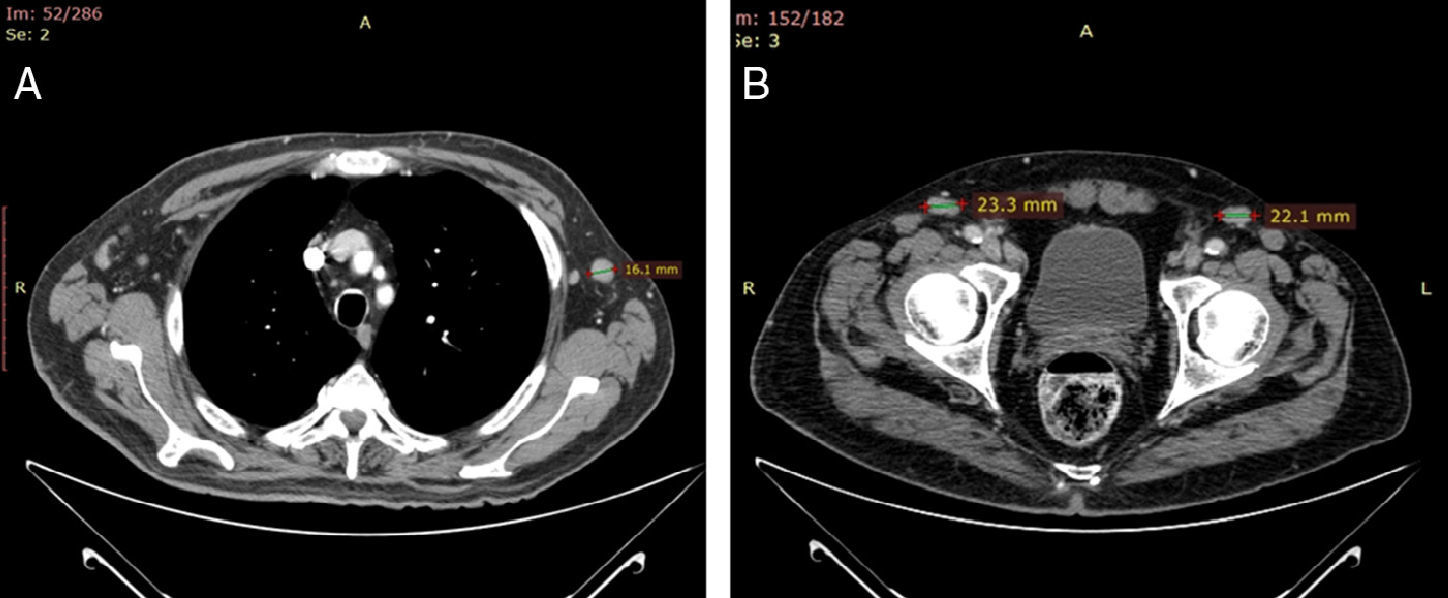
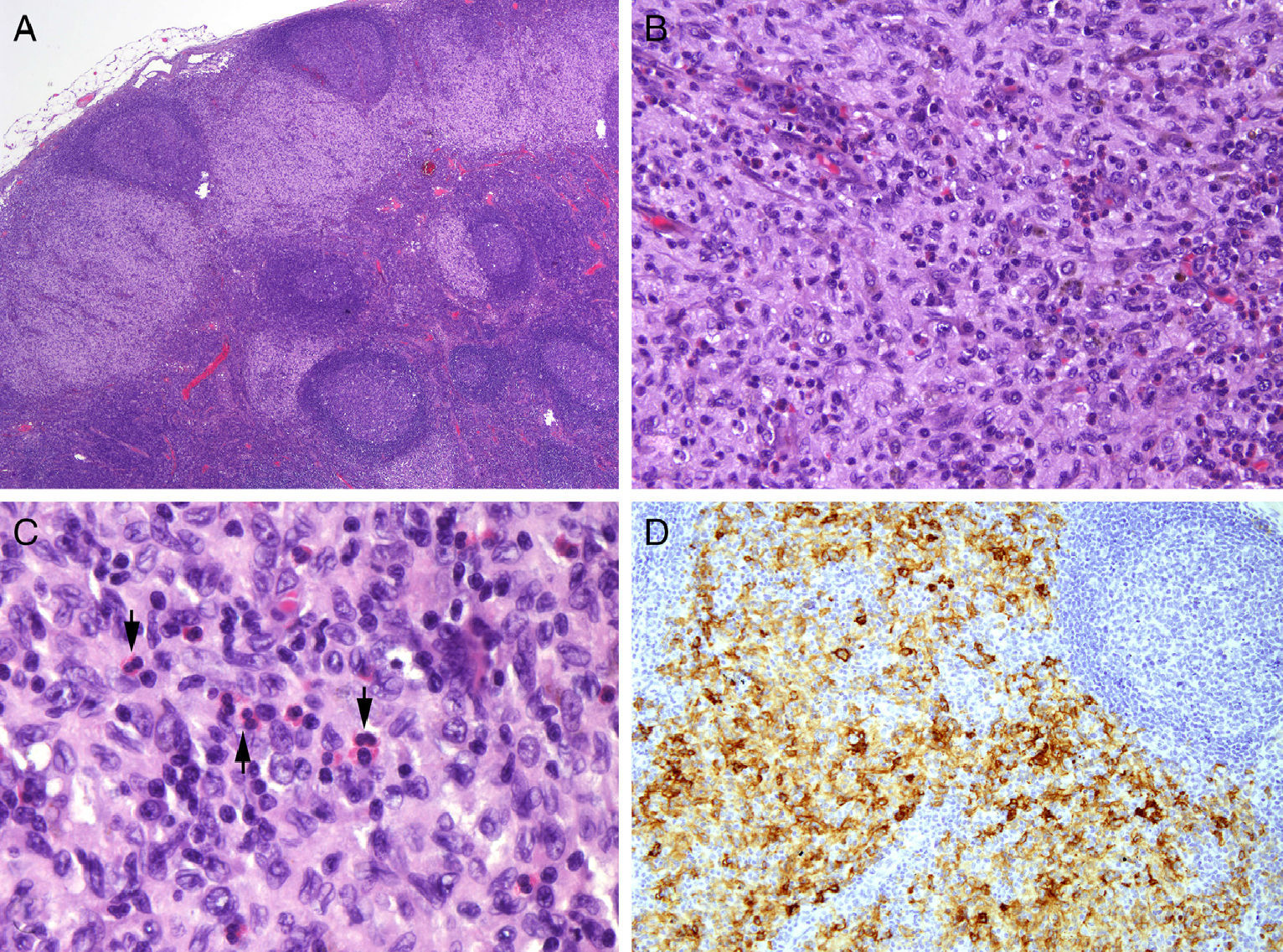
Weeks later the patient noticed an enlarged right inguinal lymph node of 2cm in diameter. A computed tomography scan of the chest and abdomen revealed considerable enlargement of the mediastinal lymph nodes (Fig. 2A) and bilateral axillary and inguinal lymph nodes of over 1cm in diameter (Fig. 2B). No hepatosplenomegaly, mesenteric lymphadenopathy, or bone alterations were observed. Histological examination of the inguinal node revealed that the paracortex contained cellular aggregates consisting of large cells with grooved nuclei containing compact chromatin, together with a large, eosinophilic cytoplasm. Microabscesses and occasional histiocytes and plasma cells were also observed. The cells were positive for S-100/CD1a and negative for myeloperoxidase and CD117, and had a low proliferative index. A histological diagnosis of Langerhans cell histiocytosis (LCH) involving the sinus was established (Fig. 3 A-D). Based on this diagnosis, acitretin treatment was discontinued and the patient began treatment with tapering dosages of vinblastine (intravenous bolus, starting at 6mg/m2) and oral prednisone (starting at 40mg/m2/d) for 6 and 4 weeks, respectively. This resulted in an improvement in the patient's baseline condition. The patient remains asymptomatic after 3 months of follow-up.
A, Lymph nodes affected by Langerhans cell histiocytosis (hematoxylin-eosin, original magnification ×2). B, Subcapsular sinus occupied and expanded by a predominantly mononuclear cell population containing some eosinophils (hematoxylin-eosin, original magnification ×20). C and D, Higher magnification images showing the eosinophils (arrowheads in C; hematoxylin-eosin, original magnification ×40) and the grooves or folds in the elongated nuclei of the CD1a+ Langerhans cells (D; CD1a, original magnification ×10).
