Clinical characteristics of psoriasis vary between different races and climates. There are few data on Latin American and even fewer on Chilean patients with psoriasis.
ObjectivesTo assess that clinical characteristics and quality of life (QoL) of a group of Chilean patients with psoriasis.
MethodsA cross-sectional, observational and analytic study was conducted at the Dermatology Department of the Clinical Hospital of the University of Chile between July 2006 and December 2008 applying an epidemiological and QoL-related survey to psoriatic patients.
ResultsOne hundred fifty-three patients with psoriasis were included in the study. The mean (SD) age was 42.7 (14.9) years and 60.1% of the patients were male. The most frequent disease subtype was plaque psoriasis (71.9%), followed by “guttatiform” (guttate morphology without confirmed streptococcal infection) psoriasis (17.7%). In 38.6% of patients, less than 10% of body surface area (BSA) was affected. Joint involvement was reported in 28.8% of patients. Those with early onset of disease (before 30 years of age) were more likely to have a positive family history of psoriasis. Hypertension and diabetes were present in 20.3% and 11.1% of patients, respectively. The mean Dermatology Life Quality Index was 14. Greater impact of the disease on QoL was associated with male sex, young age of onset, newly diagnosed disease, facial involvement, and widespread disease.
ConclusionChilean patients with psoriasis have clinical characteristics and QoL comparable to patients in other countries. A notable difference, however, was the greater impact of psoriasis on the QoL of Chilean men compared to women.
Las características clínicas y calidad de vida (CDV) de los pacientes psoriásicos varía según la raza y el clima. Son escasos los estudios en Latinoamérica en general y en Chile en particular.
ObjetivosDeterminar aspectos clínicos y CDV de un grupo de pacientes psoriásicos chilenos.
MetodologíaSe realizó un estudio de corte, observacional y analítico, en el Departamento de Dermatología del Hospital Clínico de la Universidad de Chile entre julio de 2006 a diciembre de 2008, aplicándose una encuesta a pacientes psoriásicos sobre aspectos clínicos e impacto de la enfermedad en la CDV.
ResultadosSe incluyeron 153 pacientes. El promedio de edad fue 42,7±14,9 años (hombres/ mujeres: 60,1%/ 39,9%). El subtipo clínico más frecuente fue psoriasis en placas (71,9%) seguido de la psoriasis guttata (17,7%). El 38,6% de los pacientes tenía menos del 10% de la superficie corporal afectada y el 28,8% tenía compromiso articular. Aquellos pacientes con enfermedad de inicio temprano (antes de los 30 años) tenían más historia familiar positiva de psoriasis. El 20,3 y 11,1% tenía, concomitantemente, hipertensión y diabetes mellitus, respectivamente. El Dermatology Life Quality Index (DLQI) promedio fue de 14. Los aspectos relacionados con un mayor impacto de la psoriasis en la CDV fueron: sexo masculino, presentación a edad temprana, enfermedad de reciente diagnóstico, afectación de la cara y enfermedad extensa.
ConclusionesLas características clínicas de los pacientes chilenos con psoriasis y el impacto de la enfermedad en la CDV es comparable con lo reportado en otros países. Destacamos el mayor impacto de la enfermedad en la CDV de hombres chilenos comparado con las mujeres.
Psoriasis is almost universally present in the human population. Despite extensive research, the pathophysiology is not fully understood though the explosive development of new therapeutic options has advanced our understanding. The prevalence of the disease varies widely from 0% in American Samoa1 and South American indigenous peoples2 to 11.8% in Northern Russia.1 The mean worldwide prevalence of psoriasis is considered to be around 2%.3 Moreover, it has been reported that the prevalence of psoriasis varies with climatic conditions and is more common in colder climates than in tropical regions.1,3 Several studies have suggested Caucasians are more affected than other races.4 It is known that psoriasis has a substantial impact on quality of life (QoL). A systematic review of the literature established that patients with psoriasis suffer physical discomfort, impaired emotional functioning, a negative body self-image and limitations in daily activities, social contacts and work.5 The severity of psoriasis was also correlated with a poor QoL, whereas gender and QoL are generally found to be unrelated.
