Phototesting is a technique that assesses the skin's sensitivity to UV radiation by determining the smallest dose of radiation capable of inducing erythema (minimal erythema dose [MED]) and anomalous responses to UV-A radiation. No phototesting protocol guidelines have been published to date.
MethodologyThis was a multicenter prospective cohort study in which 232 healthy volunteers were recruited at 9 hospitals. Phototests were carried out with solar simulators or fluorescent broadband UV-B lamps. Each individual received a total of 5 or 6 incremental doses of erythemal radiation and 4 doses of UV-A radiation. The results were read at 24hours.
ResultsAt hospitals where solar simulators were used, the mean (SD) MED values were 23 (8), 28 (4), 35 (4), and 51 (6)mJ/cm2 for skin phototypes i to iv, respectively. At hospitals where broadband UV-B lamps were used, these values were 28 (5), 32 (3), and 34 (5)mJ/cm2 for phototypes ii to iv, respectively. MED values lower than 7, 19, 27, and 38mJ/cm2 obtained with solar simulators were considered to indicate a pathologic response for phototypes i to iv, respectively. MED values lower than 18, 24, and 24mJ/cm2 obtained with broadband UV-B lamps were considered to indicate a pathologic response for phototypes ii to iv, respectively. No anomalous responses were observed at UV-A radiation doses of up to 20J/cm2.
ConclusionsResults were homogeneous across centers, making it possible to standardize diagnostic phototesting for the various skin phototypes and establish threshold doses that define anomalous responses to UV radiation.
La técnica del fototest evalúa la sensibilidad de la piel a la radiación ultravioleta (RUV) mediante la determinación de la mínima dosis de radiación capaz de producir eritema (dosis mínima eritemática [DEM]) y la respuesta anómala a UVA. No existen guías protocolizadas para la técnica del fototest.
MetodologíaEstudio multicéntrico de cohortes prospectivo. Un total de 232 voluntarios sanos fueron reclutados en 9 centros hospitalarios. El fototest se realizó con simuladores solares (SS) o lámparas fluorescentes de UVB de banda ancha (UVBBA). Cada sujeto recibió un total de 5 o 6 dosis progresivas de radiación eritemática y 4 dosis de UVA. La lectura se realizó a las 24h.
ResultadosLa DEM media por fototipo fue de 23±8, 28±4, 35±4 y 51±6mJ/cm2 (fototipos i a iv respectivamente) para los centros que utilizaron SS y de 28±5, 32±3 y 34±5mJ/cm2 cuando se utilizaron lámparas de UVBBA para fototipos del ii al iv. Se consideraron valores de DEM patológica 7, 19, 27 y 38mJ/cm2, para los fototipos i al iv respectivamente cuando se emplearon SS y de 18, 24 y 24mJ/cm2 para los fototipos ii-iv expuestos a lámparas de UVBBA. A dosis de hasta 20J/cm2 de UVA no se observaron respuestas anómalas.
ConclusionesExiste homogeneidad de resultados en los diferentes centros participantes, lo que permite estandarizar el método del fotodiagnóstico para los diferentes fototipos cutáneos, así como establecer las dosis umbral que definen una respuesta anómala a la radiación ultravioleta.
Phototesting is used to evaluate the skin's response to light and attempt to establish the spectrum of radiation that will cause adverse reactions or inhibit them.1
A phototesting session can determine a) the minimal erythema dose (MED), which is to say the lowest dose of UV radiation able to cause visible erythema; b) abnormal responses to UV-A light; and c) abnormal responses to visible light. Although phototesting guidelines have recently become available,2 the UV irradiation doses able to induce erythema in healthy individuals and standardized MED doses for testing have not been well established in the literature.3–6 Physicians who undertake phototesting, therefore, may disagree about how to read and interpret the results. For practical purposes, the MED thresholds described by Fitzpatrick7,8 are usually considered reference values for assessing an individual's MED according to phototype.
Lack of homogeneity, both in the use of light sources and dose measurements, between the various members of the Spanish Photobiology Group (GEF) has prevented the development of a common phototesting protocol in the recent past.9
This study's aim was to standardize the phototesting protocol, analyze MED values in a healthy Spanish population by phototype, determine MED threshold values below which an individual could be considered photosensitive, and assess the doses that may trigger abnormal responses to UV-A radiation in this population.
Material and MethodsStudy DesignThis was a multicenter, prospective cohort study.
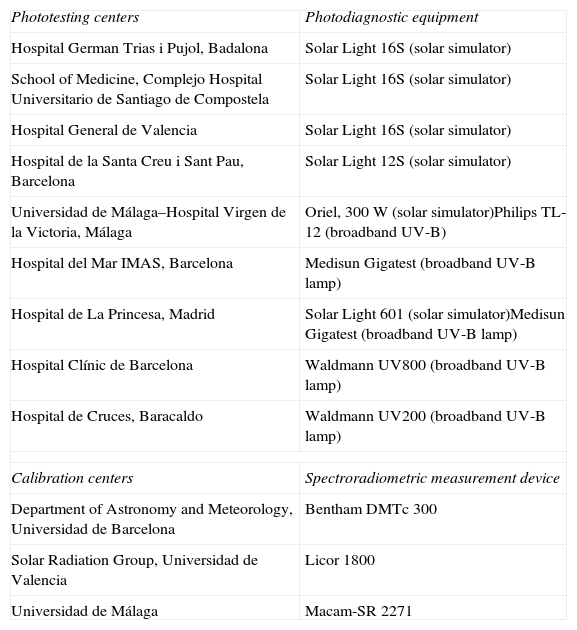
The study was independently reviewed and approved by the ethics committees of the participating hospitals (Table 1) and followed the principles of the Declaration of Helsinki.
