A perceived risk of cancer encourages preventive behavior while the lack of such a perception is a barrier to risk reduction. There are no instruments in Spanish to measure this perceived risk and thus quantify response to interventions for preventing this disease at a population level. The aim of this study was to design and validate a self-administered questionnaire for measuring the perceived risk of skin cancer.
Material and methodsA self-administered questionnaire with a visual Likert-type scale was designed based on the results of the analysis of the content of a survey performed in 100 patients in the Dr. Ladislao de la Pascua Skin Clinic, Distrito Federal México, Mexico. Subsequently, the questionnaire was administered to a sample of 359 adult patients who attended the clinic for the first time. As no gold standard exists for measuring the perceived risk of skin cancer, the construct was validated through factor analysis.
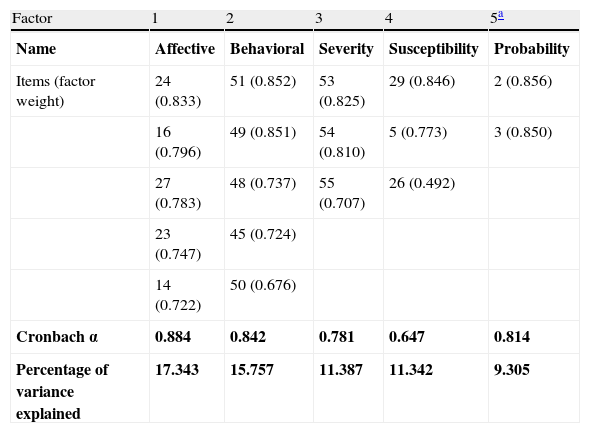
ResultsThe final questionnaire had 18 items. The internal consistency measured with Cronbach α was 0.824 overall. In the factor analysis, 4 factors (denoted as affective, behavioral, severity, and susceptibility) and an indicator of risk accounted for 65.133% of the variance.
ConclusionsThe psychometric properties of the scale were appropriate for measuring the perception of risk in adult patients (aged 18 years or more) who attended the dermatology clinic.
El riesgo percibido en cáncer predice un comportamiento preventivo, y la falta de este es una barrera para la reducción del riesgo. No existe un instrumento en idioma español que mida la percepción de riesgo de cáncer de piel que sirva como medida de respuesta en intervenciones para prevenir esta enfermedad a nivel poblacional. El objetivo de este trabajo fue elaborar y validar un cuestionario autoadministrado para medir percepción de riesgo de cáncer de piel.
Material y métodosSe elaboró un cuestionario autoadministrado con escala de respuesta tipo Likert pictórico en función de los resultados del análisis de contenido de una encuesta realizada a 100 pacientes del Centro Dermatológico Dr. Ladislao de la Pascua. Posteriormente se aplicó el cuestionario a una muestra de 359 pacientes adultos que acudían por primera vez a dicho centro dermatológico. Al no existir un estándar de oro para medir percepción de riesgo de cáncer de piel se realizó la validación de constructo mediante análisis factorial.
ResultadosEl cuestionario final tiene 18 ítems, su consistencia interna medida por el alfa de Cronbach fue de 0,824 global. El análisis factorial mostró 4 factores que explicaron el 65,133% de la varianza, los cuales se denominaron: afectivo, conductual, gravedad, susceptibilidad y un indicador de probabilidad.
ConclusionesLas propiedades psicométricas de la escala son adecuadas para medir la percepción de riesgo en personas adultas con una edad igual o mayor a 18 años usuarias de los servicios de salud en el área de dermatología.
