Dermal melanocytosis refers to congenital or acquired lesions characterized by the presence of dendritic cells derived from melanocytes that migrate from the neural crest to the epidermis. The nevus of Ito develops in the territory supplied by the acromioclavicular nerve. Malignant transformation in dermal melanocytosis is extremely rare, with only isolated case reports; only 2 cases of malignant transformation of a nevus of Ito have been reported. We report a very rare case that is the third to be described in the literature. The patient was a 24-year-old man who presented with a subcutaneous nodule that had developed in the anterolateral region of the thorax over the previous 8 months. The nodule was located beneath a faint blue-gray macule with poorly defined borders. Biopsy of the nodule revealed malignant melanoma; biopsies of the adjacent skin lesion showed a diffuse proliferation of scattered melanocytes in a collagen stroma in the reticular dermis. A diagnosis of malignant transformation of a nevus of Ito was made after other possibilities were ruled out.
Las melanocitosis dérmicas son lesiones congénitas y adquiridas caracterizadas por la presencia de células dendríticas que derivan de los melanocitos, que migran de la cresta neural hacia la epidermis.
El nevus de Ito se caracteriza por presentarse en el territorio de inervación del nervio acromioclavicular. La transformación maligna de las melanocitosis dérmicas es extremadamente rara, habiéndose descrito casos aislados de malignización y únicamente dos casos de transformación maligna del nevus de Ito. Presentamos un caso excepcional que representaría el tercero descrito en la literatura.
Se trata de un varón de 24 años que presentó un nódulo subcutáneo en la región anterolateral del tórax de 8 meses de evolución, localizado bajo una mácula pigmentada de color azul grisáceo muy tenue y de bordes mal delimitados. La biopsia del nódulo subcutáneo reveló la presencia de un melanoma maligno, mientras que las biopsias de la lesión cutánea adyacente mostraron en la dermis reticular una proliferación difusa de escasos melanocitos dendríticos en un estroma colagenizado. Descartadas otras posibilidades se realizó el diagnóstico de transformación maligna de nevus de Ito.
The proliferation of dendritic melanocytes in the dermis gives rise to congenital and acquired lesions characterized by the presence of dendritic cells that have migrated from the neural crest towards the epidermis. These lesions are classified as dermal melanocytoses (Mongolian spot, nevus of Ota, and nevus of Ito) and blue nevi. Malignant transformation of dermal melanocytoses is extremely rare, with very few cases reported in the literature.