Erythroderma is defined as inflammation that affects at least 90% of the body surface. Its etiologic diagnosis is difficult.1 The dermatologist must be alert to the possibility of an underlying neoplasm in cases of insidious onset, treatment resistance, or weight loss, and in cases with no prior history of skin disease.2 Histology is nonspecific, and despite the presence of signs specific to the primary disease, etiologic diagnosis is often not achieved.3
LCH is a relatively uncommon entity characterized by oligoclonal proliferation of Langerhans cells. Its incidence is unknown4 and it is difficult to diagnose. Cutaneous presentations of LCH resembling pyoderma gangrenosum, annular granuloma, amebiasis, eruptive xanthomas, and flat warts, among other conditions, have been described.5,6 LCH can affect one or more organs; the number of affected organs has implications for prognosis and treatment. This condition has been reported in association with solid tumors, lymphomas, and leukemias, and a common origin of LCH and hematological malignancies has been widely debated.7,8
Several therapeutic strategies are used in the management of LCH in adult patients, depending on the number of organs involved and the clinical course. In our case, even though only lymphatic involvement was initially observed, we opted for aggressive therapy, which significantly reduces morbidity and mortality according to the Evaluation and Treatment Guidelines of the Histiocyte Society.9
Erythroderma as an initial presentation of LCH, as occurred in the present case, has been described in only one series to date.10 The main difficulty in the present case was the length of time between the onset of erythroderma and lymphadenopathy; we established a definitive histological diagnosis of the latter through histological analyses, as all findings hitherto were nonspecific. We wish to stress the importance of repeated complementary testing and close follow-up with retesting in patients with erythrodermas with an atypical clinical course and poor therapeutic response.
Please cite this article as: Ruiz-Villaverde R, Galán-Gutierrez M, Ramos-Pleguezuelos F, Martinez de Victoria J. Eritrodermia como forma de presentación inicial de histiocitosis sinusal de células de Langerhans. Actas Dermosifiliogr. 2014;105:630–632.