The incidence of skin cancer is increasing throughout the world, making this disease the most common malignant neoplasm in Mexico.1 Basal cell carcinoma is the most frequent type (74%), followed by squamous cell carcinoma (14%), and melanoma (3%).2 The risk factors for skin cancer are chronic or intermittent sun exposure,3 history of sunburn,4 use of tanning beds,5 >15 melanocytic nevi,6 family and personal history of skin cancer, phototype (light-colored eyes and fair skin and hair),7 previous radiotherapy8 and phototherapy,9 immunosuppression associated with organ transplantation,10 and exposure to carcinogens such as arsenic (contaminated water).11
Skin cancer can be prevented by means of behavioral measures, such as avoiding sun exposure and using sunscreen, which are associated with an individual's perception of the risk of skin cancer. A perceived risk of cancer encourages preventive behavior, while the lack of such a perception is a barrier to risk reduction. It is well known that information cannot produce an expected effect on behavioral change, and that an individual's motivation to change his/her behavior is affected by social and psychological variables. The model developed by Jackson and Aiken to investigate the intention to protect oneself from the sun and to sunbathe brings together the theory of planned behavior,12 the health belief model,13 and the protection motivation theory.14,15 In the model, behavior associated with sun exposure is the result of 4 psychological variables: health beliefs, self-efficacy with respect to sun protection, attitudes toward sunbathing, and norms for protection and sunbathing. The intention of protecting oneself from the sun arises from an individual's perception of the risk of skin cancer, that is, those who feel threatened by or believe themselves prone to skin cancer will have the intention to protect themselves from the sun and avoid exposure to it.
According to Brewer et al,16 the perception of risk is a construct comprising 3 dimensions associated with the damage caused if measures are not taken to prevent it. The 3 dimensions are probability of damage, constitutional susceptibility or vulnerability, and severity or degree of damage. The perception of the risk of skin cancer is the impression or sensation of threat we feel based on individual severity, probability, and susceptibility, which are the product of the attitudes and beliefs towards the intention to protect oneself from and/or expose oneself to sunlight.17