Most of the knowledge about psoriasis, its clinical features and its psychological impact has been generated in European and North American populations. There are few reports in the literature on psoriatic patients and their QoL in Latin America. In Chile, psoriasis accounts for 2.03% of dermatological consultations, with higher rates (around 2.6%) in the cooler southern area and 1.8% in the warmer north; in addition, a difference has been observed between urban and rural areas (2.3% versus 1.9%; Sánchez Millán et al, personal communication). To our knowledge, this is the first report of Chilean patients with psoriasis including assessment of QoL.
The purpose of this study was to determine epidemiological features and the impact on QoL of psoriasis in patients seen in a Chilean hospital.
Patients and MethodsAn observational, analytic, cross-sectional study evaluating clinical, epidemiological and QoL-related features of psoriasis in the Chilean population was carried out from July 2006 to December 2008 at the Dermatology Department of the University of Chile Clinical Hospital in Santiago. A multiple-choice questionnaire was designed, including information on sex, current age, clinical type of psoriasis, body surface area (BSA) affected by psoriasis, anatomical distribution of lesions, treatment regimens (not presented here), family history, age at onset of psoriasis, comorbidities, joint involvement (with or without rheumatology evaluation), and triggering factors (not presented here). All psoriatic patients seen during the study period were informed of the survey and consent was obtained prior to participation. Dermatology residents conducted the survey. Patients then completed the Spanish version of the Dermatology Life Quality Index (DLQI), which includes 10 questions and is designed for use in adults. It is self-explanatory and can be simply handed to the patient who is asked to fill it in without the need for detailed explanation. The scoring of each question is as follows: very much, 3; a lot, 2; a little, 1; not at all, 0; not relevant, 0; question unanswered, 0. The DLQI is calculated by summing the score on each question, resulting in a maximum of 30 and a minimum of 0. The higher the score, the greater the impairment of QoL. The DLQI can also be expressed as a percentage of the maximum possible score of 30. DLQI scores are interpreted as follows: 0-1, no effect at all on QoL; 2-5, small impact on patient's QoL; 6-10, moderate impact on patient's QoL; 11-20, very large impact on patient's QoL; 21-30, extremely large impact on patient's QoL. For patients younger than 18 years, we applied the Children's DLQI (CDLQI).
For the analysis of early versus late onset psoriasis, we separated the sample into 2 groups. Early onset was defined as psoriasis that appeared at 0 to 30 years and late onset as that appearing in patients older than 30 years.6 We also compared comorbidity rates for hypertension and diabetes mellitus in our sample with the general Chilean population based on data from the Chilean Ministry of Health.7
Statistical analysisContinuous data were described as means (SD). Categorical variables were described as frequencies and percentages. Missing values were not included in calculations. Parametric statistic analysis (t test or analysis of variance) was used when parametric assumptions were met. χ2 and Kruskal-Wallis test were used to analyze categorical and non-normally distributed variables. Statistical analyses were conducted using SPSS 17.0 and a significance level of P<.05 was applied.
ResultsBetween July 2006 to December 2008, 153 outpatients with a diagnosis of psoriasis attending the Dermatology Department of the Clinical Hospital University of Chile were included in the study. Psoriasis accounted for 4.65% of the dermatology consultations seen in our hospital during the study period. Taking into account the total number of dermatological patients seen in our hospital, the sample of 153 patients represents 66.5% of all patients with psoriasis seen during this period (230 patients). Requests for patients to participate in the study were random, and 93% of patients agreed. Almost every patient was white Latino, with less than 5% Caucasians and less than 5% indigenous Chilean. Most participants came from the northern urban area of Santiago de Chile. Men accounted for 60.1% of the sample and women 39.9%. The mean (SD) age of the patients was 42.7 (14.9) years (range, 9–79 years). There were no significant differences in the mean age between sexes. The distribution in age ranges was as follows:<10 years, 1.3%; 10-29 years, 16.3%; 30-49 years, 50.3%; 50-69 years, 28.1%; and ≥ 70 years, 3.9%. Plaque psoriasis was the predominant morphological type (71.9%), followed by “guttatiform” (guttate morphology without confirmed streptococcal infection) psoriasis (17.7%) and palmoplantar or inverse types (2.6% each). Uncommon types were erythrodermic psoriasis (2.0%), generalized pustular psoriasis (0.6%), and nail or scalp psoriasis (2.6%).
