We present a series of 6 cases of disseminated superficial actinic porokeratosis and describe their dermoscopic features.
Dermoscopy is a noninvasive in vivo technique that is useful as a tool for the diagnosis and follow-up of porokeratosis. This condition has specific dermoscopic features that were observed in our series of cases and that are consistent with reports in the international literature.
Presentamos una serie de 6 casos de poroqueratosis actínica superficial diseminada en los cuales se describen las características dermatoscópicas halladas en cada uno de ellos.
La dermatoscopia es una técnica no invasiva in vivo útil como herramienta diagnóstica y de seguimiento en la poroqueratosis ya que se describen elementos dermatoscópicos específicos de esta entidad observados en nuestra serie de casos, que concuerdan con lo comunicado en la literatura internacional.
Porokeratosis (PK) is a group of chronic, progressive disorders of keratinization that includes several subtypes with a broad clinical spectrum.1
Five clinical variants of PK have been described based on different patterns of distribution. PK of Mibelli, disseminated superficial PK, linear PK, punctate palmoplantar PK, and disseminated superficial actinic PK (DSAP).2,3 An eruptive form of PK with a rapidly progressive clinical course has also been described, with lesions affecting the entire skin surface. This form of porokeratosis has been associated with malignancies, immunosuppression, and proinflammatory states, although the small number of reported cases makes relationships difficult to demonstrate.4 Other proposed variants include malignant disseminated PK, PK plantaris discreta, and reticular PK.5
DSAP is the most common clinical subtype.2,6,7 It is a chronic, autosomal dominant disease characterized by multiple erythematous-to-brownish papules and annular plaques with a well-defined hyperkeratotic border around a sometimes atrophic central area.5,8 Lesions usually start to appear in adolescence, in exposed areas; complete penetrance is reached in the third or fourth decade of life. The disease is rare in black individuals and in the elderly.1,5 Histopathology shows a narrow column of parakeratotic cells, the cornoid lamella, extending through the stratum corneum. This correlates clinically with the raised hyperkeratotic border.2,6
The dermoscopic features of DSAP suggest the diagnosis. We describe a series of 6 patients in which we detected several dermoscopic features associated with DSAP that are useful for diagnosis and follow-up.
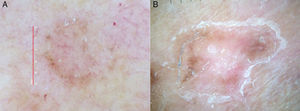
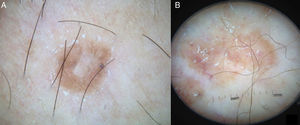
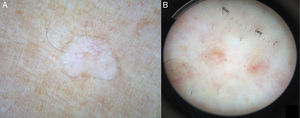
Case descriptionsThe clinical findings of each case are summarized in Table 1. The following dermoscopic alterations were observed: in case 1, a central area of atrophy was surrounded by an annular border with scales (Fig. 1A); in case 2, the lesions presented vascular structures and a hyperkeratotic border (Fig. 1B); brownish dots and central atrophy were observed in case 3 (Fig. 2A); central hairpin vessels were seen crossing the plaques in case 4 (Fig. 2B); in case 5 there was a scar-like area (Fig. 3A); and in case 6, irregular vessels were visible in a central area of atrophy surrounded by a hyperkeratotic border (Fig. 3B).
Clinical details of the case series.
| Patient | Sex | Age, y | Phototype | Relevant past history | Disease duration | Symptoms | Site | Clinical findings | Dermoscopy |
|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 45 | II | No | 5 years | Pruritus | Sun exposed areas of upper limbs | Multiple, well-defined, slightly erythematous papules with peripheral enhancement. Fine pigmented desquamation | Fig. 1A |
| 2 | M | 37 | III | Occupational sun exposure | 6 months | No | Sun exposed areas of lower limbs | Same clinical features as patient 1 | Fig. 1B |
| 3 | F | 51 | III | Smoker | Unknown | Pruritus | Sun exposed areas of upper and lower limbs | Erythematous-to-brownish papules with fine scales and pale central area | Fig. 2A |
| 4 | M | 62 | II | Asthma | 18 months | No | Sun exposed areas of both lower limbs | Erythematous and brown plaques with fine peripheral scales | Fig. 2B |
| 5 | F | 55 | II | No | 2 years | No | Upper limbs and upper back | Brown-to-grey plaques of 1-cm diameter, with a raised scaly grey border and a hypopigmented central area | Fig. 3A |
| 6 | F | 58 | II | No | Unknown | No | Sun exposed areas of the limbs | Same clinical features as patient 4 | Fig. 3B |
Abbreviations: F, female; M, male.