Several methods have been applied to measure the perceived risk of melanoma and nonmelanoma skin cancer (basal cell and squamous cell carcinoma). The most common method involves measuring risk absolutely and comparatively, that is, by asking individuals to estimate their personal risk and their risk compared with the population in general, respectively. The absolute forms include those associated with and not associated with preventive behavior. They also include cognitive and affective-type measures of perceived risk; the former reflect the probability of having skin cancer based on the objective risk (norms), the latter reflect the purely cognitive component (beliefs). In summary, the dimensions of the construct for perceived risk of skin cancer are as follows: probability, susceptibility, severity, affective dimension, and behavioral dimension.15
No Spanish-language instruments have been developed to measure perceived risk of melanoma and nonmelanoma skin cancer. Some instruments evaluate behavior, attitudes, and knowledge associated with sun exposure. However, it is necessary to develop an instrument to measure perception of risk for use in future interventions to modify behavior with respect to sun exposure. The objective of the present work was to design and validate an instrument for measuring perceived risk of skin cancer (basal cell, squamous cell, and melanoma) in Mexicans aged >18 years. The instrument includes all 5 dimensions of the construct and is self-administered. The responses are given on a visual Likert-type scale of 7 options to make it easier to answer.
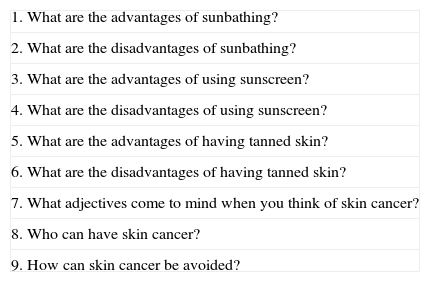
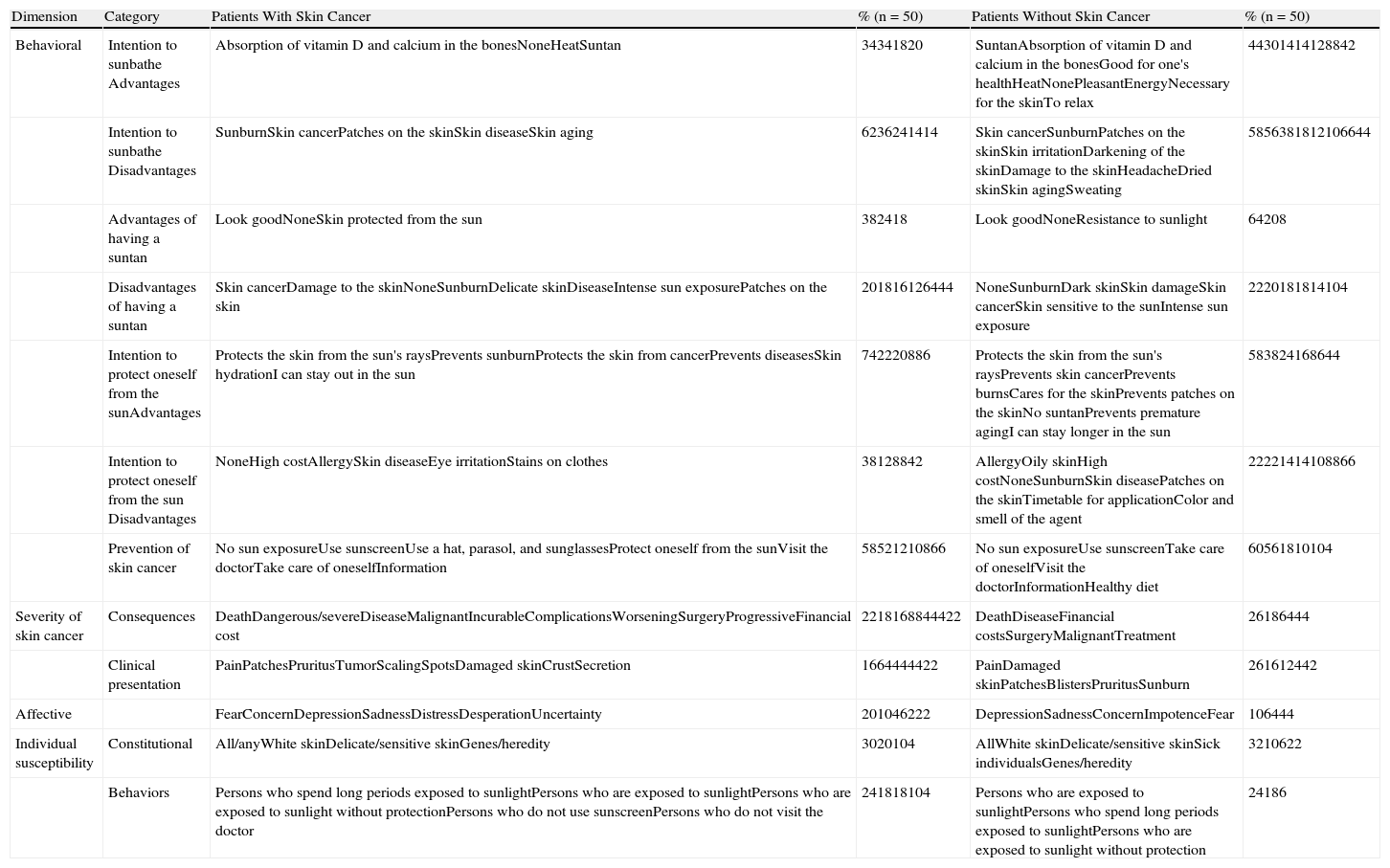
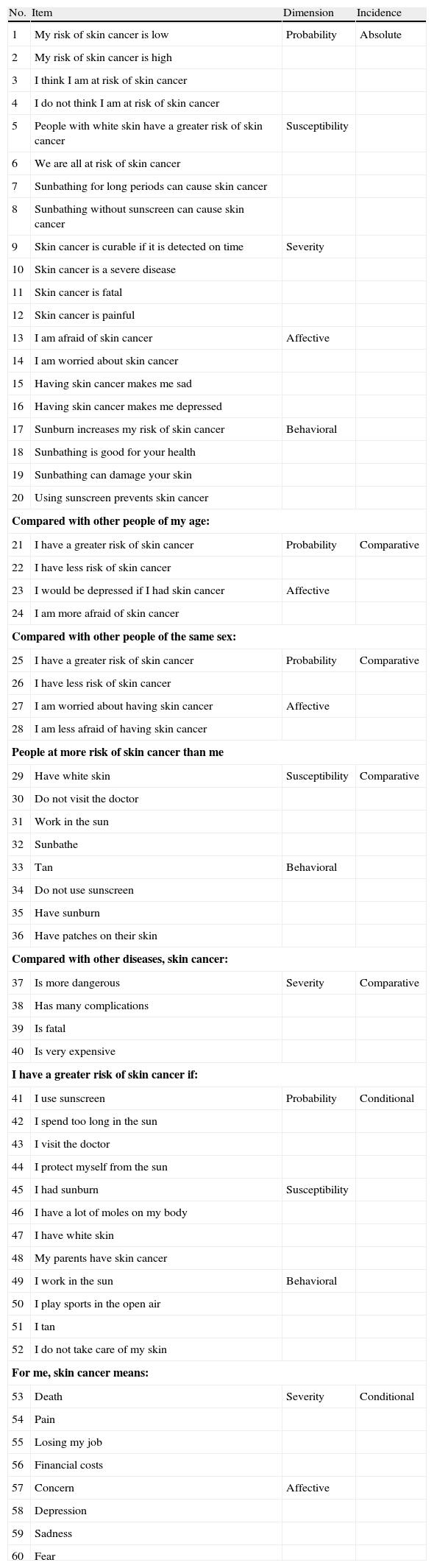
Materials and MethodsDesignThe construct to be measured was perceived risk of skin cancer, which comprises 5 dimensions: probability, susceptibility, severity, affective, and behavioral. The items were prepared using an open-question survey to sample the content and terminology of the construct dimensions. The open questions were chosen based on previous studies and the opinion of the authors with the help of an expert in the design and validation of psychometric instruments. The questions are shown in Table 1. We surveyed 100 patients, 50% of whom had been diagnosed