Case ReportThe patient was a 24-year-old man with a hip prosthesis for a congenital malformation. He consulted for a subcutaneous nodule of about 2cm in diameter that had developed over the previous 8 months in the anterolateral region of the thorax and was clinically compatible with a lipoma. The nodule was excised in the thoracic surgery department; irregular, brownish fragments of firm consistency and with a maximum diameter of 2cm were obtained.
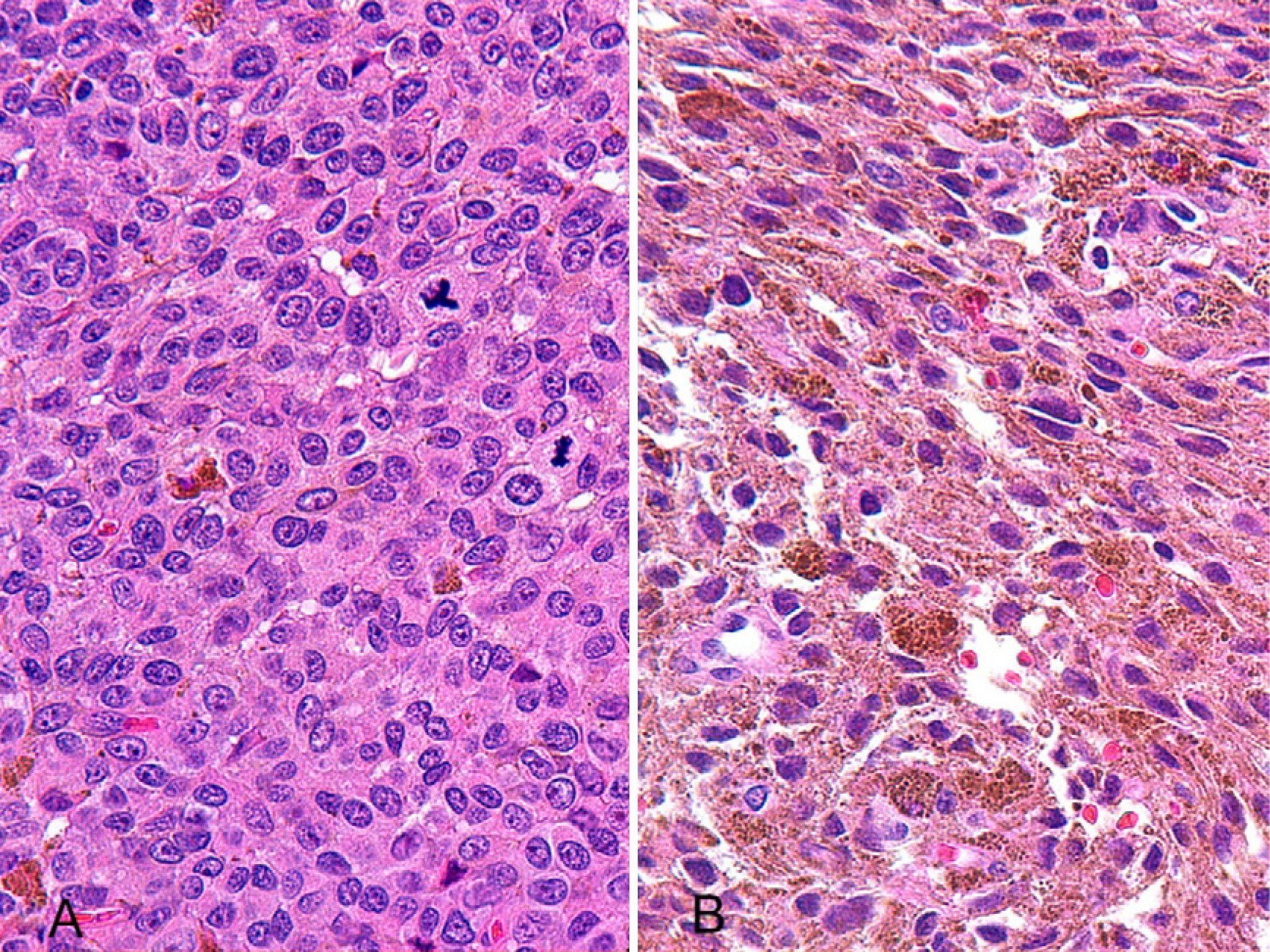
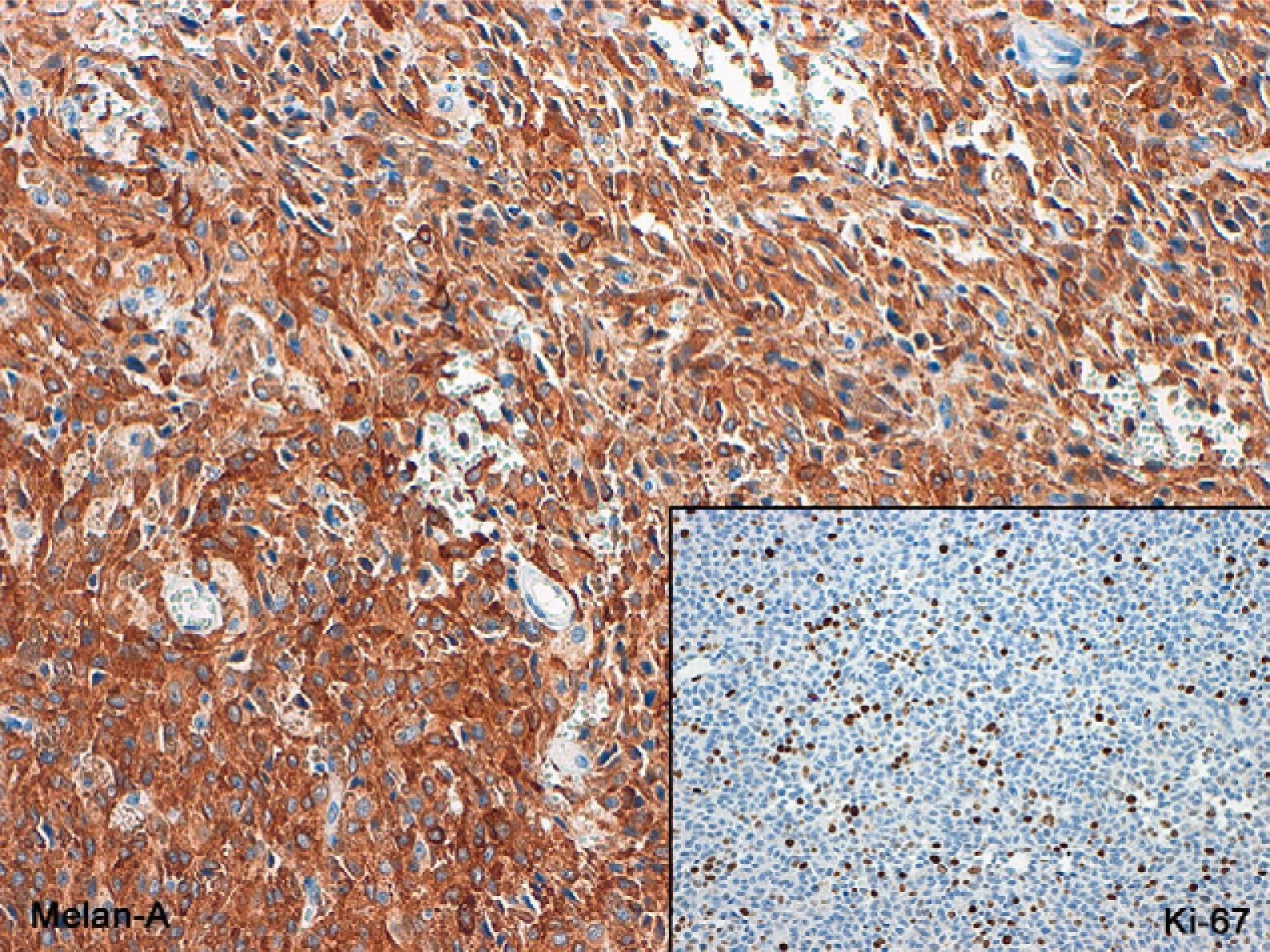
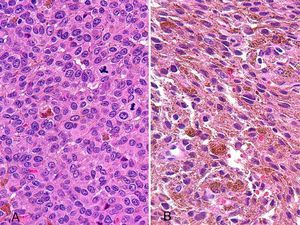
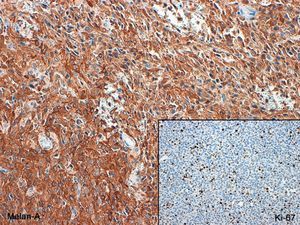
Histology revealed a densely cellular tumor with a diffuse growth pattern. It was formed of medium-to-large cells, some of which were ovoid (Figure 1A), with a vesicular nucleus, prominent nucleolus, and scant cytoplasm that contained melanotic pigment. In other areas the cells were spindle-shaped (Figure 1B), with unclear cytoplasmic borders, oval nuclei with marked anisokaryosis, large nucleoli, and abundant melanin in their cytoplasm. Particularly noticeable was the presence of a large number of mitoses, many of which were atypical, and a small amount of dense fibrous stroma that contained small-caliber vessels, some of which were dilated and congested. These findings were suggestive of malignant melanoma, and the diagnosis was confirmed by the intense immunoreactivity of the tumor cells to S-100, HMB-45 and Melan-A, associated with a high Ki-67 (MIB-1) cell proliferation index (Figure 2).