Hospitals Participating in the Study and the Equipment Used for Phototesting and Calibration.
| Phototesting centers | Photodiagnostic equipment |
| Hospital German Trias i Pujol, Badalona | Solar Light 16S (solar simulator) |
| School of Medicine, Complejo Hospital Universitario de Santiago de Compostela | Solar Light 16S (solar simulator) |
| Hospital General de Valencia | Solar Light 16S (solar simulator) |
| Hospital de la Santa Creu i Sant Pau, Barcelona | Solar Light 12S (solar simulator) |
| Universidad de Málaga–Hospital Virgen de la Victoria, Málaga | Oriel, 300W (solar simulator)Philips TL-12 (broadband UV-B) |
| Hospital del Mar IMAS, Barcelona | Medisun Gigatest (broadband UV-B lamp) |
| Hospital de La Princesa, Madrid | Solar Light 601 (solar simulator)Medisun Gigatest (broadband UV-B lamp) |
| Hospital Clínic de Barcelona | Waldmann UV800 (broadband UV-B lamp) |
| Hospital de Cruces, Baracaldo | Waldmann UV200 (broadband UV-B lamp) |
| Calibration centers | Spectroradiometric measurement device |
| Department of Astronomy and Meteorology, Universidad de Barcelona | Bentham DMTc 300 |
| Solar Radiation Group, Universidad de Valencia | Licor 1800 |
| Universidad de Málaga | Macam-SR 2271 |
All subjects gave their written informed consent before enrollment.
PopulationVolunteers were recruited in the general dermatology clinics of the participating hospitals. The participants had Fitzpatrick skin phototypes from I to IV and were over the age of 18 years. The exclusion criteria were a history of endogenous or exogenous photosensitivity; current pregnancy or breastfeeding; presence of a skin disease or other condition that might interfere with the performance of the test or the reading of results; having ingested a photosensitizing agent in the 2 months before the phototest, corticosteroids in the last 15 days, or an H1 antihistamine in the last week; and sun exposure in the last 2 months.
Each participant's skin phototype was determined in 2 ways: following the dermatologist's usual practice for assigning a Fitzpatrick classification, and by use of Fitzpatrick's scale, in which genetic and sun exposure aspects are assigned values that can be added together to indicate phototype according to established ranges.10
Light SourcesThe following light sources were used in phototesting: a) solar simulators equipped with xenon arc lamps (the 12S and 16S Solar Light series; Glenside, PA, USA) and the 300-W Oriel Solar Simulator (Newport Corp, Irvine, CA, USA), and b) broadband UV-B (BBUVB) lamps with fluorescent tubes, the most common ones being the Philips TL-12 lamp, the Medisun Gigatest MED Tester (Schulze & Böhm GmbH, Brühl, Germany) and the Waldmann UV 21 (Waldmann GmbH & Co, Villingen-Schwenningen, Germany).
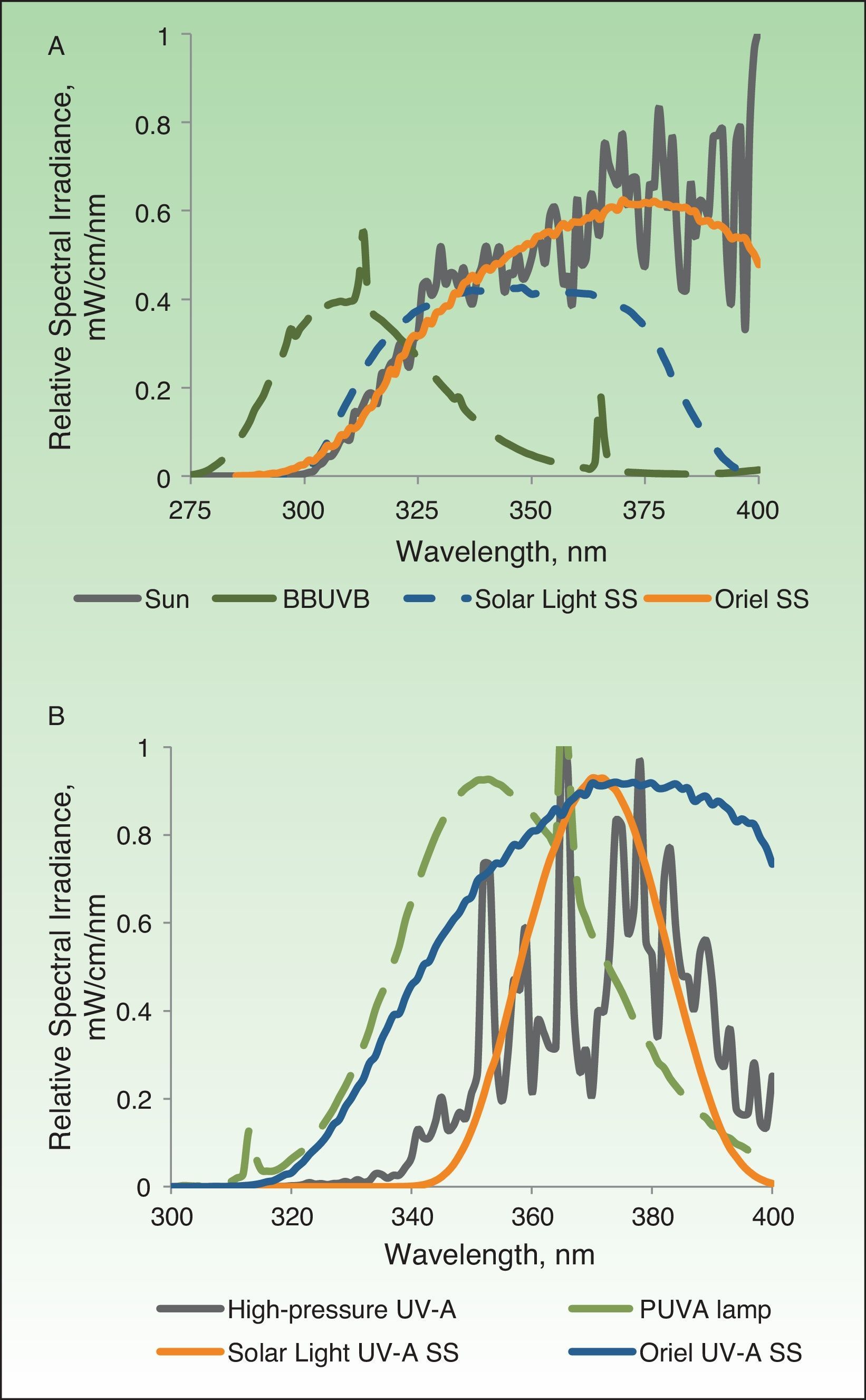
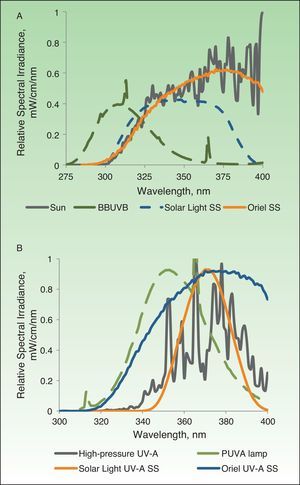
The xenon arc lamps of solar simulators are connected to an energy source and an optical system with dichroic reflectors that allow only UV emissions. With air mass filters (e.g., the AM 1.5 G) they are able to match a solar spectrum between 290 and 400nm (Fig. 1A). These systems are also equipped with external removable filters that can eliminate UV-B wavelengths (below 320nm) to ensure that only UV-A radiation (between 320 and 400nm) reaches the target.