The anatomical distribution of skin lesions was as follows: 83.0% of patients had psoriasis on the lower limbs (including the feet), 73.2% had involvement of the upper limbs, 75.16% had trunk involvement, 62.09% had scalp plaques, 31.37% had lesions on the hands, 16.34% had lesions on the face, and 14.38% had lesions on the genitalia. Nearly one third (38.6% of patients) had less than 10% of BSA affected, while 29.4% had 10% to 29%, 16.3% had 30% to 49%, 7.8% had 50% to 69%, and 5.9% had 70% to 90% BSA involved; 2.0% were classified as erythrodermic. Men had a higher BSA affected than women (P<.03).
The time since appearance of the disease at the time of the study was less than 1 year in 12.4% of patients, 1 to 4 years in 8.5%, 5 to 9 years in 21.6%, 10 to 20 years in 29.4%, and more than 20 years in 28.1% of patients.
When we asked about family history of psoriasis, 47.1% of patients had a first- or second-degree relative with the disease (positive family history of psoriasis).
In relation to joint involvement, 28.8% of patients reported some joint disease, although only 10 patients had a rheumatology evaluation that confirmed psoriatic arthritis (6.5%). Taking all patients with self-reported joint involvement into consideration, 6.8% had a single affected joint, 72.7% had less than 5 affected joints, and 20.5% had more than 5 affected joints. There were no significant differences between symmetric (14.4%) and asymmetric (13.1%) joint involvement (18 and 14 patients respectively). No patients with mutilating arthritis were observed and 2 patients (4.5% of patients with joint involvement) had spondyloarthritis. The most commonly affected joints were the knees, wrists and distal interphalangeal joint.
Among reported selected comorbidities, 20.3% of our sample had high blood pressure and 11.1% had diabetes mellitus.
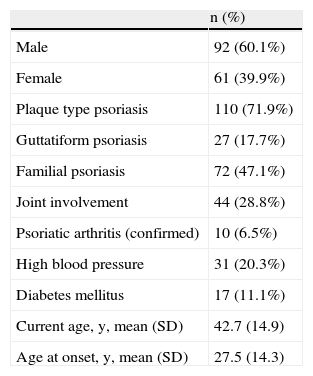
Table 1 shows a review of the most important demographic and clinical features of enrolled patients.
Demographic and Clinical Features of Enrolled Patients (N=153).
| n (%) | |
| Male | 92 (60.1%) |
| Female | 61 (39.9%) |
| Plaque type psoriasis | 110 (71.9%) |
| Guttatiform psoriasis | 27 (17.7%) |
| Familial psoriasis | 72 (47.1%) |
| Joint involvement | 44 (28.8%) |
| Psoriatic arthritis (confirmed) | 10 (6.5%) |
| High blood pressure | 31 (20.3%) |
| Diabetes mellitus | 17 (11.1%) |
| Current age, y, mean (SD) | 42.7 (14.9) |
| Age at onset, y, mean (SD) | 27.5 (14.3) |
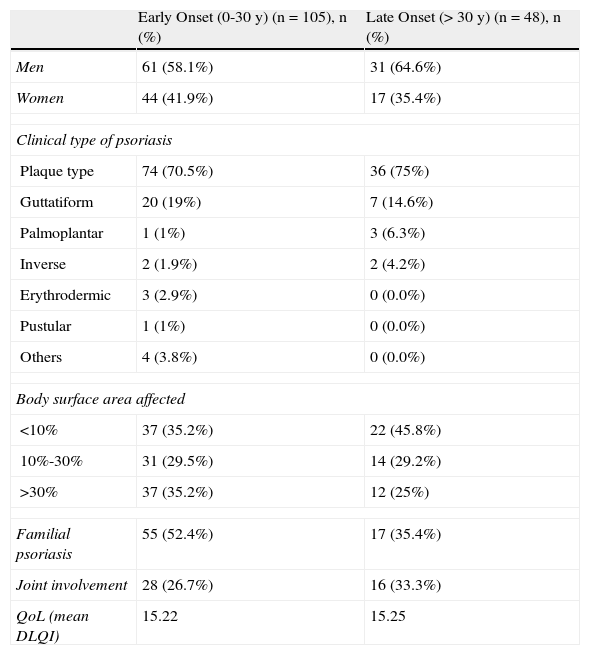
The mean age at onset was 27.5 (14.3) years and there was no significant difference between men and women (29.2 and 24.8 years, respectively). In order to find differences between patients with early and late onset psoriasis, patients were classified into 2 different groups (onset up to or after the age of 30).6,8 The early-onset group included 105 patients and the late-onset group 48 patients. There was no significant difference in onset according to sex in the total sample; however, in the late-onset group there was a slight but significantly greater number of men (31 men versus 17 women, P=.043).