with skin cancer (Group 1) and 50% of whom had not (Group 2). All the patients were from the Dermatology-Oncology Clinic and Outpatient Clinic of Centro Dermatológico Dr. Ladislao de la Pascua. Group 1 included 25 men and 25 women, with a mean age of 59 years (37-92 years). The mean age was 61 years for women and 57 years for men. As for educational level, 52% had completed primary education, 12% secondary education, 19% university preparatory studies, and 17% an undergraduate degree. Group 2 included 25 men and 25 women, with a mean age of 37 years (18-69 years). The mean age was 35 years for women and 40 years for men. As for educational level, 20% had completed primary education, 34% secondary education, 34% university preparatory studies, and 12% an undergraduate degree. The content was analyzed qualitatively and by subject using words or sentences associated with the dimensions of the construct as the unit of analysis under the following categories: intention to sunbathe, intention to protect oneself from the sun, suntan, prevention of skin cancer, consequences, clinical symptoms, affective aspects, and constitutional and behavioral susceptibility. The summary of the content analysis is shown in Table 2. Based on the results of the survey, we drew up a proposal for an instrument based on 60 items distributed in 3 areas of incidence and 5 dimensions. Each dimension had 12 items distributed homogenously in 3 areas of incidence (absolute, comparative, and conditional), that is, 4 for each area. Table 3 shows all the items proposed according to the area of incidence and the corresponding dimension. Each item has 7 possible responses; therefore, the minimum score is 1 and the maximum 7 per item. A score of 1 corresponds to the smallest square on the pictorial Likert-type scale and 7 to the largest square, which lies immediately to the right of the question.
List of Open Questions for Design of the Items.
| 1. What are the advantages of sunbathing? |
| 2. What are the disadvantages of sunbathing? |
| 3. What are the advantages of using sunscreen? |
| 4. What are the disadvantages of using sunscreen? |
| 5. What are the advantages of having tanned skin? |
| 6. What are the disadvantages of having tanned skin? |
| 7. What adjectives come to mind when you think of skin cancer? |
| 8. Who can have skin cancer? |
| 9. How can skin cancer be avoided? |
Content Analysis.