A, Spectra of light emitted by the different sources used in the study shown in comparison with solar light at ground level in the band between 275 and 400nm. B, Spectra of light in the 300–400-nm range emitted by the different UV-A sources studied. BBUVB refers to broadband UV-B; SS, solar simulator; PUVA, psoralen plus UV-A.
The BBUVB lamps are the fluorescent lamps traditionally used in phototherapeutic applications of this type of irradiation. These lamps emit light in wavelengths between 275 and 450nm, with the maximum emission around 310nm; therefore, they are highly erythemogenic. In fact, very short exposure times are used when phototesting with these devices, in spite of their low irradiance. The spectrum of light emitted, however, does not come close to simulating natural sunlight (Fig. 1A).
UV-A devices use 3 types of light source: a) a solar simulator that filters out wavelengths below 320nm, b) UV-A fluorescent lamps (Waldmann UV181 devices with Waldmann lamps developed for psoralen plus UV-A therapy), and c) high-pressure UV-A lamps (Waldmann UVA700 and Philips HB400). The spectra of UV-A radiation emitted by these lamps are shown in Fig. 1B.
Calibration of the Light SourcesBefore phototesting began in this study, the spectral intensity ranges of the light sources used at all the participating centers were measured with a double-monochromator spectroradiometer (MACAM-SR 2271, Macam Photometrics Ltd, Scotland) connected to a flat-field detector with cosine correction. This portable device was itself calibrated with a Bentham DTMc300 double-monochromator spectroradiometer (Bentham Instruments Ltd, Reading, UK), and that device was also periodically calibrated with a 150-W quartz halogen lamp traceable to the UK's National Physical Laboratory. Each light source's spectrum of radiation was recorded and expressed in mW/cm2/nm. As each lamp emitted light over a different spectrum, the irradiance outputs had to be normalized. To that end, the spectral irradiance data were weighted by the erythemal action spectrum of Mackinlay and Diffey,11 established as a reference spectrum by the Commission Internationale de l’Eclairage (CIE). The resulting values of erythemally active irradiance were expressed in mJ/cm2.
For UV-A light sources, emissions were expressed in physical units of radiance (J/cm2) in the range of 320to 400nm.
In addition to these spectroradiometric comparisons, we also calibrated all the radiometers sent by each participating center. In this way the volunteers’ exposure could be adjusted based on radiometric measurements before each phototesting session over the course of the study.
Details of these calibration methods were recently published.1
Phototesting ProtocolThe phototests were performed on skin on the lumbar back or buttocks that had not been sun-exposed. Each exposure site measured at least 1cm in diameter and was located at least 1cm away from the next site.
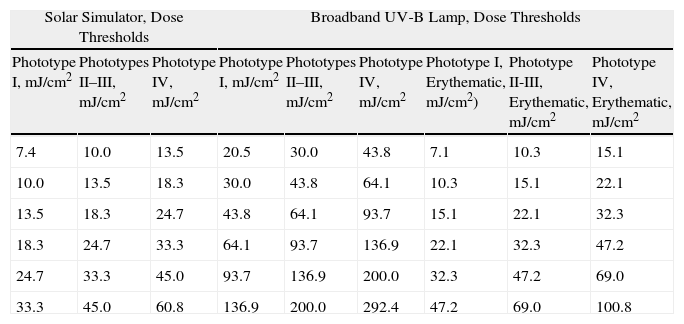
Table 2 shows the threshold doses for each test series for each skin phototype. These values took into consideration the thresholds commonly used at the participating centers. Series of steps were set for use with phototypes II and III and they were then shifted lower for phototype I and higher for phototype IV.
