Ixekizumab has proven efficacy and safety for the treatment of psoriasis in clinical trials. The aim of this study was to evaluate its effectiveness and safety in routine clinical practice.
MethodsRetrospective study of all patients treated with ixekizumab in 2 dermatology departments in the city of Valencia, Spain.
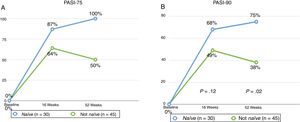
ResultsSeventy-five patients (53.3% men and 46.7% women) with a mean age of 48.61 years were studied; 77.3% (n = 58) had plaque psoriasis and 22.7% (n = 17) had psoriasis predominantly affecting a specific area. The most common comorbidity was obesity (present in 48% of patients) and 40% of the overall group had not been previously treated with a biologic drug. Mean psoriasis area and severity index (PASI) fell from 9.99 at baseline to 1.5 at week 16. PASI-75 and PASI-90 (improvements of at least 75% and 90% in PASI) were independent of sex, age, baseline PASI, and the comorbidities analyzed. Responses at week 16 and 52 were significantly better in biologic-naïve patients for the overall group and the subgroup of patients with localized psoriasis. Adverse effects were reported for 25.7% of patients and the most common effect was injection-site reaction. There were no serious adverse effects.
ConclusionsOur findings show that ixekizumab is both effective and safe in the treatment of psoriasis in routine clinical practice.
Ixekizumab es un fármaco efectivo y seguro en el tratamiento de pacientes con psoriasis dentro de ensayos clínicos. Nuestro objetivo es valorar la eficacia y seguridad de ixekizumab en la práctica clínica habitual.
MaterialEstudio retrospectivo incluyendo todos los pacientes que han recibido ixekizumab en 2 servicios de dermatología de la ciudad de Valencia.
ResultadosSe incluyeron un total de 75 pacientes, siendo el 53,3% varones y el 46,7% mujeres con una edad media de 48,61 años. El 77,3% (58 pacientes) presentaba una psoriasis en placas, mientras que el 22,7% (17 pacientes) presentaba psoriasis de predominio en un área especial. La comorbilidad más frecuente fue obesidad en el 48% de ellos y el 40% eran naive a biológicos. El PASI inicial medio fue de 9,99, mientras que el PASI medio a la semana 16 era de 1,5. Las respuestas de PASI75 y PASI90 fueron independientes de las comorbilidades analizadas, del sexo, de la edad y del PASI basal. Los pacientes naive a biológicos respondieron mejor que los pacientes que habían recibido tratamiento biológico previo, tanto en la semana 16 como en la semana 52 de forma estadísticamente significativa. Estas observación también se mantuveroni en los pacientes con psoriasis en un área especial. El 25,7% de los pacientes refería algún efecto adverso, siendo lo más frecuente reacción en el sitio de inyección. No se observaron reacciones adversas graves.
ConclusionesEl estudio plasma nuestra experiencia en la práctica clínica real de ixekizumab, siendo un fármaco efectivo y seguro para el tratamiento de la psoriasis.
Psoriasis is a systemic inflammatory autoimmune disease that follows a course of exacerbations followed by remissions. It mainly affects the skin and joints, although comorbidities associated with this disease are increasing.1 In recent years, the development of biologic or targeted therapies has drastically changed treatment of these patients.
Ixekizumab is a humanized recombinant biologic agent that acts against IL-17A and that was recently approved for use in patients with plaque psoriasis.2 The efficacy and safety of this drug have been evaluated in randomized clinical trials, although data on its use in routine clinical practice are limited.3,4
The primary objective of this study was to assess the efficacy and safety of ixekizumab in patients with psoriasis in routine clinical practice in Spain. A secondary objective was to assess different potential clinical variables that may influence therapeutic efficacy.
Material and MethodsThis was a retrospective observational study that included all patients with psoriasis who had received treatment with ixekizumab in 2 dermatology departments in Valencia, Spain, between March 2017 and September 2018. The variables collected were sex, age, previous treatments (whether conventional systemic agents or biologic agents), comorbidities, predominant involvement of a difficult-to-treat location (palmoplantar sites, genitals, scalp), and adverse effects, as well as discontinuation of treatment with the reason. Psoriasis severity was assessed using the Psoriasis Area and Severity Index (PASI), at baseline, week 16, and the end of study follow-up. The Dermatology Quality of Life Index (DLQI) was also employed. PASI-75 and PASI-90 were defined as an improvement of 75% and 90%, respectively, compared with the baseline PASI. The duration of follow-up of each patient varied according to when they had started treatment.