Biopsy was performed in all patients to confirm the diagnosis of DSAP. At the time of writing, the clinical and dermoscopic follow-up had been of 18–36 months.
DiscussionPorokeratosis is a group of disorders in which there is a disturbance of keratinization. DSAP typically affects sun-exposed areas, suggesting that UV radiation may be the most important extrinsic factor.3,6
Although the aetiology is unknown, recent studies have suggested a mutation of the mevalonate kinase (MVK) gene on chromosome 12q24 as the cause of DSAP. This mutation has been detected in several patients diagnosed with DSAP, but because of the few cases that have been reported, the exact causes of the gene mutation are unknown.6,7
Mevalonate kinase, encoded by the MVK gene, is an enzyme involved in cholesterol synthesis. Overexpression of this protein promotes differentiation of keratinocytes that produce type 1 keratin. The expression of this protein protects keratinocytes from UV-A-induced apoptosis.7 DSAP is primarily associated with UV radiation and immunosuppression, but also occurs in organ transplants recipients, patients with psoriasis, or after the administration of thiazides (phototoxic drugs), and in several cases has been related to primary lymphedema.3,6,8 The malignant potential, thought to be due to overexpression of p53 protein, must be taken into consideration as there is an association with squamous cell carcinoma, basal cell carcinoma, and Bowen disease. The risk of malignant transformation appears to be higher with a longstanding history of injuries, in larger lesions, and in elderly or immunocompromised patients.6
The diverse clinical presentations represent different phenotypic expressions of the same genetic alteration due to the coexistence of distinct types of porokeratosis in the same patient or in different members of a single family.5,7
Porokeratosis presents clinically as annular erythematous-to-brownish lesions surrounded by a hyperkeratotic border which corresponds to the typical histopathologic feature, the cornoid lamella. The cornoid lamella is a column of parakeratotic cells located in a depression in the epidermis where the granular layer is absent; it is a characteristic but not pathognomonic sign of porokeratosis. All forms of porokeratosis have similar histopathologic features. A further important histologic finding observed in most cases is the presence of dyskeratotic keratinocytes and a mild dermal inflammatory infiltrate composed of plasma cells and occasional granulocytes.2,3 Dermoscopy is of recognized value in the differentiation of erythematous diseases with similar clinical features.9 In DSAP, dermoscopy is useful because it reveals specific diagnostic criteria.9,10 The dermoscopic findings in the 6 patients analyzed match those already reported in the literature (Table 2). UV dermoscopy highlights the hyperkeratotic border, which glints, resembling a diamond necklace.10 Ink has been used to stain porokeratosis lesions, revealing large pores with keratotic plugs.11
Dermoscopic features of disseminated superficial actinic porokeratosis.
| White peripheral border also more prosaically known as lines of volcanic crater seen from above |
| Homogeneous central white scar-like area |
| Brownish globules or dots |
| Vascular structures: |
| - pinpoint vessels |
| - irregular linear vessels crossing the lesion |
The treatment of DSAP by excisional surgery is impractical in the majority of cases. However, given its potential for malignant transformation, dermoscopic monitoring of lesions enables early treatment to be provided when necessary.
Several treatments have been proposed, but they are unsatisfactory in most cases and none is globally effective.5,8 The need for meticulous sun protection, emollients, and monitoring due to the risk of malignant transformation are key elements of therapy.5 Use of the different modalities to treat a purely cosmetic alteration, such as DSAP, is questionable. Proposed treatments include 5-fluorouracil, imiquimod, vitamin D analogues, and cryotherapy; recent descriptions of photodynamic therapy with topical hypericin have reported variable degrees of success.2,5
In conclusion, dermoscopy is a rapid technique that can help to improve the clinical diagnosis of DSAP.2,3 In view of the extensive therapeutic arsenal and the variable results, it is important to reach a correct diagnosis. Dermoscopic monitoring should be performed because of the risk of malignant transformation, especially into squamous cell carcinoma, with a reported incidence between 3.4% and 11%.1,3
We have highlighted the value of dermoscopic evaluation in cases in which the clinical features are consistent with a diagnosis of porokeratosis.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the responsible Clinical Research Ethics Committee and in accordance with those of the World Medical Association and the Helsinki Declaration.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors must have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence must be in possession of this document.
Conflict of interestThe authors declare no conflict of interest.