UV Irradiation Dose Steps Used in the Phototesting Series, by Phototype and Light Source.
| Solar Simulator, Dose Thresholds | Broadband UV-B Lamp, Dose Thresholds | |||||||
| Phototype I, mJ/cm2 | Phototypes II–III, mJ/cm2 | Phototype IV, mJ/cm2 | Phototype I, mJ/cm2 | Phototypes II–III, mJ/cm2 | Phototype IV, mJ/cm2 | Phototype I, Erythematic, mJ/cm2) | Phototype II-III, Erythematic, mJ/cm2 | Phototype IV, Erythematic, mJ/cm2 |
| 7.4 | 10.0 | 13.5 | 20.5 | 30.0 | 43.8 | 7.1 | 10.3 | 15.1 |
| 10.0 | 13.5 | 18.3 | 30.0 | 43.8 | 64.1 | 10.3 | 15.1 | 22.1 |
| 13.5 | 18.3 | 24.7 | 43.8 | 64.1 | 93.7 | 15.1 | 22.1 | 32.3 |
| 18.3 | 24.7 | 33.3 | 64.1 | 93.7 | 136.9 | 22.1 | 32.3 | 47.2 |
| 24.7 | 33.3 | 45.0 | 93.7 | 136.9 | 200.0 | 32.3 | 47.2 | 69.0 |
| 33.3 | 45.0 | 60.8 | 136.9 | 200.0 | 292.4 | 47.2 | 69.0 | 100.8 |
In an effort to follow the manner usually used in the literature for expressing radiation exposure, we used biologically effective erythema doses for the series of exposures to solar simulators; absolute, or physical, units were used for exposure to broadband UV-B lamps (mJ/cm2 of UV-B light: 280–320nm). The spectral emissions from each light source were measured (from 275–400nm) and irradiance output was weighted by the erythemal factor to calculate the biologically effective erythema dose (similarly to the system used for solar simulators). This was done so that MED values could be expressed comparably as biologically effective erythema doses.
Six exposures of increasing intensity were delivered. When a solar simulator was the light source, the doses progressed geometrically by a factor of 1.35. When BBUVB lamps were used, doses increased by a factor of 1.45 on the basis of the participating centers’ usual selection of thresholds. However, when the source was the Medisun Gigatest BBUVB lamp, only 5 steps were included in the series because of the number of apertures with which the device is fitted; this device adjusts the dose intervals automatically according to the maximum threshold value for the individual's phototype. That threshold is entered manually by the operator.
The results were read 24hours after exposure, and the lowest irradiation level at which erythema was noticed on an exposed surface was considered the positive reading.12
An abnormal response to UV-A light was detected by exposing 4 sites to increasing doses of 5, 10, 15, and 20J/cm2 (physical units).