A descriptive statistical analysis was undertaken of all variables, using the mean and SD for quantitative variables and percentages for qualitative variables. Hypothesis testing used the Chi-squared test or the Fisher exact test as appropriate. The impact of sex, age, prior treatment, comorbidities, and baseline PASI was assessed using a multivariate analysis. Statistical data were analyzed using the SPSS program, version 21.0, and P < .05 was considered significant.
ResultsA total of 75 patients were included, of whom 53.3% were male and 46.7% were female, with a mean (SD) age of 48.61 (13) years. The clinical and epidemiological characteristics of the patients are summarized in Table 1 and Table 2. All patients, except 2 without an induction dose, received ixekizumab as indicated in the Summary of Product Characteristics. Overall, 76% of patients had at least 1 comorbidity, with the most frequent being obesity as defined by a body mass index≥30mg/kg2 (48%), followed by dyslipidemia (45.3%), smoking habit (37.3%), and nonalcoholic fatty liver disease (40%). Other comorbidities reported were hypertension (22.7%), psychiatric disorders in the form of anxiety and major depression (22.7%), type II diabetes mellitus (16%), hyperuricemia (17.3%), psoriatic arthritis (16%), hypothyroidism (4%), prior hepatitis B virus infection (2.6%), major cardiovascular events (2.6%), cirrhosis (1.3%), and Moyamoya disease (1.3%). No patients had a history of inflammatory bowel disease.
Clinical-Epidemiological Characteristics of Patients Included in the Study.
| Patients included in study (n=75) | |
|---|---|
| Sex, n (%) | |
| Male | 40 (53.5%) |
| Female | 35 (46.7%) |
| Age, y (mean±SD) | 48.61±13 |
| Psoriasis site, n (%) | |
| Plaques | 58 (77.3%) |
| Difficult-to-treat locations | 17 (22.7%) |
| Comorbidities | |
| Obesity | 36 (48%) |
| Dyslipidemia | 34 (45.3%) |
| Smoking habit | 28 (37.3%) |
| NAFL | 30 (40%) |
| Hypertension | 17 (22.7%) |
| Psychiatric disorder | 17 (22.7%) |
| DM2 | 12 (16%) |
| Hyperuricemia | 13 (17.3%) |
| PsA | 12 (16%) |
| Baseline PASI (mean±SD) | 9.99±5.13 |
| Prior treatments, n (%) | 60 (80%) |
| Phototherapy | 17 (22.7%) |
| Conventional systemic/smallmolecule | 60 (80%) |
| Methotrexate | 49 (65.3%) |
| Acitretin | 18 (24%) |
| Ciclosporin | 11 (14.7%) |
| Apremilast | 10 (13.3%) |
| Fumaric acid | 1 (1.3%) |
| Biologics | 45 (60%) |
| Ustekinumab | 32 (42.7%) |
| Secukinumab | 20 (26.7%) |
| Etanercept | 18 (24%) |
| Adalimumab | 15 (20%) |
| Infliximab | 8 (10.7) |
| Efalizumab | 5 (6.7%) |
| Certolizumab | 2 (2.7%) |
| Golimumab | 2 (2.7%) |
| Brodalumab | 1 (1.3%) |
Abbreviations: DM2, type 2 diabetes mellitus; NAFL, nonalcoholic fatty liver; PsA, psoriatic arthritis
Clinical-Epidemiological Characteristics of Patients With Psoriasis in Difficult-to-Treat Locations Treated with Ixekizumab.