The early-onset group had more guttatiform psoriasis than the late-onset group but the difference was not significant (19% versus 14.6%, P=.502). All patients with pustular or erythrodermic psoriasis belonged to the early-onset psoriasis group. The late-onset group had proportionally more inverse and palmoplantar psoriasis than the early-onset one. None of these differences were statistically significant. The early-onset group had slightly more BSA affected by psoriasis, reported more positive family history of psoriasis, and had less joint involvement than the late-onset group, but these findings were not statistically significant (Table 2).
Clinical Features of Psoriasis in Patients With Early-Onset and Late-Onset Disease (N=153).
| Early Onset (0-30 y) (n=105), n (%) | Late Onset (> 30 y) (n=48), n (%) | |
| Men | 61 (58.1%) | 31 (64.6%) |
| Women | 44 (41.9%) | 17 (35.4%) |
| Clinical type of psoriasis | ||
| Plaque type | 74 (70.5%) | 36 (75%) |
| Guttatiform | 20 (19%) | 7 (14.6%) |
| Palmoplantar | 1 (1%) | 3 (6.3%) |
| Inverse | 2 (1.9%) | 2 (4.2%) |
| Erythrodermic | 3 (2.9%) | 0 (0.0%) |
| Pustular | 1 (1%) | 0 (0.0%) |
| Others | 4 (3.8%) | 0 (0.0%) |
| Body surface area affected | ||
| <10% | 37 (35.2%) | 22 (45.8%) |
| 10%-30% | 31 (29.5%) | 14 (29.2%) |
| >30% | 37 (35.2%) | 12 (25%) |
| Familial psoriasis | 55 (52.4%) | 17 (35.4%) |
| Joint involvement | 28 (26.7%) | 16 (33.3%) |
| QoL (mean DLQI) | 15.22 | 15.25 |
Abbreviations: DLQI, Dermatology Life Quality Index; QoL, quality of life.
