Primary recurrent cutaneous eosinophilic vasculitis is a rare condition characterized by pruritic, erythematous, purpuric plaques associated to edema. We compared and analyze the clinical, dermoscopic and histological features of the disease in 4 patients from our hospital and 13 patients published in the literature. Seventeen patients were included, with a median age of 56yo, a median duration of disease of 6 months. Lesions were most frequently generalized (47%) or localized in lower limbs (41%). The most frequent features were purpuric color (71%), local edema (65%), necrotizing vasculitis (94%) and eosinophil infiltration (100%) in histology. Most of the patients (82.4%) were given oral steroids with a median dose of 30mg. Primary recurrent cutaneous eosinophilic vasculitis might be an infra-diagnosed condition. The analysis of the patients allowed us to propose diagnostic criteria for the definition of this disease. We suggest a therapeutic strategy with high-potency steroids and dapsone, which might be considered as first-line treatment.
La vasculitis eosinofílica recurrente cutánea primaria es una enfermedad rara, caracterizada por placas purpúricas, eritematosas y pruriginosas asociadas a edema. Comparamos y analizamos las características clínicas, dermatoscópicas e histológicas de la enfermedad en 4 pacientes de nuestro hospital y en 13 casos de pacientes publicados previamente. Se incluyeron 17 pacientes, con una mediana de edad de 56 años, y una mediana de duración de la enfermedad de 6 meses. En la mayoría de los casos las lesiones fueron generalizadas (47%) o localizadas en los miembros inferiores (41%). Las características histológicas más frecuentes fueron: color purpúrico (71%), edema local (65%), vasculitis necrosante (94%) e infiltración eosinofílica (100%). La mayoría de los pacientes (82,4%) recibió esteroides orales (mediana de la dosis de 30mg). La vasculitis eosinofílica recurrente cutánea primaria podría ser una entidad clínica infradiagnosticada. El análisis de los pacientes nos permitió proponer algunos criterios diagnósticos para su definición. Recomendamos una estrategia terapéutica con esteroides de alta potencia y dapsona, pudiéndose considerar como el tratamiento de primera línea.
Recurrent cutaneous eosinophilic vasculitis (RCEV) is a rare condition recently described and characterized by the presence of pruritic, purpuric, erythematous plaques and papules associated to edema, especially on lower extremities. Histopathology findings show necrotizing vasculitis of small vessels with infiltration of numerous eosinophils. RCEV has a good response to corticoid therapy with rapid recurrence after suspension of treatment.1
Chen et al.1 in 1994 originally described RCEV as an idiopathic or primary entity. Incidence is unknown since only 13 primary RCEV cases have been reported in the literature.3 We firmly believe that RCEV diagnosis has been underestimated, since it has been recently described and we lack specific diagnostic criteria.
We aim to review the clinical, dermoscopic and histological features of the patients from our hospital with the diagnosis of primary RCEV and compare the findings to those reported in the literature in order to describe this condition.
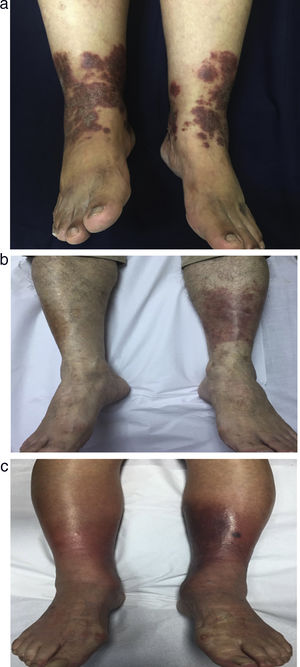
CasesCase 1 (Fig. 1a) was a 61-yo. woman with a two year history of pruritic, erythematous and purpuric macules, plaques and edema of lower limbs, with dermographism reaching the thighs. Lesions were progressively ascending to trunk, with heliotrope-like lesions on the face (Table 1). Treatment was initiated with oral and topical corticosteroids with good results. However, recurrence was evident after tapering of corticosteroids. Patient was maintained with intermittently oral and topical corticosteroids during the flares with good response after six months of treatment.
Case 1, a 61 yo female patient with (a) bilateral erythematous-purpuric plaques in lower limbs. (b) Case 3, a 78 yo male patient with unilateral, erythematous, purpuric plaque in posterior right lower limb. (c) Case 4, a 88 yo female patient with bilateral, erythematous, purpuric plaques in lower limbs.