| Patients With Psoriasis in Difficult-to-Treat Locations | |
|---|---|
| (n=17) | |
| Sex, n (%) | |
| Male | 7 (41.2%) |
| Female | 10 (58.2%) |
| Age, y (mean±SD) | 47±14 |
| Difficult-to-treat location, n (%) | |
| Palmoplantar | 7 (41.2%) |
| Genital | 7 (41.2%) |
| Scalp | 3 (17.6%) |
| Baseline PASI (mean±SD) | 5±1.3 |
| Baseline PGA (mean±SD) | 3±0.5 |
| Baseline DLQI (mean±SD) | 19±5.7 |
| Prior treatments, n, % | 10 (58.8%) |
| Conventional systemic/small molecule | 1 (5.9%) |
| Biologics | 9 (52.9%) |
The mean (SD) baseline PASI was 9.99 (5.13) and the mean (SD) PASI at week 16 was 1.5 (2.3). PASI-75 and PASI-90 were achieved by 73.3% and 56% of patients, respectively, at week 16. These responses were independent of comorbidities, including BMI>30mg/kg2 and of having received prior biologic therapy. The percentage of patients who achieved PASI-75 at week 16 was higher in patients who were naïve to biologic agents (P=.03).
At the end of the study, the median follow-up duration was 46 weeks, at which point 89.3% of patients had completed 24 weeks of treatment, 40% had completed 52 weeks of treatment, and PASI-75 and PASI-90 were achieved by 74.6% and 62.7% of patients, respectively. Of the patients who completed 52 weeks of treatment, 73.3% and 56.7% achieved PASI-75 and PASI-90, respectively. At week 24 and week 52, efficacy responses were independent of sex, age, smoking habit, dyslipidemia, diabetes mellitus, psoriatic arthritis, psychiatric disorder, hyperuricemia, and obesity. However, the biologic-naïve patients had higher rates of both PASI-75 and PASI-90 compared with patients who had been treated previously with a biologic agent (Fig. 1).
Of the 17 patients with psoriasis located predominantly on a difficult-to-treat area, 35.3% and 29.4% achieved PASI-75 and PASI-90, respectively, at week 16. At the end of the study, 15 patients had completed week 24, of whom 40% and 33.3% had achieved PASI-75 and PASI-90, respectively. Of the 9 patients who completed 52 weeks, 44.4% achieved PASI-75 and PASI-90. Mean physician global assessment (PGA) was 1.3 at week 16 and 0.8 at week 52. Mean DLQI was 3.2 at week 16 and 2.4 at week 52. The percentage of patients who achieved PASI-75 and PASI-90 at week 52 was higher in patients who were naïve to biologic agents (P=.001) (Fig. 1B).
Of the 75 patients included in the study, 25.7% reported an adverse effect, with the most frequent being injection-site pain (18.6%) followed by mucocutaneous candidiasis (5.6%). Other adverse effects reported were general malaise and asthenia (2 patients), rhinoconjunctivitis (2 patients), canker sores (1 patient), pharyngitis (1 patient), and arthritis of the knee (1 patient). At the end of follow-up, 89.3% of patients remained on treatment whereas 10.7% (8 patients) had discontinued treatment, 2 due to adverse reactions (uncontrolled rhinoconjunctivitis and injection site reaction), 3 for primary treatment failure, 2 for secondary failure, and 1 because of desire to become pregnant. Of the remaining patients who were still on treatment (67 patients), 2 had undergone dose intensification with ixekizumab every 15 days, 2 were receiving the agent in combination with methotrexate, and 1 had undergone ixekizumab dose deintensification to administration every 6 weeks because of achieving complete clearance sustained over time.
DiscussionOur study demonstrates the efficacy and safety of ixekizumab in routine clinical practice in patients with psoriasis, whether psoriasis vulgaris or psoriasis at difficult-to-treat locations. The efficacy of ixekizumab 40mg every 12 weeks has been evaluated in several randomized clinical trials (UNCOVER-1, UNCOVER-2, and UNCOVER-3), with 81.6% of patients attaining PASI-75, 63.3% attaining PASI-90, and 33.2% attaining PASI-100 at week 12. The patients in our study are comparable with those in clinical trials, with the exception of baseline PASI (9.99 vs 20.3) and the fact that patients had received prior biologic therapy (26.4% vs 60%).3
The efficacy of ixekizumab in routine clinical practice has been evaluated in several studies. Diotallevi et al.5 reported responses at week 12 of 80% of patients with PASI-75, 13% with PASI-90, and 6.9% with PASI-100, although the sample size was limited to 15 patients. In a series of 60 patients published by Georgakopoulos et al.,6 75% of patients attained PASI-75 or PGA 0 or 1 at 12 weeks of treatment, with a mean baseline PASI of 2.3. In Spain, the efficacy in routine clinical practice has been assessed in a study published by Deza et al.,4 in which the percentages of patients who attained PASI-75, PASI-90, and PASI-100 at week 12-16 were 87.5%, 50%, and 39.9%, respectively. Our results at week 16 are similar to those reported previously, with responses of 73.3% and 56% of patients attaining PASI-75 and PASI-90, respectively.