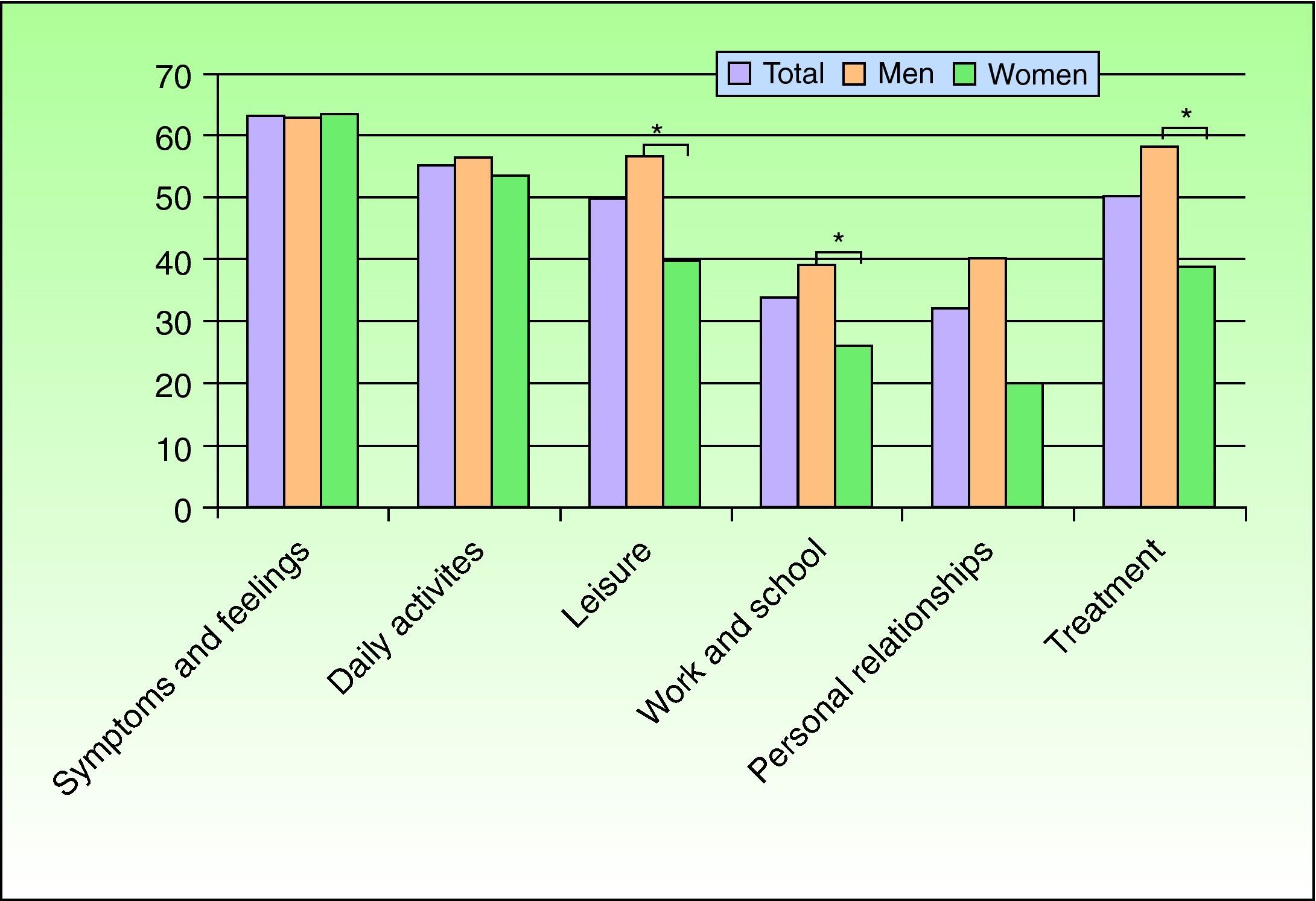
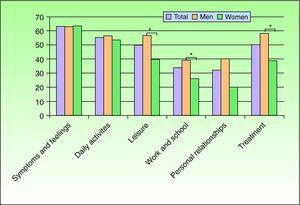
In order to evaluate the impact on QoL, the Spanish version of DLQI was applied. The mean DLQI was 14 (“very large impact”). The impact on QoL was significantly higher for men (mean DLQI, 15) than for women (mean DLQI, 13) (P=.027) even though both sexes lie within the range of “very large impact”. The most affected QoL domains were symptoms and feelings, daily activities, and treatment. There were statistically significant differences between sexes in the leisure, personal relationships, and treatment domains. Men were more affected in all these domains than women (Fig. 1).
DLQI in the groups of early and late onset was 15.22 and 15.25, respectively (P=.52) (Table 3).