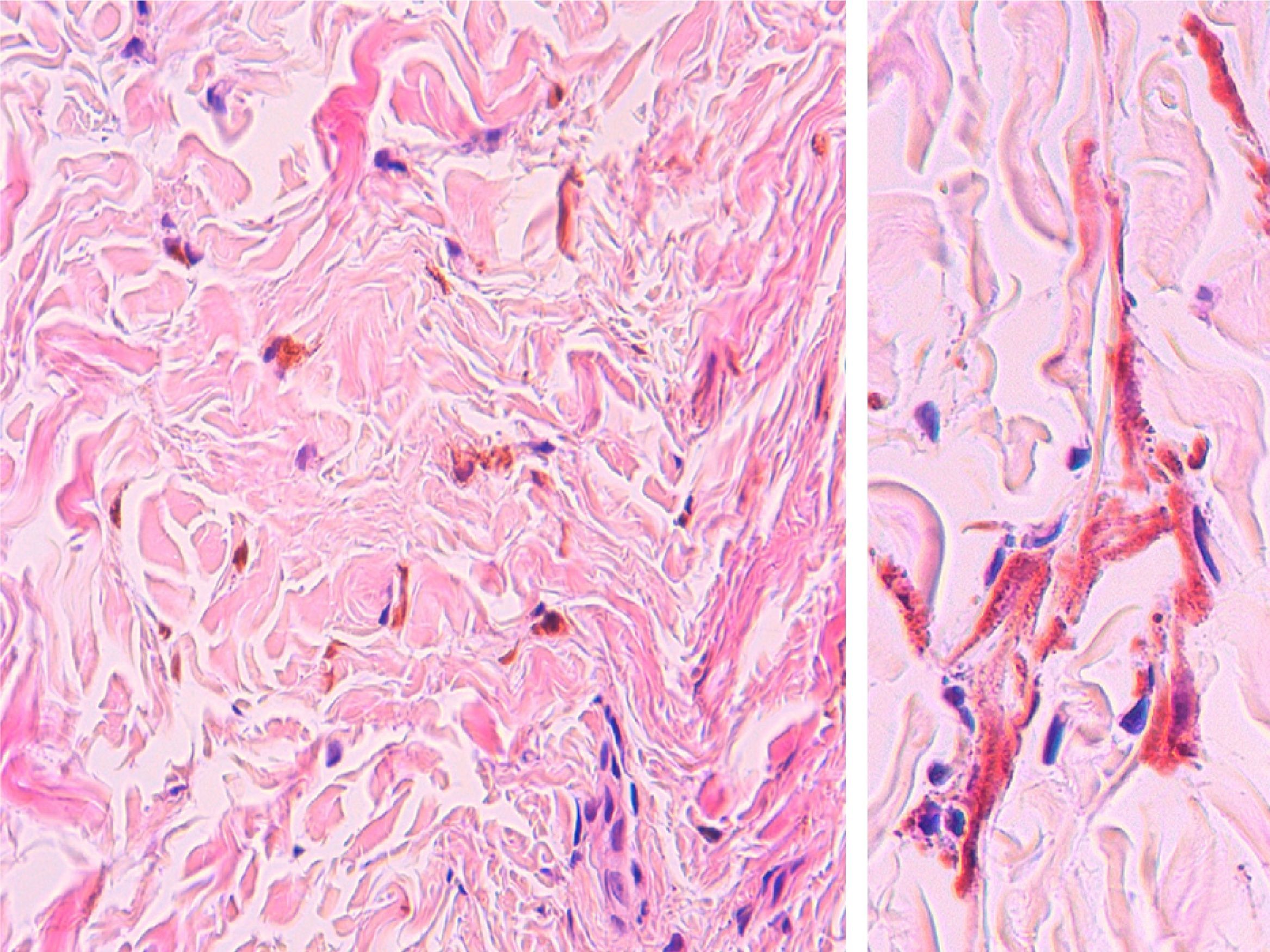
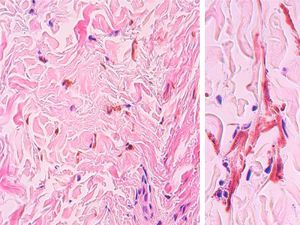
After confirmation of the diagnosis, the skin was examined in detail and a macule 10cm in diameter, composed of smaller, very pale grayish-blue macules a few millimeters diameter (Figure 3), was observed on the anterior aspect of the thorax, in the same area as the subcutaneous tumor described. Dermoscopy of the lesion showed a homogeneous blue coloration with no globules, pigment network, or streaks (Figure 3B). Punch biopsies were performed of 2 pinpoint lesions, one of them close to the scar from the excision of the subcutaneous nodule. Histology revealed the presence of dermal melanocytes with dendritic processes and melanotic pigment in their cytoplasm, with no atypia or mitoses. These cells were present in small numbers in the whole thickness of the dermis, scattered diffusely through a stroma formed of thick bundles of collagen (Figure 4). The epidermis was not affected. A diagnosis of nevus of Ito was made based on the morphology and site of the lesion. When questioned, the patient remembered that the lesion had been present since childhood.