| Dimension | Category | Patients With Skin Cancer | % (n=50) | Patients Without Skin Cancer | % (n=50) |
| Behavioral | Intention to sunbathe Advantages | Absorption of vitamin D and calcium in the bonesNoneHeatSuntan | 34341820 | SuntanAbsorption of vitamin D and calcium in the bonesGood for one's healthHeatNonePleasantEnergyNecessary for the skinTo relax | 44301414128842 |
| Intention to sunbathe Disadvantages | SunburnSkin cancerPatches on the skinSkin diseaseSkin aging | 6236241414 | Skin cancerSunburnPatches on the skinSkin irritationDarkening of the skinDamage to the skinHeadacheDried skinSkin agingSweating | 5856381812106644 | |
| Advantages of having a suntan | Look goodNoneSkin protected from the sun | 382418 | Look goodNoneResistance to sunlight | 64208 | |
| Disadvantages of having a suntan | Skin cancerDamage to the skinNoneSunburnDelicate skinDiseaseIntense sun exposurePatches on the skin | 201816126444 | NoneSunburnDark skinSkin damageSkin cancerSkin sensitive to the sunIntense sun exposure | 2220181814104 | |
| Intention to protect oneself from the sunAdvantages | Protects the skin from the sun's raysPrevents sunburnProtects the skin from cancerPrevents diseasesSkin hydrationI can stay out in the sun | 742220886 | Protects the skin from the sun's raysPrevents skin cancerPrevents burnsCares for the skinPrevents patches on the skinNo suntanPrevents premature agingI can stay longer in the sun | 583824168644 | |
| Intention to protect oneself from the sun Disadvantages | NoneHigh costAllergySkin diseaseEye irritationStains on clothes | 38128842 | AllergyOily skinHigh costNoneSunburnSkin diseasePatches on the skinTimetable for applicationColor and smell of the agent | 22221414108866 | |
| Prevention of skin cancer | No sun exposureUse sunscreenUse a hat, parasol, and sunglassesProtect oneself from the sunVisit the doctorTake care of oneselfInformation | 58521210866 | No sun exposureUse sunscreenTake care of oneselfVisit the doctorInformationHealthy diet | 60561810104 | |
| Severity of skin cancer | Consequences | DeathDangerous/severeDiseaseMalignantIncurableComplicationsWorseningSurgeryProgressiveFinancial cost | 2218168844422 | DeathDiseaseFinancial costsSurgeryMalignantTreatment | 26186444 |
| Clinical presentation | PainPatchesPruritusTumorScalingSpotsDamaged skinCrustSecretion | 1664444422 | PainDamaged skinPatchesBlistersPruritusSunburn | 261612442 | |
| Affective | FearConcernDepressionSadnessDistressDesperationUncertainty | 201046222 | DepressionSadnessConcernImpotenceFear | 106444 | |
| Individual susceptibility | Constitutional | All/anyWhite skinDelicate/sensitive skinGenes/heredity | 3020104 | AllWhite skinDelicate/sensitive skinSick individualsGenes/heredity | 3210622 |
| Behaviors | Persons who spend long periods exposed to sunlightPersons who are exposed to sunlightPersons who are exposed to sunlight without protectionPersons who do not use sunscreenPersons who do not visit the doctor | 241818104 | Persons who are exposed to sunlightPersons who spend long periods exposed to sunlightPersons who are exposed to sunlight without protection | 24186 |
Proposed Instrument With Classification of Items (n=60).
| No. | Item | Dimension | Incidence |
| 1 | My risk of skin cancer is low | Probability | Absolute |
| 2 | My risk of skin cancer is high | ||
| 3 | I think I am at risk of skin cancer | ||
| 4 | I do not think I am at risk of skin cancer | ||
| 5 | People with white skin have a greater risk of skin cancer | Susceptibility | |
| 6 | We are all at risk of skin cancer | ||
| 7 | Sunbathing for long periods can cause skin cancer | ||
| 8 | Sunbathing without sunscreen can cause skin cancer | ||
| 9 | Skin cancer is curable if it is detected on time | Severity | |
| 10 | Skin cancer is a severe disease | ||
| 11 | Skin cancer is fatal | ||
| 12 | Skin cancer is painful | ||
| 13 | I am afraid of skin cancer | Affective | |