Statistical AnalysisMean (SD) values were calculated for each phototype and participating center. We also calculated mean MEDs for the whole population, grouped by center and phototype. A MED was considered abnormal (pathologic) if it was more than 2 SDs below the mean (95% probability of not finding a pathologic MED within that range).
The t test for 2 independent samples was used to test for significant differences. One-way analysis of variance (ANOVA) followed by a multirange Tukey's b test was used to evaluate the significance of differences in mean MED values between centers. Differences were considered significant at a level of P<.05.13
ResultsNine hospitals participated. Four of them used solar simulators (Solar Light S12 or S16), 3 used BBUVB lamps, and 2 used both types of light source (Table 1). The 9 centers recruited 232 volunteers in total.
Most volunteers were women (69%). There were no statistically significant differences (P>.05) in mean age between the sexes (women, 37.9 [14.3] years, range 21–76 years; men, 37.4 [13.8] years, range 21–74 years).
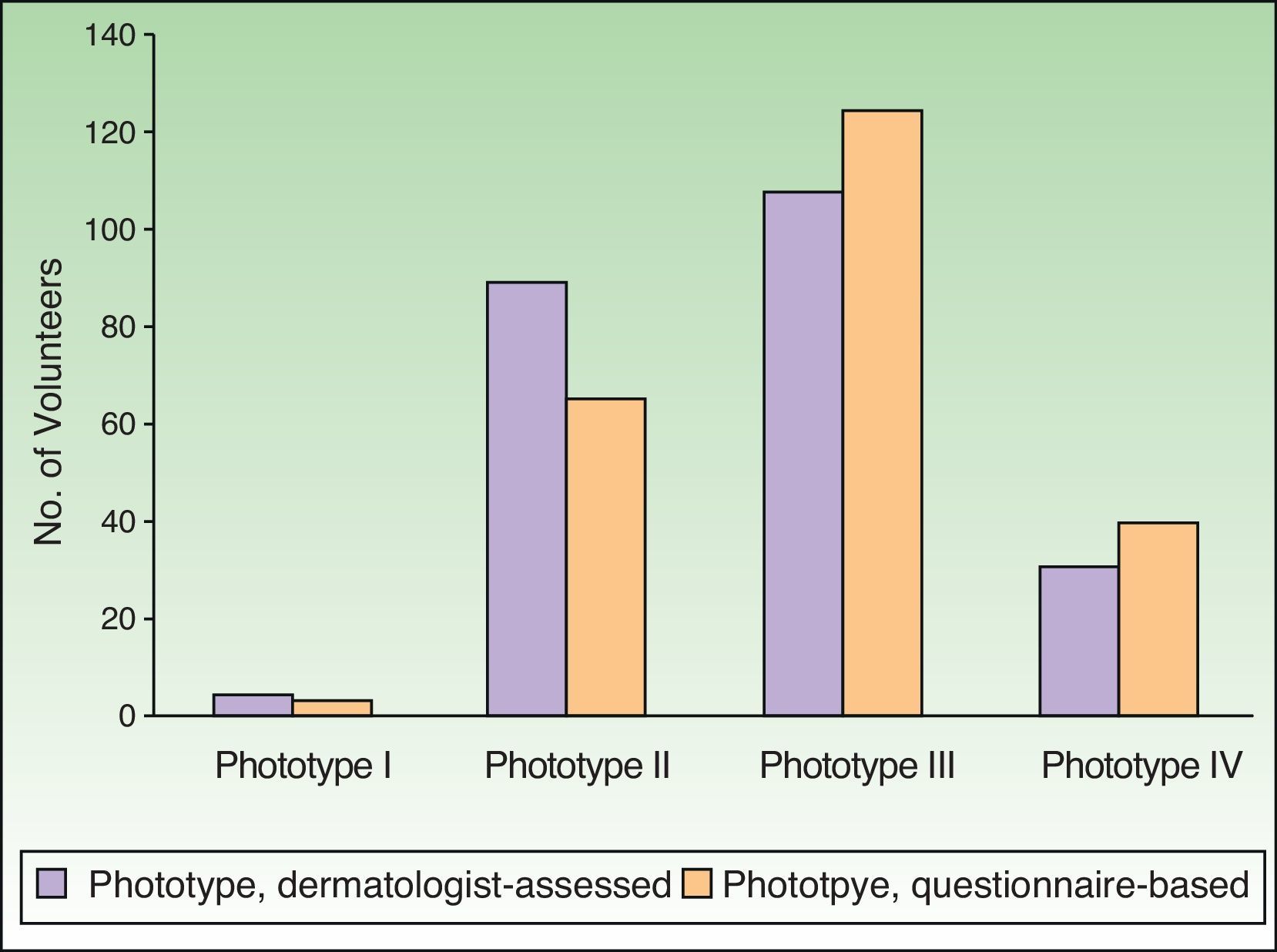
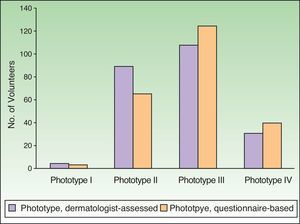
Phototypes assigned by dermatologists using their usual system were mostly II and III (89 and 108 volunteers, respectively) (Fig. 2). The dermatologists classified 4 volunteers as phototype I and 31 as phototype IV. The classifications based on self-reporting (questionnaire) were distributed as follows: I, 3 volunteers; II, 65; III, 124; and IV, 40. When phototype was based on self-assessment, fewer were assigned to phototype II and more to phototypes III and IV.
The dermatologist-assigned phototypes were the ones used to guide choice of a MED test series.
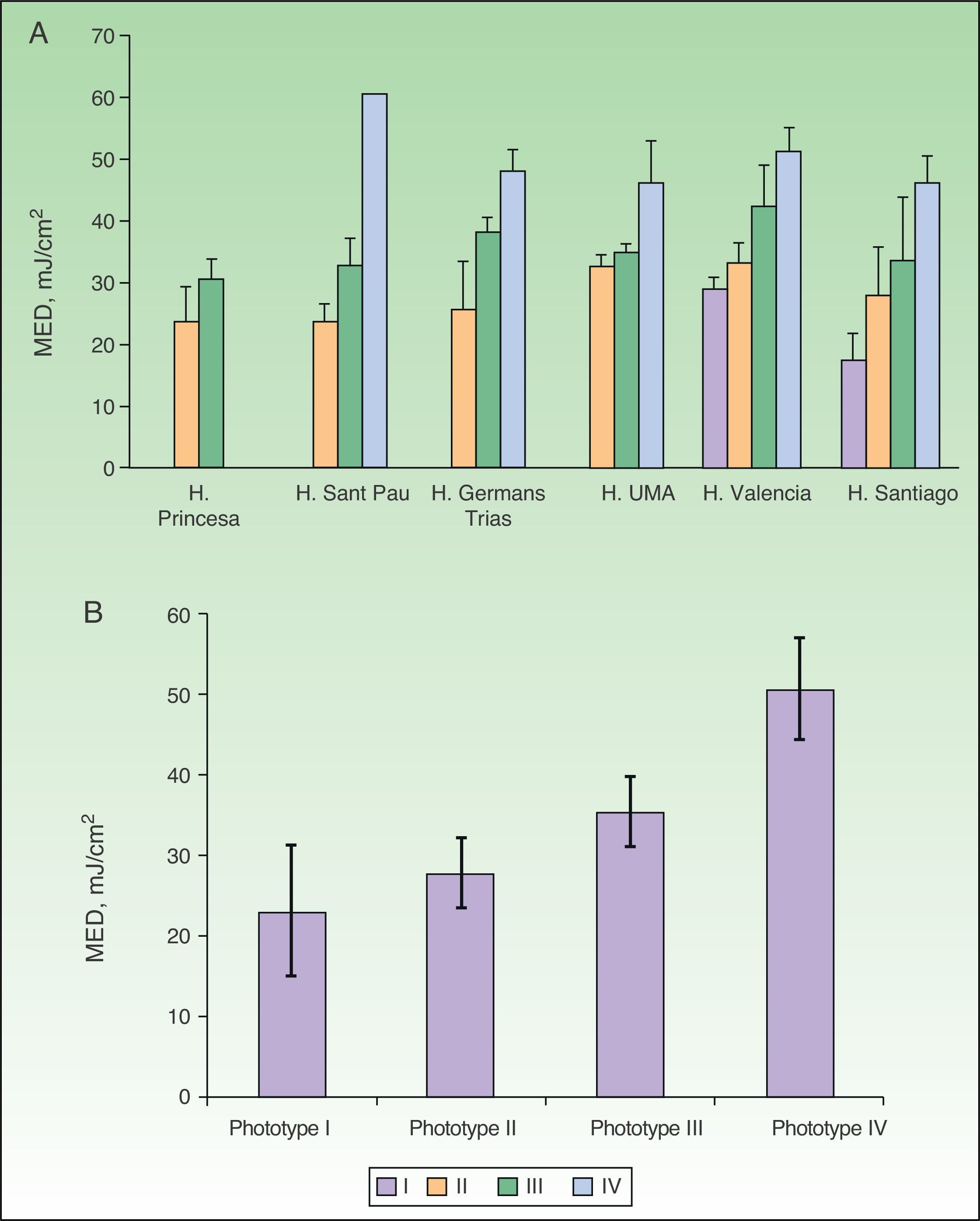
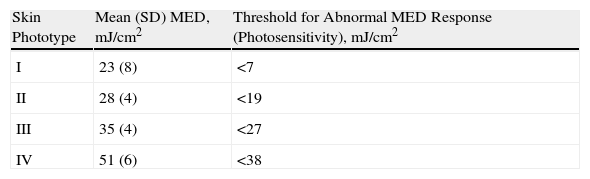
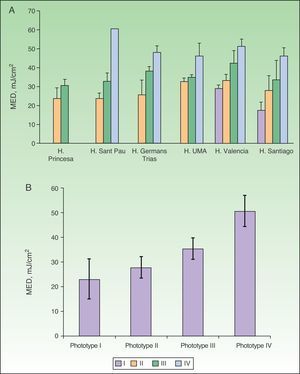
Figure 3A shows mean MEDs for each phototype as recorded at centers using solar simulators. MED increased significantly with phototype at all centers (P<.05, one-way ANOVA). No between-center differences were found on comparing the mean MED findings for phototypes II or III (P>.05, one-way ANOVA; MEDs for phototype II, 28[4] and for phototype III, 35 [4]mJ/cm2; Table 3). The MEDs for phototype IV were very similar in all centers (mean, 51 [6]mJ/cm2) although a higher value was seen in a center that recruited a single volunteer with this phototype. For phototype I, the MEDs were significantly different (P<.05) between the 2 centers that tested phototype-I volunteers; the mean MED was 23(8)mJ/cm2.
