The term fistula is defined as an abnormal or surgically made passage between a hollow or tubular organ and the body surface, or between 2 hollow or tubular organs. A perianal fistula connects the anal canal and the skin of the perineum. The fistulas may follow different paths through the structures of this anatomical region and can be classified, according to Parks, as intersphincteric, trans-sphincteric, suprasphincteric, and extrasphincteric fistulas. Moreover, some authors identify a fifth group of fistulas called superficial fistulas, which run from the lower end of the anal canal to the skin of the perineum.1,2
Perianal fistulas are more common in men, with peak incidence between the third and fifth decades of life. They manifest in the skin of the perianal region, perineum or buttocks as an orifice or violaceous, indurate, painful nodule that drains serosanguinous matter. They may be primary (primary cryptogenic fistulas) or appear secondary to Crohn disease (CD) or hidradenitis suppurativa (HS).
We report on 2 patients with no history of CD or HS, both with indurate violaceous lesions in the perineal region, which drained serosanguinous matter; the ultrasound study provided the definitive diagnosis and indicated the therapeutic approach.
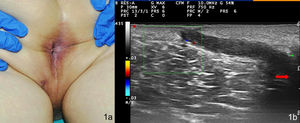
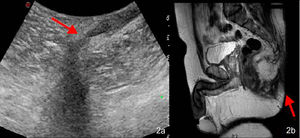
The first case was a 73-year-old man who was referred to our department from general surgery owing to suspected HS. He presented an indurate nodule on the left side of the perineum that was painful on palpation and had appeared a year earlier (Fig. 1A). The patient presented no other skin lesions in the area or in other skin folds and reported no gastrointestinal discomfort. An ultrasound examination was performed using a high-resolution probe (Esaote Mylab Class C, 18MHz), which showed a broad hypoechoic band connecting the skin lesion with the anal canal, with no associated abscesses. Color Doppler mode revealed no vascularization (Fig. 1B). These findings suggested a diagnosis of primary perianal fistula and we requested a perianal transcutaneous ultrasound examination (Fig. 2) and a magnetic resonance imaging study (Fig. 2b); the patient was referred to general surgery for surgical treatment.
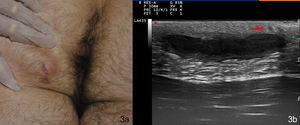
The second patient was a 32-year-old man who was referred to our department from the emergency department to rule out HS. The patient presented an indurate plaque on the left buttock that had appeared 6 months earlier in addition to 2 erosive and exudative nodules (Fig. 3A). The patient presented no other skin lesions in the area or in other skin folds. The ultrasound examination revealed a broad hypoechoic subcutaneous band connecting the visible cutaneous orifice with the skin of the perianal region (Fig. 3B). He also presented associated local thickening of the dermis, dilation of the hair follicles, and a positive color Doppler study of the periphery. In light of the suspected diagnosis of perianal fistula as a form of presentation of HS, we recommended treatment with infiltration of triamcinolone acetonide and follow-up in the dermatology department. A magnetic resonance imaging study confirmed the subcutaneous path of the fistular tract.
Clinical and ultrasound images of the first patient. A,Violaceous nodules with an erosive central region on the left buttock. B,Hypoechoic subcutaneous band corresponding to the fistular path, which connects the visible lesion with the perianal skin. Thickening of the dermis and dilated follicles can also be seen (red arrow).
Primary perianal fistulas originate with an abscess in the anal crypts; their pathogenesis has not been clearly established. They appear in young adults (mostly men) and require no further studies when they present as a single episode. Magnetic resonance imaging is currently the gold-standard examination for diagnosing and classifying these entities, which makes it possible to plan surgical treatment that conserves sphincter function and prevents recurrence.3 Nevertheless, perianal fistulas may also constitute the onset or complication of CD or HS and these diseases should be ruled out in patients who repeatedly present with these fistulas.
Twenty percent of patients with CD present perianal involvement, with complex fistulas that occasionally show branching paths that run through deep anatomical structures from the perineal skin, passing through sphincters to the anal canal, and may form collections of fluid in their path.4,5 Perianal fistulas are highly invalidating and respond poorly to medical treatment.
Involvement of the perianal and gluteal region in HS is not infrequent, particularly in men and in the LC3 phenotype of the Canoui-Poitrine classification.6 According to some studies,7 the disease may be complicated with perianal fistulas in as much as 9% of cases. These are superficial fistulas with single simple paths between the skin of the region and the lower end of the anal orifice, below the pectinate line.4 As well as the path of the fistula, ultrasound will reveal other changes characteristic of HS, such as thickening of the dermis and the subcutaneous cellular tissue, dilated follicles, and hypoechoic collections, which facilitate the diagnosis.8,9 Presence of these fistulas indicates severe HS and a multidisciplinary approach is required, although local medical treatments may be tried prior to surgical excision.10
Recent studies1 suggest that endoanal ultrasound and transcutaneous perianal ultrasound may be the examinations of choice, as they are accessible and minimally invasive techniques that make it possible to accurately determine the path of the fistula. An ultrasound study is essential in patients who present with perianal, perineal or gluteal lesions similar to those we describe; together with the patients’ medical history, this will guide the diagnosis and the appropriate therapeutic approach.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Gómez-Zubiaur A, Alfageme F, Martínez-Lorenzo E, Roustán G. Repercusión diagnóstica y terapéutica del estudio ecográfico en los trayectos fistulosos perianales en pacientes con sospecha de hidradenitis supurativa. Actas Dermosifiliogr. 2018;109:845–847.