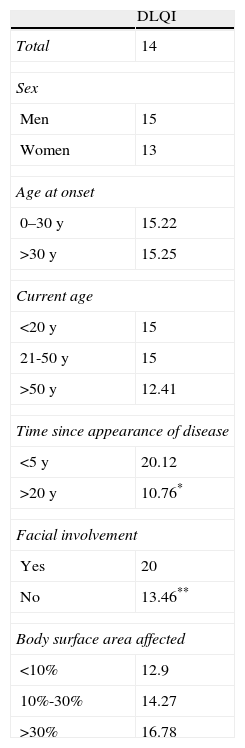
Comparison of Dermatology Life Quality Index (DLQI) According to Sex, Age at Onset, Current Age, Time Since Appearance of Disease, Facial Involvement, and Extent of Disease.
| DLQI | |
| Total | 14 |
| Sex | |
| Men | 15 |
| Women | 13 |
| Age at onset | |
| 0–30 y | 15.22 |
| >30 y | 15.25 |
| Current age | |
| <20 y | 15 |
| 21-50 y | 15 |
| >50 y | 12.41 |
| Time since appearance of disease | |
| <5 y | 20.12 |
| >20 y | 10.76* |
| Facial involvement | |
| Yes | 20 |
| No | 13.46** |
| Body surface area affected | |
| <10% | 12.9 |
| 10%-30% | 14.27 |
| >30% | 16.78 |
*P=.002, **P<.001.
DLQI in patients younger than 20 years and between 21 and 50 years was 15 and for those patients older than 50 years DLQI was 12.41 (P=1.72) (Table 3).
Patients with recent disease (onset within the last 5 years) had a DLQI of 20.12, which is significantly higher than the DLQI 10.76 observed in patients with long-standing disease (more than 20 years) (P=.00007) (Table 3).
Psoriasis affecting the face was associated with a higher mean DLQI (20 in patients with face involvement versus 13.46 in those without, P=.002). Involvement of the genitalia, hands, and joints were also associated with a higher DLQI but these differences were not statistically significant (Table 3).
In relation to the extension of the disease, patients having less than 10% of BSA affected had a DLQI of 12.9, those with 10% to 30% BSA affected had a DLQI of 14.27, and patients with more than 30% BSA affected had a DLQI of 16.78, but these differences were not statistically significant (P=.1) (Table 3).
DiscussionThis study includes outpatients with psoriasis seen in our department over a period of 29 months without exclusions related to age, extent of psoriasis, or whether the patient was seen for a first visit or follow-up. Each patient completed a single questionnaire and follow-up was not included. The distribution of psoriasis subtypes in our sample was similar to published data. A recent study from the Iberian region reported the following distribution of psoriasis subtypes: vulgaris (79.8%), guttate (6.7%), palmoplantar (4.0%), erythrodermic (4.3%), pustular (1.8%) and other types (3.3%).9 All of the proportions were very similar to our data, except for guttate psoriasis. Another study from Japan, which enrolled over 28 000 patients with psoriasis, reported 86.0% plaque psoriasis, 2.8% guttate psoriasis, 0.8% psoriatic erythroderma, 0.9% generalized pustular psoriasis, and 0.5% localized pustular psoriasis.10 The most frequent manifestation of psoriasis in all these studies was chronic plaque-type psoriasis,9,10 as in our study. In our study there was a higher rate of guttatiform psoriasis (17.7%). This may be because we included psoriasis with guttate morphology without confirmed streptococcal infection (for this reason, we used the term guttatiform rather than guttate psoriasis), or because patients aged up to 30 years (where guttate psoriasis is more prevalent) represented 16.3% of our sample, or because a real difference in psoriatic types truly exists. Mallbris et al11 reported in a Swedish study that enrolled 400 adults with a first psoriatic episode, that 18% of cases corresponded to guttate psoriasis. Comparing early- and late-onset psoriatic groups, guttatiform psoriasis was more frequent in the early onset group, whereas inverse and palmoplantar psoriasis were more frequent in the late-onset group. These differences were not significant but are in agreement with the results of the previously mentioned Spanish study that separated patients with psoriasis into early and late onset of disease.6 We also found that all the cases of erythrodermic and pustular psoriasis belonged to the early-onset group, but the number of patients with this type of disease was very small.