| 14 | I am worried about skin cancer | ||
| 15 | Having skin cancer makes me sad | ||
| 16 | Having skin cancer makes me depressed | ||
| 17 | Sunburn increases my risk of skin cancer | Behavioral | |
| 18 | Sunbathing is good for your health | ||
| 19 | Sunbathing can damage your skin | ||
| 20 | Using sunscreen prevents skin cancer | ||
| Compared with other people of my age: | |||
| 21 | I have a greater risk of skin cancer | Probability | Comparative |
| 22 | I have less risk of skin cancer | ||
| 23 | I would be depressed if I had skin cancer | Affective | |
| 24 | I am more afraid of skin cancer | ||
| Compared with other people of the same sex: | |||
| 25 | I have a greater risk of skin cancer | Probability | Comparative |
| 26 | I have less risk of skin cancer | ||
| 27 | I am worried about having skin cancer | Affective | |
| 28 | I am less afraid of having skin cancer | ||
| People at more risk of skin cancer than me | |||
| 29 | Have white skin | Susceptibility | Comparative |
| 30 | Do not visit the doctor | ||
| 31 | Work in the sun | ||
| 32 | Sunbathe | ||
| 33 | Tan | Behavioral | |
| 34 | Do not use sunscreen | ||
| 35 | Have sunburn | ||
| 36 | Have patches on their skin | ||
| Compared with other diseases, skin cancer: | |||
| 37 | Is more dangerous | Severity | Comparative |
| 38 | Has many complications | ||
| 39 | Is fatal | ||
| 40 | Is very expensive | ||
| I have a greater risk of skin cancer if: | |||
| 41 | I use sunscreen | Probability | Conditional |
| 42 | I spend too long in the sun | ||
| 43 | I visit the doctor | ||
| 44 | I protect myself from the sun | ||
| 45 | I had sunburn | Susceptibility | |
| 46 | I have a lot of moles on my body | ||
| 47 | I have white skin | ||
| 48 | My parents have skin cancer | ||
| 49 | I work in the sun | Behavioral | |
| 50 | I play sports in the open air | ||
| 51 | I tan | ||
| 52 | I do not take care of my skin | ||
| For me, skin cancer means: | |||
| 53 | Death | Severity | Conditional |
| 54 | Pain | ||
| 55 | Losing my job | ||
| 56 | Financial costs | ||
| 57 | Concern | Affective | |
| 58 | Depression | ||
| 59 | Sadness | ||
| 60 | Fear | ||
Since there is no gold standard for measuring perceived risk of skin cancer, the construct was validated. We selected patients who were attending Centro Dermatológico Dr. Ladislao de la Pascua for the first time. All patients were Mexican and aged ≥18 years. They all agreed to participate in the survey and gave their informed consent to do so. The sample size was calculated at 300 patients, considering that 5 patients were necessary for each item in the initial proposal. The patient sample was different from that selected for the design of the instrument. The instrument was administered to the group in the waiting room before the visit with the doctor.
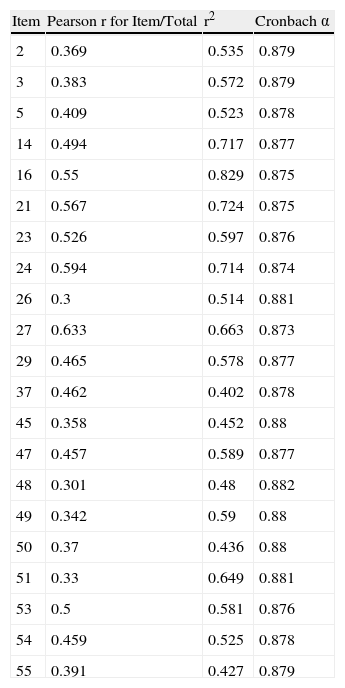
Statistical AnalysisFrequency per item was analyzed to verify whether all the options were selected, and the upper and lower quartiles of each item were compared using the t test to evaluate discrimination. The directionality of the items was evaluated using contingency tables and the χ2 test. Items shown to be discriminatory (P<.05, t test) and to have directionality (P<.05, χ2 test) were analyzed using the Cronbach α to measure internal consistency or reliability. The Pearson correlation between the items was calculated. We then eliminated items with the following characteristics: correlation with the total <0.30, multiple correlation squared <0.40, and high correlation (≥0.8) between items. From the items that showed a high correlation, we chose the one with the best profile according to the characteristics set out above. For the remaining items, we performed factor analysis using the principal component method. We calculated the z values and the percentile ranges to set the norms for standardizing the direct scores of the questionnaire in our study sample.