A, Adjusted MED by center. B, Adjusted mean MED by phototype when solar simulators were used for phototesting. MED refers to minimal erythema dose; H, hospital; UMA, Universidad de Málaga. Complete hospital names are given in Table 1.
Overall Mean MEDs, Reflecting Data From All Centers Testing With Solar Stimulators, and the Thresholds Indicating Photosensitivity for Each Phototype.
| Skin Phototype | Mean (SD) MED, mJ/cm2 | Threshold for Abnormal MED Response (Photosensitivity), mJ/cm2 |
| I | 23 (8) | <7 |
| II | 28 (4) | <19 |
| III | 35 (4) | <27 |
| IV | 51 (6) | <38 |
Abbreviation: MED, minimal erythema dose.
The average MED values are shown in Table 3 and displayed graphically in Fig. 3B by phototype for all the hospitals that used solar simulators. The MED thresholds below which positivity was considered to indicate photosensitivity are also included. The mean MED values were significantly different between phototypes (P<.05, one-way ANOVA), and there was a positive correlation between mean MED and phototype.
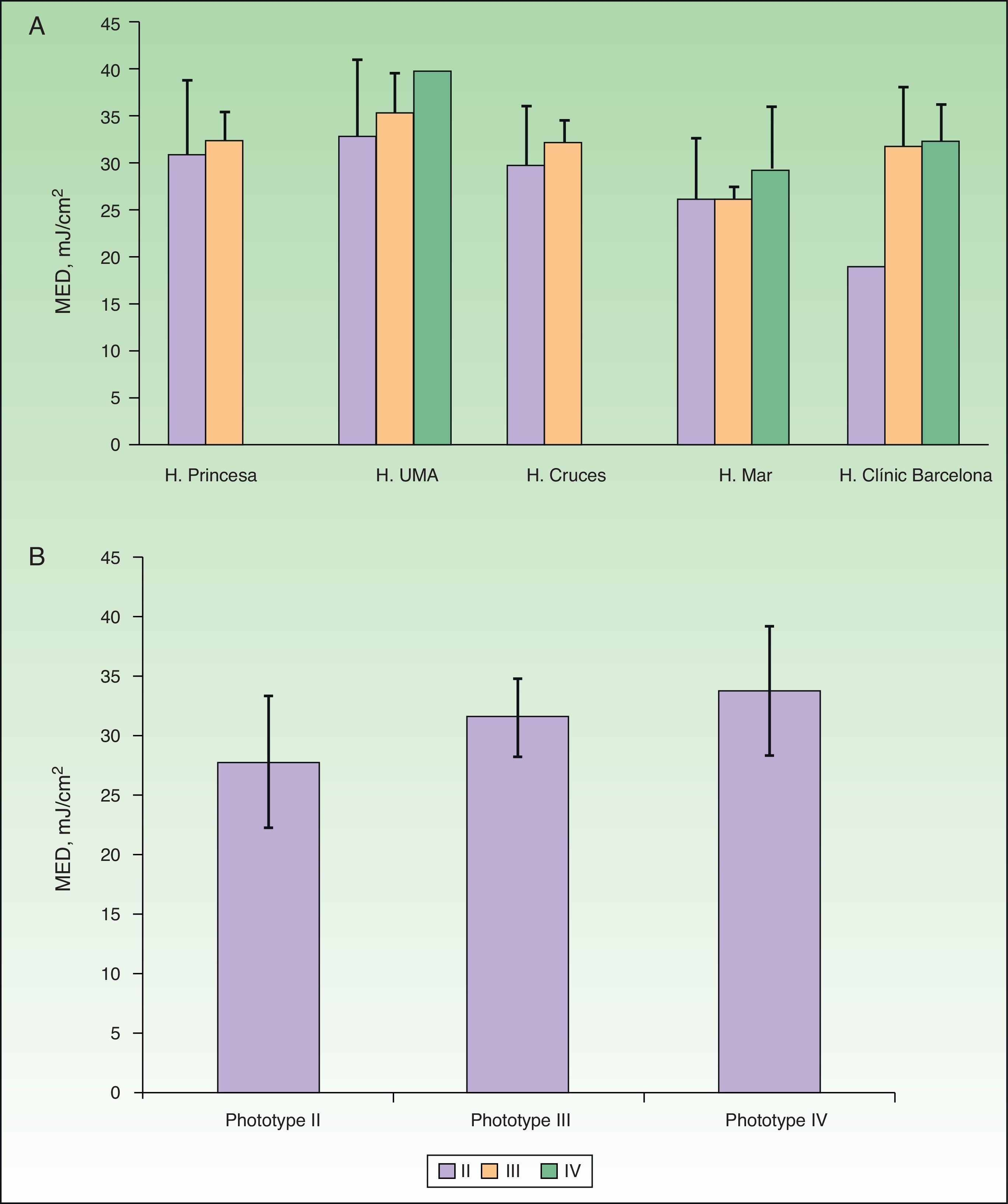
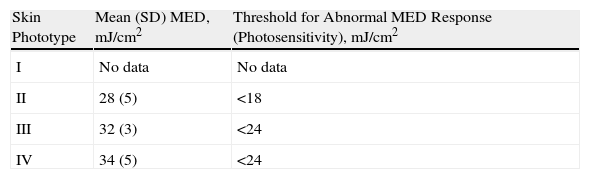
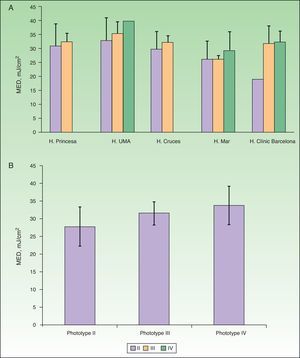
No between-center differences were found on comparing the mean findings of BBUVB phototesting for phototypes II or III (P>.05, one-way ANOVA), but for phototype IV, 1 center had significantly higher MED values (P<.05, one-way ANOVA) (Fig. 4A).
A, Adjusted mean minimal erythema dose (MED) by center. B, Adjusted mean MED by phototype when broadband UV-B lamps were used for phototesting. MED refers to minimal erythema dose; H, hospital; UMA, Universidad de Málaga. Complete hospital names are given in Table 1.
The mean MED values by phototype for all the hospitals that tested with BBUVB lamps are shown in Table 4 and displayed graphically in Fig. 4B. The MED thresholds indicating photosensitivity in BBUVB phototesting are also included. No statistically significant differences in mean MED values or photosensitivity thresholds were found between phototypes II and III.
Overall Mean MEDs, Reflecting Data From All Centers Testing With BBUVB Lamps, and the Thresholds Indicating Photosensitivity for Each Phototype.
| Skin Phototype | Mean (SD) MED, mJ/cm2 | Threshold for Abnormal MED Response (Photosensitivity), mJ/cm2 |
| I | No data | No data |
| II | 28 (5) | <18 |
| III | 32 (3) | <24 |
| IV | 34 (5) | <24 |
Abbreviations: MED, minimal erythema dose; BBUVB, broadband UV-B light.