A, Physical examination of the area of the surgical scar in the right pectoral region revealed a 10-cm diameter plaque formed of grayish-blue macules a few millimeters in diameter. B, On dermoscopy, the macules consisted of round, homogeneous blue areas, with no globules, pigment network, or streaks.
Staging studies (upper and lower gastrointestinal endoscopy and computed tomography and positron emission tomography of the thorax) revealed no metastases and also allowed other lesions suggestive of primary melanoma to be excluded. The diagnostic possibilities considered were primary melanoma of the dermis, malignant transformation of a blue nevus, and malignant transformation of a nevus of Ito. The clinical presentation and histology of the melanotic lesion that surrounded the melanoma were different from those of a blue nevus, making malignant transformation of that type of nevus very unlikely. Primary melanoma of the dermis was excluded because of the association with a melanotic lesion, in this case the melanocytosis. The definitive diagnosis was malignant melanoma on a melanocytosis, that is, malignant transformation of a nevus of Ito.
DiscussionMelanocytoses are benign pigmented lesions that are congenital or acquired in childhood. They are characterized by the presence of dendritic cells derived from the melanocytes that migrate from the neural crest towards the epidermis. A number of clinical forms have been described, although the most common are the Mongolian spot, nevus of Ota, and nevus of Ito, which are only differentiated by their location. The nevus of Ota is distributed between the first and the second branches of the trigeminal nerve and the nevus of Ito is located in the area supplied by the acromioclavicular nerve.1
Malignant transformation of the melanocytoses, though very rare, has been reported in cases of nevus of Ota and, more frequently, in blue nevi.2–4 Only 2 cases of malignant transformation of a nevus of Ito have been published.5,6 The diagnosis can only be made after excluding other possibilities, as we did in our case, considering metastasis from a primary melanoma at another site (skin or mucosa), primary dermal melanoma, and malignant transformation of a blue nevus.
Because of the small number of cases described in the literature, the ideal treatment and the prognosis of these lesions remain unclear, particularly as staging can be complicated, as is also the case in primary dermal melanomas, in which the absence of epidermal involvement makes use of the Breslow depth controversial. In primary dermal melanoma, depending on the series reported, some authors measure the Breslow depth as in a conventional melanoma,7 despite no surface involvement, and others simply ignore it and use the Clark level as reference.8 In the 2 similar cases reported, the treatment and prognosis were considered to be comparable to those of a conventional melanoma.9
Our patient was treated surgically, with resection of the area of the nevus of Ito and the underlying tumor; 2 operations were required as the tumor infiltrated extensively into the muscle plane. In addition, the findings of selective sentinel lymph node biopsy from the right axilla were negative. This was therefore a locally advanced melanoma with no detectable lymph node or blood-borne metastases. The patient refused adjuvant treatment with interferon, and we therefore decided to perform 3-monthly follow-up. Two local recurrences were detected over a period of 18 months, with tumor infiltration reaching the parietal pleura, requiring the resection of 2 ribs, sternum, and pleura (Figure 5). The patient is disease-free at the time of writing and continues periodic follow-up.
This is the third case of malignant transformation of a nevus of Ito reported in the literature. Although malignant transformation of the melanocytoses in general, and of nevus of Ito in particular, is very rare, we consider these lesions warrant close follow-up and monitoring.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Martinez-Peñuela A, et al. Transformación maligna de un nevus de Ito: descripción de un caso extraordinario. Actas Dermosifiliogr.2011;102:817-820.