Recurrent Cutaneous Eosinophilic Vasculitis cases.
| N° | Author, year | Sex-Age | Duration | Localization | Description | HP | Blood tests | Treatment | Follow-up |
|---|---|---|---|---|---|---|---|---|---|
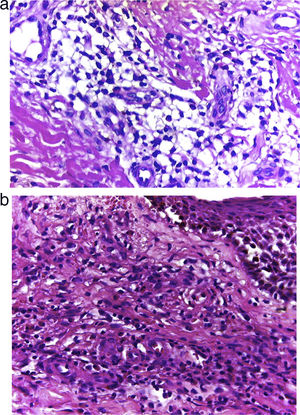
| 1 | Case 1 | 61 - F | 24 m | Generalized | Bilateral, erythematous-purpuric plaques in lower limbs with edema and pain. Purpuric plaques and dermographism on the face, thighs and arms. | Hyperkeratosis and spongiosis of the epidermis. Diffuse infiltration of lymphocytes and eosinophils in the superficial and deep dermis, with the presence of fibrinoid necrosis of the vessels of the superficial dermis with the presence of abundant eosinophils both dispersed and invading the wall of vessels. No leukocytoclasia (Fig. 2a). | Eosinophilia 0.7 x 109/L; CRP 13 mg/L. Stools analysis positive for Giardia lamblia. No other significant abnormalities (ANCA negative). | Oral deflazacort 30mg and topical clobetasol 0.05%. When oral corticosteroids suspended, symptoms relapsed. Maintained with intermittent topical and oral corticosteroids. | Six months with no recurrence. |
| 2 | Case 2 | 66 - F | 12 m | Lower limbs | Poorly delimited erythematous-purpuric plaque in left lower limb. Unilateral edema, pruritus and pain. | Spongiosis of the epidermis, diffuse infiltration of the superficial and deep dermis, with fibrinoid necrosis of the vessels of the superficial dermis, and eosinophils both dispersed and invading the wall of necrotic vessels (Fig. 2b). | Eosinophilia 0.4 x 109/L; CRP 10 mg/L, urine analysis positive for Echerichia coli. No other significant abnormalities (ANCA negative). | Deflazacort 30 mg/day and topical clobetasol 0.05% for two weeks. After tapering of oral steroids, lesions recurred. Dapsone 100 mg/day was initiated with deflazacort 30 mg/day, and then tapered with control of symptoms. | Eight months with no recurrence. |
| 3 | Case 3 | 78 - M | 6 m | Lower limbs | Bilateral, poorly delimited, edematous, erythematous, purpuric and pruritic plaques on the right lower limb. | Small vessels of the dermis with fibrinoid necrosis. Infiltrate of vessels rich in eosinophils with minimal or no leukocytoclasia and extravasation of erythrocytes. | Eosinophilia 0.8 x 109/L; IgE 161.2 ug/L, CRP 10 mg/L. No other significant abnormalities (ANCA negative). | Deflazacort 30mg for two weeks and clobetasol 0.05% topical BID for two weeks. After tapering, lesions remitted, and patient was under 6mg of deflazacort chronically. | Six months with no recurrence. |
| 4 | Case 4 | 88 - F | 1 m | Lower limbs | Bilateral erythematous, purpuric, pruritic and painful plaques, poorly delimited and edematous. | Small vessels of the dermis with fibrinoid necrosis. Infiltrate of vessels rich in eosinophils with minimal or no leukocytoclasia and extravasation of erythrocytes. | ESR 32 mm/h. No other significant abnormalities (ANCA negative). | Dapsone 100mg is initiated with control of lesions. | Six months with no recurrence. |
Abbreviations
HP: histopathology; F: female; M: male; m: months; w: weeks; ESR: erythrocyte sedimentation rate; CPR: C-Reactive Protein; IgE: Immunoglobulin E; ANA: antinuclear antibodies; ANCA: anti-neutrophil cytoplasmic antibodies; CT: computerized tomography; LDH: lactate dehydrogenase; BID: two times a day.
Case 2 is a 66-yo. woman with one-year history of pruritic, painful and poorly delimited erythematous purpuric plaque in the left lower limb, with local edema (Table 1). Treatment with oral and topical corticosteroids had good results after one month, but recurrence occurred after corticosteroids suspension. Dapsone 100mg was initiated with control of lesions after one month, with no recurrence at eight months of follow-up.
Case 3 (Fig. 1b) is a 78-yo. male patient with a six months history of a pruritic, well delimited purpuric erythematous plaque on the posterior right leg associated with mild edema (Table 1). Deflazacort 30mg was initiated, with deflazacort 6mg as maintenance therapy.