ResultsThe instrument was administered to 359 patients at the Outpatient Clinic of Centro Dermatológico Dr. Ladislao de la Pascua in March and April 2012. The demographic characteristics of the sample were as follows: 70.2% women and 29.8% men, with a mean (SD) age of 38 (14.4) years. Educational level was primary in 18.4% of cases, secondary in 22%, university preparatory in 34.5%, undergraduate in 22.6%, and postgraduate in 2.5%.
Of the 60 initial items on the questionnaire, replies were provided for each of the 7 options on the pictorial Likert scale. Items 1, 4, and 18 were not discriminatory and were eliminated. Items 6-12, 17, 19-20, 31-36, 38-44, 52, and 56-60 were eliminated owing to lack of directionality. Item 22 was the only one with a correlation with the total <0.30, whereas 28, 30, and 46 had a squared multiple correlation <0.40. A high correlation was recorded between items 14, 16, and 21 and items 13, 15, and 25, respectively, (r=0.803, 0.883, and 0.815). Those with the best profile were selected, and items 13, 15, and 25 were eliminated. Table 4 presents the results for the correlations and the Cronbach α of those items that proved to be discriminatory and have directionality. A total of 39 items were eliminated; the Cronbach α or reliability of the instrument with the 21 items selected was 0.851. The factor analysis with orthogonal rotation was subsequently performed using the principal components method, since the correlations between the items were low to medium. Coefficients <0.40 were excluded. According to the percentage of variance explained and the break in the scree test, 5 real factors were identified. Items 21, 37, and 47 were repeated in more than 1 factor with factor weights >0.40; therefore, they were eliminated. Finally, 18 items remained, and the total Cronbach α was 0.824. Four factors (affective aspects, behavioral aspects, severity, and susceptibility) and an indicator of risk accounted for 65.133% of the variance. Table 5 shows the factors, their items, and the explained variance.
Analysis of Items.
| Item | Pearson r for Item/Total | r2 | Cronbach α |
| 2 | 0.369 | 0.535 | 0.879 |
| 3 | 0.383 | 0.572 | 0.879 |
| 5 | 0.409 | 0.523 | 0.878 |
| 14 | 0.494 | 0.717 | 0.877 |
| 16 | 0.55 | 0.829 | 0.875 |
| 21 | 0.567 | 0.724 | 0.875 |
| 23 | 0.526 | 0.597 | 0.876 |
| 24 | 0.594 | 0.714 | 0.874 |
| 26 | 0.3 | 0.514 | 0.881 |
| 27 | 0.633 | 0.663 | 0.873 |
| 29 | 0.465 | 0.578 | 0.877 |
| 37 | 0.462 | 0.402 | 0.878 |
| 45 | 0.358 | 0.452 | 0.88 |
| 47 | 0.457 | 0.589 | 0.877 |
| 48 | 0.301 | 0.48 | 0.882 |
| 49 | 0.342 | 0.59 | 0.88 |
| 50 | 0.37 | 0.436 | 0.88 |
| 51 | 0.33 | 0.649 | 0.881 |
| 53 | 0.5 | 0.581 | 0.876 |
| 54 | 0.459 | 0.525 | 0.878 |
| 55 | 0.391 | 0.427 | 0.879 |
Factors Used in the Instrument.
| Factor | 1 | 2 | 3 | 4 | 5a |
| Name | Affective | Behavioral | Severity | Susceptibility | Probability |
| Items (factor weight) | 24 (0.833) | 51 (0.852) | 53 (0.825) | 29 (0.846) | 2 (0.856) |
| 16 (0.796) | 49 (0.851) | 54 (0.810) | 5 (0.773) | 3 (0.850) | |
| 27 (0.783) | 48 (0.737) | 55 (0.707) | 26 (0.492) | ||
| 23 (0.747) | 45 (0.724) | ||||
| 14 (0.722) | 50 (0.676) | ||||
| Cronbach α | 0.884 | 0.842 | 0.781 | 0.647 | 0.814 |
| Percentage of variance explained | 17.343 | 15.757 | 11.387 | 11.342 | 9.305 |
Each item has 7 possible options for response, with a minimum score of 1 and a maximum of 7 per question. Since the final questionnaire has 18 items, the minimum score is 18 and the maximum 126.