None of the volunteers in the study displayed abnormal reactions to UV-A exposure.
DiscussionThe phototesting protocol in this study could be followed regardless of whether a hospital uses a solar simulator or a BBUVB lamp as the light source. As a result, we are able to propose phototype-appropriate irradiation ranges that have been validated in different centers. The data can also be used to establish the MED values that, if positive, should be interpreted as an abnormal erythema response for each phototype.
One of the strengths of this study is that we took an important aspect—calibration—into consideration in the first phase. We compared and calibrated the equipment used in the different participating centers, following a suggestion made some years ago.14 The participating centers’ equipment was grouped into 2 categories in this study, even though the devices within each category differed by manufacturer and model. Xenon arc lamps (solar simulators) comprised one group and fluorescent lamps (emitting BBUVB light) comprised the other. Although the devices have evident spectral differences, both these UV light sources have been widely used in many studies and are accepted by the European dermatology forum.2,15
Spectral analyses of all the light sources used for calibration facilitated the normalization of values in the test series. By weighting each light source's emissions with values for the erythemal action spectrum adopted as a reference by the CIE,11 we were able to normalize incremental doses of exposure in terms of irradiance. Because measurements were normalized, phototests with solar simulators and BBUVB devices could be compared, even though the solar simulators used different dose intervals.
The dose thresholds at the upper and lower limits of the test series were defined for each phototype, and 6 geometrically increasing dose steps were set, as in protocols used in other studies.16,17 This 6-step approach, with upper and lower limits set according to phototype, favors the central MED values and increases the likelihood of accurately detecting photosensitivity (by an abnormally low MED). By focusing the series on the central MED thresholds, the 2 highest points are generally positive for erythema and the individual's MED usually falls between the third and fourth step, as the 2 lowest steps do not usually produce erythema in normal skin. The threshold dose for indicating photosensitivity would be found between these 2 lower points.