Case 4 (Fig. 1c) is a 88-yo. female patient with a one month history of bilateral pruritic, painful, edematous, purpuric and erythematous plaques on lower limbs (Table 1). Oral and topical corticosteroids were started with recurrence after corticosteroids tapering. Dapsone 100mg controlled the lesions after two months, with no recurrence at six months of follow-up.
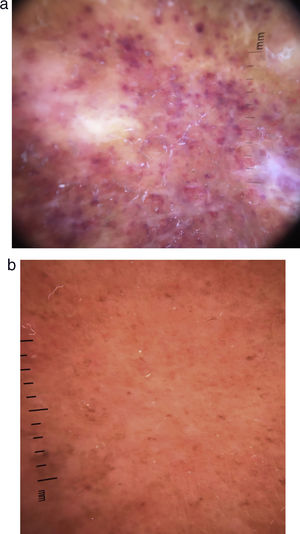
Review of RCEV casesThirteen cases were retrieved from literature (ver material suplementario). From the seventeen cases included, 14 (82%) were females (Table 2). The median age was 56 yo. (interquartile range IQR36-78), with a median duration of disease of 6 mo. (IQR1-12). Lesions were frequently generalized (47%), or distributed mostly in lower limbs (41%), characterized as plaques (64.7%), papules (52.9%), with a purpuric (70.6%) and erythematous (64.7%) color. Lesions were mostly pruritic (88.2%), with local or distal edema and angioedema (64.7%), symptoms used for follow-up control. Dermoscopy findings were purpuric dots and globules immerse in an irregular orange-red background (Fig. 3a and b). Laboratory results showed a median of eosinophil count of 3.4 x 109/L (IQR0.8–4.3) and RCP of 13.75mg/L (IQR10.0–30.1). The most frequent treatment was oral corticosteroids (82.4%), mostly prednisone (47.1%) with a median dose of 30mg (IQR20–60). Recurrence of lesions after the tapering or discontinuation of oral steroids was frequent (70.6%). The median time of follow-up with no recurrence of lesions was 6 months (IQR1–12).
Descriptive analysis of the seventeen cases included in the review.
| Median | IQR25-75% | N=17n(%) | |
|---|---|---|---|
| Sex female | 14(82.4) | ||
| Age | 56 | 36;78 | |
| Duration | 6 | 01;12 | |
| Dose of oral CE | 30 | 20;60 | |
| Follow-up | 6 | 1;12 | |
| Recurrence after CE | 12(70.6) | ||
| Distribution | Generalized | 8(47.1) | |
| Upper limbs | 2(11.8) | ||
| Lower limbs | 7(41.1) | ||
| Symptoms | Pruritus | 15(88.2) | |
| Pain | 4(23.5) | ||
| Findings | Color | Erythematous | 11(64.7) |
| Purpuric | 12(70.6) | ||
| Primary lesion | Plaque | 11(64.7) | |
| Papule | 9(52.9) | ||
| Ulcer | 4(23.5) | ||
| Urticarial like | 4(23.5) | ||
| Patch | 1(5.9) | ||
| Nodule | 1(5.9) | ||
| Other | Edema - angioedema | 11(64.7) | |
| Fever | 2(11.8) | ||
| Lymph node enlargement | 1(5.9) | ||
| Histology findings | Eosinophil infiltration | 17(100) | |
| Necrotizing vasculitis | 16(94.1) | ||
| No leukocytoclasia | 7(41.1) | ||
| Steroid use | 16(94.1) | ||
| Deflazacort | 4(23.5) | ||
| Prednisone | 8(47.1) | ||
| Topical | 2(11.8) | ||
| Other | 2(11.8) | ||
| None | 1(5.9) | ||
| Additional therapy | 7(41.1) | ||
| Dapsone | 2(11.8) | ||
| Colchicine | 1(5.9) | ||
| Indomethacin | 1(5.9) | ||
| Tosilate | 1(5.9) | ||
| Tacrolimus | 1(5.9) | ||
| Glycyrrhizin | 1(5.9) | ||
| Lab results | |||
| Eosinophil count | 3.4 | 0.8;4.3 | 13(76.5) |
| ERS | 61 | 32;107 | 7(41.1) |
| CPR | 13.75 | 10;30.1 | 6(35.3) |
| IgE | 218 | 161;658 | 5(29.4) |
RCEV is an infra-diagnosed condition difficult to treat. Literature lacks of epidemiologic data.1,2 According to the 2012 International Chapel Hill Consensus,3 RCEV is a single-organ vasculitis (SOV). However, some patients with SOV might develop additional disease manifestations that warrant redefining the case as a systemic vasculitis.3
RCEV pathophysiology demonstrates that there is a selective recruitment and activation of eosinophils due to the increase of cytokines such as interleukin (IL) 5, IL-3, granulocyte-macrophage colony-stimulating factor and platelet-activating factor.4,5 As two patients had current infections, we believe that infections could act as a trigger for this entity, or as an element of aggravation or persistence.6
Clinical findingsOur patients were mostly females, with pruritic, purpuric and erythematous papules and plaques mostly in the lower limbs, with local or distal edema (Fig. 1a to c). These symptoms are very similar between the patients described in other case reports (Sup. Table 1) and those presented by Sawada et al.2
