There are 2 stages to the diagnosis and surgical treatment of melanoma. First a biopsy is performed to obtain histological confirmation of the diagnosis; this may be a punch or shave biopsy or an excisional biopsy with a narrow margin of 1–2mm. The definitive surgical approach will depend on the histological findings. Surgical excision of a previously biopsied and confirmed melanoma is performed via re-excision with surgical margins of 0.5–2cm, depending on the Breslow thickness.1 For many authors, however, partial biopsies are not recommended in melanoma patients because of the higher risk of misdiagnosis.2
The high incidence of invasive disease in lesions initially diagnosed as melanoma in situ has been widely reported, demonstrating that biopsy specimens represent only a part of the total tumor and often underestimate the true Breslow thickness of the overall lesion.3
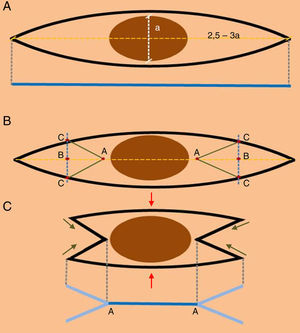
Most excisional biopsies for suspected melanoma are performed using an elliptical incision with narrow margins and primary closure of the defect. The standard ellipse is designed with a long axis 2.5–3 times the length of the outer border of the proposed surgical margin (Fig. 1A). This practice ultimately leads to larger wounds that are more complex to reconstruct and have a higher risk of surgical morbidity, as well as leaving a relatively long scar.
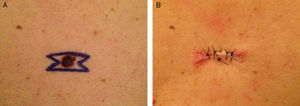
(A) The design of an elliptical excision. The blue line indicates the length of the surgical scar after closure. (B) Design of the double M-plasty. (C) Excision of the double M-plasty (the red arrows indicate closure of the central area, green arrows indicate the closure of the ends of the scar, and the blue line A-A indicates the exact site where the suspicious lesion was located).
Although the current standard practice of wide local excision for melanoma treatment should not be compromised, the situation would be optimized if morbidity and scaring could be reduced while maintaining the same standards applied for wide local excision. To this end, when the diagnosis of a clinically suspected melanoma requires excisional biopsy, we propose a double M-plasty technique (Fig. 1B).4
To design a double M-plasty, we first draw the ellipse described above. Points “A” on the main axis are placed 1mm from the border of the melanoma, and points “B” are situated at the midpoint of the section between point “A” and the apex of the ellipse. Lines perpendicular to the long axis are then drawn through each point “B”; these lines will give 4 points “C” at the intersections of the perpendiculars with the outline of the ellipse, allowing 4 line segments “AC” to be drawn, thus defining the double M-plasty.
This technique has the advantage of leaving a scar that shows exactly where the melanoma was located prior to removal (Fig. 1C, segment “AA”), which will enable us to measure the subsequent surgical margin with much greater accuracy in the definitive excision and thus minimize the need to excise excessive tissue. For example, for a melanoma with a diameter of 8mm, the length of segment AA would be 1cm instead of 2.5-3.6cm. As the surface area of an ellipse is directly proportional to the radius, the area of skin removed using the double M-plasty technique would be 2–3 times smaller than with a conventional elliptic excisional biopsy, though the standard surgical margins recommended for a given Breslow thickness would still be satisfied. In addition, the remaining surgical wound of the double M-plasty would be much simpler to close, with a lower morbidity and a better cosmetic outcome as the scar is shorter and less visible (Fig. 2). Not only does this technique leave a clear indication of the site of the tumor for the definitive surgical excision, but it also has the advantages of tissue conservation and scar length shortening, which have been widely discussed in the literature.5,6
In summary, the double M-plasty is applied as a modification of the traditional elliptical excision. This modification is widely used for the resection of benign and malignant lesions, especially those in areas adjacent to critical structures such as the eyebrow, the vermillion border of the lip, or the chin skin crease. The double M-plasty is generally used to make direct closure of a wound possible with lower tension and a shorter scar length, in addition to avoiding crossing multiple cosmetic units within the repair. When performing an excisional biopsy for a suspected melanoma, the double M-plasty has the additional advantage of identifying the exact site of the primary lesion, which will give us greater control over the width of the surgical margins. In our experience, this has resulted in greater sparing of healthy tissue, less disruption of lymph drainage, and a lower overall morbidity.
Conflict of interestAuthors declare no conflict of interest.