In relation to anatomical distribution, we found that the most frequently involved areas (from greater to lesser) were lower limbs, upper limbs, trunk and scalp. Kawada et al10 reported similar results from a large study. In our study, men had a larger affected BSA than women, and more than 60% of our patients had more than 10% of BSA involved. Similar results were reported in the Iberian population.6,9
The mean age at onset of psoriasis in our sample was 27.5 years (range, 4–68 years), without significant differences between sexes in the sample as a whole; however, in the late-onset group there was a slight but significantly larger proportion of men. In the international literature, a range between 23 and 37 years has been reported,12 and in Spanish patients it has been estimated between 28 and 29 years,6,9 very similar to other European reports, with mean ages at onset of 27 in women and 29 in men.13 In contrast, Japanese patients had an older mean age of onset, 39 years of age.10 Women tend to develop psoriasis earlier than men in Western countries6,8,13 and in Japan.10
The rates of positive family history of psoriasis reported in the literature vary widely from 2% to nearly 91%.13,14 In our study, 47.1% of patients reported that a first- or second-degree relative had psoriasis, which is comparable to reports from Spain (40.7%),6 the Iberian Peninsula (49.6%),9 and Sweden (52%),11 but much greater than in Japan (4.4%).10 Our results suggest that a positive family history of psoriasis is inversely related to the age at onset of the disease, which has been noted in several other studies.6,15 The mentioned studies also demonstrated that the disease has an irregular course with tendency to be severe in patients with early-onset psoriasis, especially those with a positive family history.6,8
High blood pressure and diabetes mellitus were present as comorbidities in 20.3% and 11.1% of our sample, respectively. Again, these data are very similar to those described by García-Díez et al9 for Spanish and Portuguese patients (20.2% for high blood pressure and 8.3% for diabetes). Comparison of these rates with published data on the healthy Chilean population, where hypertension has a prevalence of 10.3% and diabetes mellitus of 3.2%,7 revealed statistically significant differences between age- and sex-matched individuals according to the Z test. Current studies have given some evidence of an association between psoriasis and diabetes mellitus, hypertension, atherosclerosis, obesity, and ischemic heart disease.16 However, further studies are needed to support these observations. The link between the pathophysiology of metabolic syndrome, cardiovascular disease, and psoriasis may be explained by a chronic inflammatory state.17 In recent years, there has been growing interest in the possibility of modifying this association, especially among researchers who study biological agents that target the inflammatory cascade.17 Screening for metabolic syndrome in all psoriatic patients is highly recommended, especially in cases of severe disease.16,17
Psoriatic arthritis (PsA) has been defined as a chronic inflammatory arthropathy of the peripheral joints and axial skeleton, usually seronegative and associated with psoriasis, which is estimated to occur in 1% to 3% of the general population but in 4.7% to 42% of patients with psoriasis.9,18,19 The exact prevalence of PsA is unknown and its estimation has been difficult for a number of reasons, including the lack of an accepted classification and clear diagnostic criteria.6,20 Recent studies have suggested that PsA occurs in around 30% of patients with psoriasis.21 In our study, 28.8% of patients reported joint involvement, but psoriatic arthritis was confirmed in only 10 patients, due to difficult access to rheumatologist and imaging. A study by Aslanian et al22 showed 24% of cases had joint involvement in a group of Brazilian patients with psoriasis and a Spanish study reported a rate of 9.4%.6 A study from Japan by Kawada et al10 obtained the lowest rate of psoriatic arthritis rate (1.0%), and the authors concluded that a genetic factor should be playing a crucial role in psoriatic arthritis in Japan. In our analysis, patients with late–onset disease had slightly more joint involvement than subjects with early-onset disease, but the difference was not statistically significant. Ferrándiz et al6 reported the opposite finding in a study that enrolled more than 1700 individuals.