The linear standard qualification according to the z values showed that the mean (SD) total punctuation of the sample was 83.0529 (19.96225), whereas the median was 81 points with an interquartile range of 28 points. These findings enable us to interpret the results in subsequent applications of the questionnaire by comparing the final score with that obtained by our study sample, from which we obtained the norm for standardization.
The instrument is enclosed as an appendix.
DiscussionThe validated questionnaire enables us to measure the construct perceived risk of skin cancer. No specific instruments have been designed to measure this construct. Perceived risk of skin cancer has been investigated using focus groups and interviews.18 Questionnaires used at population level, such as the Health Information Trends Survey, measure the perceived risk of cancer by posing 3 questions associated with the probability of having skin cancer in the affective dimension.19 Bränström et al.21 measured the perceived risk of skin cancer using 3 questions on individual probability, the incidence of this type of cancer in Sweden, and the probability compared with another individual of the same age. However, the study by Janssen et al.17 compared the different forms of operationalization or design of questions for measuring this construct. The purpose-designed questionnaire comprised 14 and 13 questions from the dimensions of probability and severity, respectively. The results show us that the comparative and conditional questions are better predictors of sun protection behavior. The only available Spanish-language instrument is that of De Troya-Martín et al.,20 which measures knowledge and attitude associated with sun exposure; therefore, we consider that, to date, our questionnaire is the only one designed to measure perceived risk of skin cancer and that, together with the questionnaire of De Troya-Martin et al., it can be used to measure the impact of interventions aimed at preventing melanoma and nonmelanoma skin cancer.
The final version of the questionnaire is short (only 18 items) and easy to complete, since it is based on a pictorial scale. As with most psychometric instruments, it requires a cover sheet with instructions and trained staff to help with comprehension and completion. Unlike previous questionnaires, it measures the 5 dimensions of the construct perceived risk of skin cancer. Consistent with Janssen et al.,17 it was necessary to use structured items comparatively and conditionally; however, the dimensions of severity and probability only included items of absolute structure. The appearance and content validity of the instrument was achieved by having a representative set of items, which were formulated according to the bibliographic review, construct content sampling, author consensus, and the final review by an expert in the design and validation of psychometric instruments. In addition, we demonstrated the construct validity of the questionnaire using factor analysis, which made it possible to eliminate items that did not have the necessary profile. The consistency or internal reliability of the instrument is good, and we intend to apply temporal consistency tests such as test-retest. As this is an instrument that measures perceived risk, it is not absolutely necessary to measure internal reliability; however, internal consistency must be determined.
The main limitation of this instrument is that associated with the characteristics of the study sample. The sample chosen for validation of the instrument comprised patients attending a reference dermatology clinic in Mexico; most were women, and mean age was 38 years. In addition, the objective of our instrument was to measure perceived risk of skin cancer involving sun exposure, namely, basal cell carcinoma, squamous cell carcinoma, and melanoma, since prevention in these neoplasms focuses on avoiding risk behavior associated with sun exposure. However, there are other risk factors that, by their very nature, cannot be modified.
Perceived risk of skin cancer is an extremely useful measure in studies of clinical interventions to prevent skin cancer, since dissemination of information on skin cancer is not sufficient to ensure that preventive measures are adopted. Furthermore, it is essential that people realize that they are at risk of skin cancer so that they can modify their behavior with respect to sun exposure and protection.21 Therefore, improved perception of risk would be associated with behaviors aimed at sun protection. This is the reason why we propose that perceived risk be used to modify behavior and that the information provided to the general public and to high-risk groups should impact individuals in such a way that they perceive or identify the risk.
In summary, this validated Spanish-language questionnaire serves as a measurement tool in intervention studies on approaches to preventing skin cancer.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed their hospital's protocol on the publication of data concerning patients and that all patients included in the study have received sufficient information and have given their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare that no private patient data are disclosed in this article.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Morales-Sánchez M, Peralta-Pedrero M, Domínguez-Gómez M. Diseño y validación de un cuestionario para medir percepción de riesgo de cáncer de piel. Actas Dermosifiliogr. 2014. 105:276–285.