In the same study by Deza et al.,4 the results were sustained at week 24 (n=77) but then decreased slightly at week 52 (n=41), with the percentage of patients who attained PASI-75, PASI-90, and PASI-100 of 79.1%-60.7%, 52.3%-42.9%, and 41.9%-30.4%, respectively.4 In our study, 74.6% and 62.7% of the patients analyzed at week 24 (67 patients) attained PASI-75 and PASI-90, respectively, while 73.3% and 56.7% of patients analyzed at week 52 (30 patients) achieved this outcome. These findings are consistent with previously published results in Spain.
Our data also confirm the efficacy of this drug in locations that usually have poorer response, such as the scalp, genital region, or palmoplantar region. Involvement of these areas only occurs in 50% of patients at any given time of the disease, and may seriously impact the patient's quality of life.7 Moreover, there are few clinical trials of the efficacy of different drugs.8 There are no clinical trials that specifically assess the efficacy of ixekizumab in the palmoplantar region or the scalp. Furthermore, double-blind, placebo-controlled, randomized clinical trials have demonstrated the efficacy of ixekizumab in genital psoriasis,9 as well as its rapid action and improvement in the sexual quality of life.10 In our study, 33.3% of patients with psoriasis in these sites achieved PASI-90 as well as a decrease in DLQI of 84% at week 16 of treatment.
Efficacy in our study was independent of sex, age, smoking habit, comorbidities assessed, and baseline PASI. Of note is that obesity or BMI>30mg/kg2, in contrast to other biologic agents, does not seem to have an impact on ixekizumab response in routine clinical practice, as also reported by Deza et al.4 The only variable that does have an influence on efficacy of ixekizumab in clinical practice in our patients is having received prior treatment with another biologic agent, also in line with the findings of other studies. This observation, although with few patients, is also valid for patients with psoriasis with the main involvement at difficult-to-treat sites.
The rate of adverse effects reported in our patients is 25.7%, and these findings are similar to those published both in clinical trials and in routine clinical practice, with the most frequent being pain or injection site reaction.3,4,6 Furthermore, this adverse effect was more frequent in the first patients treated. With the change to the mode of administration (from prefilled pen to prefilled syringe), this problem was reduced considerably. Candidiasis, an adverse class effect of IL-17 inhibitors,2 was the second most frequent adverse effect. Of note are 2 episodes of rhinoconjunctivitis reported in our series, in one case uncontrolled, and that led to withdrawal of therapy. Although clinical trials have reported nasopharyngitis as the most frequent adverse effect (23.5%), in our series, the chronic episodes of rhinitis and nonallergic conjunctivitis were the most frequent. On the other hand, although not reported in clinical trials, one of our patients presented with arthritis of the knee, as observed in the series published by Deza et al.4 Finally, no serious adverse effects were reported in our study, although a low percentage (1%) of patients in clinical trials experienced serious events such as grade 3-4 neutropenia and inflammatory bowel disease.3
The limitations of our study are those inherent to a retrospective, observational study, with loss of data or missing data. We also did not assess the duration of psoriasis as a factor related to the efficacy of treatment. In addition, given that not all patients completed 52 weeks of treatment, we cannot draw solid conclusions on the long-term efficacy and safety in routine clinical practice.
In conclusion, we present the second largest series of patients treated with ixekizumab, both for psoriasis vulgaris and for psoriasis in difficult-to-treat locations. Our study shows similar efficacy and adverse effect rates to those published in clinical trials and in studies in the clinical practice setting. The efficacy of ixekizumab does not depend on comorbidities usually analyzed in patients, and is lower in patients with previous exposure to biologic agents.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Magdaleno-Tapial J, Carmena-Ramón R, Valenzuela-Oñate C, Ortiz-Salvador JM, Sabater-Abad J, Hernández-Bel P, et al. Efficacy and Safety of Ixekizumab in a Real-Life Practice: A Retrospective Bicentric Study. Actas Dermosifiliogr. 2019;110:585–589.