Health professionals tend to underscore the impact of skin diseases because most of them are not life threatening and have a chronic course.5 Psoriasis fulfills these characteristics and many physicians underestimate patients’ feelings about their condition; nevertheless, it is well known that psoriasis has a major impact on patient QoL.23 Furthermore, psoriasis has been shown to impact patient QoL to the same degree as other more life-threatening disorders such as diabetes, heart disease, and cancer,24 and this has been associated with depression24,25 and suicidal ideation.26 Psoriatic patients report physical discomfort, impaired emotional functioning, a negative body- and self-image, and limitations in daily activities, social contacts, outdoor activities, and work.5,6
Mean DLQI in our patients was 14 (“very large effect” on patient's life). This value is similar to or higher than that reported in the international literature.5 This may be due to disease characteristics (more than 60% of our patients had > 10% BSA affected, and more than 50.0% of patients had involvement of “sensitive areas” such as the face, hands, and genitalia). On the other hand, this score may be due to a Chilean idiosyncrasy. A recent study suggested that psoriatic patients from different countries answer differently on the DLQI, despite having the same grade of underlying health-related QoL impairment.27 Even among native English-speaking patients, some differences were found; this may be due to cultural equivalence or the use of the original DLQI. Sensitive words expressing emotions may be translated but still have different connotations between different cultures. This point may interfere in the comparison between our results and those reported in the international literature.27 Another factor that also may play a role is that scoring categories are interpreted differently in different languages and it is difficult to rank real differences (for example, in Spanish it is difficult to find a word that differentiates between “very much” and “a lot”).27 However, Nijsten et al27 suggest that the DLQI is not comparable between different countries.
Another particular issue in QoL on Chilean patients with psoriasis was the difference in DLQI between men and women. Men were consistently more affected in almost all areas of the questionnaire (Fig. 1). To our knowledge, this finding has not been reported before. It has been reported that psoriatic subjects have no gender differences in any feature, as is the conclusion of a systematic review on QoL on patients with psoriasis.5 It has also been described that there are gender differences in the score of items related to appearance and socialization and that men have greater work-related stress.28 The greater impact of psoriasis on QoL in men may have been influenced by the greater extent of the disease observed in men in our sample. The predominance of men in our sample is surprising because it is unusual in dermatological research. We ruled out the possibility that a selection bias could account for this result; moreover, the proportion of patients who refused to participate in the study was the same for men and women. Hence, we postulate that the greater impact of psoriasis on QoL of men compared with women make them consult more frequently.
QoL in our sample was worse in younger people. This observation is consistent with previous reports.5,28 It has been proposed that shame related to psoriasis is greatest in individuals under 30 years, when they are initiating social relationships and starting their career.28 It has also been suggested that psoriasis has a greater impact on QoL when the disease affects “sensitive areas”, more extended areas, and in the first few years following onset.29 In contrast to reports from a Spanish study,6 we were unable to demonstrate a greater impact on QoL in Chilean patients with early-onset psoriasis. However, we observed a higher DLQI in patients with more recent disease, in patients with facial involvement, and in those with more extensive disease, although the last difference was not statistically significant. In conclusion, it seems that for Chileans, the most affected subgroup is young males with extensive disease or facial involvement during the first few years of the disease.
We could not establish a difference in QoL between patients with or without psoriatic arthritis. Since we used DLQI, this may be due to the fact that this questionnaire was designed for measuring QoL related to skin diseases. A study that enrolled 140 patients with both psoriasis and psoriatic arthritis and 278 patients with cutaneous psoriasis only obtained similar results using another questionnaire (PQOL-12, 12-Item Psoriasis Quality of Life Questionnaire).30 These findings may reflect the intrinsic inadequacy of the QoL instruments used in both studies for capturing the additional burden of joint disease.30
In conclusion, this study verifies that clinical features in Chilean psoriatic patients are comparable to international patterns and that the disease has a negative impact on patient QoL. There was a notable similarity of our findings to the Iberian population; this may be explained by shared genetic factors. Further studies are needed in order to obtain the real prevalence and incidence of the disease and to detail these noteworthy findings in relation to DLQI in Chilean patients with psoriasis.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Valenzuela F, et al. Epidemiology and quality of life of patients with psoriasis in Chile. Actas Dermosifiliogr.2011;102:810-816.