HistologyThe histological findings, first described first by Chen et al.,1 and repeated in the following reports, found in all cases necrotizing vasculitis of small dermal vessels with fibrinoid necrosis, eosinophilic infiltration along the dermis with minimal or no leukocytoclasia (Fig. 2a and b). The epidermis is usually normal except for occasional spongiosis with eosinophilic infiltration.1
Lab resultsEosinophilia2,7 was important, but not essential8,9 with a median blood count of 3.4 x109/L (Table 2) without correlation to severity of symptoms; different from other disorders in which eosinophilia is even greater, such as HES and episodic eosinophilic angioedema.6
DermoscopyDermoscopic findings, spots and purpuric globules in an irregular red-orange background (Fig. 3a and b), have been described in other forms of vasculitis, such as urticarial vasculitis.10 The purpuric spots and globules correspond to damage superficial dermal vessels with extravasation of red blood cells (necrotizing vasculitis).10 As fibrinoid necrosis is difficult to find in histology, dermoscopic areas of vascular damage would help with the biopsy location.
DiagnosisBased on the findings described by previous authors, and presented in this review, we propose as major criteria: (i) erythematous-purpuric and pruritic plaques and/or papules; (ii) fibrinoid necrosis of dermis vessels with infiltration of eosinophils into the dermis and/or vessel walls in histology; (iii) response to systemic corticosteroids and/or high potency topical corticoids. Among the minor criteria, we suggest: (i) local or distal edema/angioedema; (ii) eosinophilia; (iii) purpuric spots on dermoscopy; (iv) recurrence of lesions after suspension and/or tapering of treatment with corticosteroids; (v) exclusion of another entity that explains the invasion of eosinophils in the skin. The diagnosis would be made with three major criteria and at least one minor criteria, or two major criteria and at least three minor criteria. The clinical and histologic findings are mandatory.
The differential diagnoses are mainly HES, Wells syndrome, and episodic eosinophilic angioedema.1,5 They are all characterized by invasion of eosinophils in the dermis of the affected skin, however no necrotizing vasculitis is found.6 Churg–Strauss syndrome (CSS) is characterized by a spectrum of neutrophilic vasculitis in ANCA-positive patients at one end, to eosinophilic vasculitis in ANCA-negative patients at the other end, whereas a mixed infiltrate of both eosinophils and neutrophils is most often found. Patients with RCEV might represent an ANCA-negative CSS end, then follow-up is mandatory11
TreatmentThe management of RCEV is challenging because the use of corticosteroids is effective, but recurrence is common after tapering of full doses.4 Therapy with 0.5mg/kg/day of oral prednisone can be initiated, with tapering of doses at 2 weeks to the minimum necessary to maintain remission.2 Some authors have proposed Indomethacin,8 Tacrolimus,12 and Sutaplast Tosilate,13 for the RCEV maintenance treatment (Table 2).8,13 Nevertheless, dapsone has been shown to be effective in the control of similar conditions such as eosinophilic cellulitis, eosinophilic fasciitis, etc.6 We propose the use of dapsone as a long-term alternative treatment after tapering of corticosteroids when recurrence occurs.
ConclusionRCEV is a infra-diagnosed condition recently described and characterized by pruritic, erythematous, purpuric plaques with fibrinoid necrosis and infiltration of eosinophils in histology. We described four cases and those published in the literature; we propose diagnostic criteria for this disease, and suggest dapsone as a long-term maintenance drug.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Dr. Quijano and Dr. Rodriguez have contributed equally to the work.
Please cite this article as: Quijano-Gomero EG, Rodríguez-Zúñiga MJM, Sanz-Montero ME, Durand-Buse D. Características clínicas, dermatoscópicas e histológicas de varios casos de vasculitis eosinofílica recurrente cutánea. Actas Dermosifiliogr. 2019;110:590–596.