In the second phase of the study the volunteers were tested in all the participating centers using the study protocol; no field work of this type had ever been undertaken prior to this study.
Most volunteers had phototype II (28.1%) or III (53.3%) skin, and their results were highly similar in all the centers. Volunteers with phototype I skin made up less than 2% of the study population, while 17.1% had phototype IV skin. No previously published data are available to indicate the prevalence of these phototypes in the Spanish population, but these frequencies are clearly valid for the population studied. Given the similarity of phototype distributions and MED values recorded in centers in different geographic locations within Spain, we can probably conclude that the data are representative of the entire Spanish population, although they might well differ considerably from data for populations outside Spain.3,4
Phototype assessment criteria are far from objective. We therefore applied 2 different methods for classifying volunteers by phototype. One was the dermatologist's usual method. The other was the self-report questionnaire leading to classification on the Fitzpatrick scale. Classifications were consistent between the 2 methods for phototypes II and III, although the responses to the questionnaire tended to suggest a slightly higher classification. This difference shows that phototype may be open to question when indicating a phototesting protocol to follow or a therapy to apply.
MED values varied greatly for individuals with the same phototype classification, consistent with many other reports in the literature3–5 and possibly attributable to a variety of factors, such as subjectivity in reading the response or the influence of ambient light. Other confounding factors might be the choice of different anatomical sites for testing and the history of recent sun exposure, but these are sources of bias we tried to minimize when designing the present study.
The results for volunteers tested with solar simulators were very similar to the MEDs established by Fitzpatrick for phototypes I through IV. However, while subjects tested with BBUVB lamps also had mean MED findings within the same ranges, their values differed less markedly between phototypes. It is noteworthy that very similar MEDs were recorded for individuals classified within phototypes III and IV who were tested with BBUVB lamps, suggesting that solar simulator MED testing is more sensitive to change of phototype, probably attributable to the size of dose increases between steps in the series. Larger intervals between steps will lead to lower sensitivity for establishing an individual's MED, and in fact the difference between the lower and upper threshold doses in the BBUVB protocol are larger, as shown in Table 2.
Variability in MED results within the same phototype must lead us to reflect seriously when trying to objectively assess clinical phototest findings. The first question is whether a MED reading bears a clear relationship to phototype. Phototesting gives a result that is said to be measurable and reproducible, but phototype classification itself is based on questions posed by the dermatologist to a healthy subject or a patient, or on self-reporting by the individual; hence it is subject to a higher index of subjectivity and error. We found a lack of correspondence between certain dose intervals and phototype in MED testing. Stated in other words, the MED values found for different phototypes overlapped, consistent with observations from an earlier study.5 The lack of correspondence may be attributable to accumulated error in the assignment of phototype (because of subjectivity and reliance on questionnaires). Alternatively, the cause may simply be that the dose at which erythema develops in response to UV-B radiation, which is tested objectively, is unrelated to the factors used to assess phototype. Nonetheless, the mean values for pooled data from all the centers showed a clear relationship to phototype assignment by the dermatologists, and there was little overlap in our population, in which data showed little dispersion.
A second goal of phototesting is that it identify a photosensitive subject whose MED is abnormally low in cases in which we do not already know what that individual's MED would have been under normal circumstances. In fact, the literature does not establish MED thresholds below which photosensitivity can be diagnosed. It must also be remembered that a large percentage of individuals with photodermatoses (nearly 70% in some series) have phototest results interpreted as normal.18 One of the most important aspects of the present study, therefore, is our proposal for erythemal threshold values below which an observed MED would indicate photosensitivity within a 95% CI; in other words, the probability of observing an abnormal response within the range of normal values would be less than 5% if this test protocol is followed. Although the small number of volunteers with phototypes I and IV in this study might be considered problematic, the consistency of results from all the different centers (Fig. 3B) argues against this being a limitation. In any case, the real clinical application of the values in the test series we propose (Tables 3 and 4) will tell us if these data are in fact reliable.
Finally, none of the volunteers we tested had an abnormal response to UV-A. This exploratory series therefore seems to have been appropriate and gave results that are consistent with those reported by other authors,18 who set the cutoff for an abnormal response at a level of irradiance of less than 20J/cm2.
In conclusion, this study used normalized units of measurement and effective erythema dose step increases across the different light sources used by the participating centers. The results recorded at the centers were pooled to give standardized MED values according to phototypes that were consistent with those of Fitzpatrick. We also proposed a MED threshold indicative of pathologic response for each phototype, defining phototesting series for detecting abnormal reactions to UV-A irradiation. Finally, we note the need for further study to improve the testing series used for BBUVB lamps in order to increase the sensitivity of MED measurements between phototypes.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that the procedures followed adhered to the ethical guidelines of the responsible committee on human experimentation and comply with the Declaration of Helsinki of the World Medical Association.
Data confidentialityThe authors declare that they have followed the protocols of their hospitals concerning the publication of patient data and that all the patients included in this study were appropriately informed and gave their written informed consent.
Right to privacy and informed consentThe authors declare that no private patient data appear in this article.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
The authors wish to express their gratitude to all the persons who directly or indirectly contributed to this study. In particular, we thank S. Gómez-Bernal, of Hospital Universitario Central de Asturias in Oviedo; and Ramón García, medical resident, and Concepción Sierra, nurse, both at the Dermatology Department, Hospital General Universitario de Valencia.
Please cite this article as: Pérez Ferriols A, Aguilera J, Aguilera P, de Argila D, Barnadas MA, de Cabo X, et al. Determinación de la dosis eritemática mínima y reacciones anómalas a radiación ultravioleta A según fototipo. Actas Dermosifiliogr. 2014;105:780–788.