Jellyfish are free-living members of the phylum Cnidaria who share a specialized stinging cell, the cnidocyte. Pelagia noctiluca is the most frequent and toxic jellyfish species found in the Balearic beaches and cnidocytes are arranged in pigmented clusters called “warts”. Dermoscopy continues to expand its use much beyond the pigmentary lesions and to date, there is no data regarding dermoscopic findings in jellyfish stings. The aim of the present work was to study the dermoscopic findings of jellyfish stings in the island of Mallorca.
Patients and methodsWe retrospectively reviewed the clinical and dermoscopic images of 25 episodes of jellyfish stings caused by P. noctiluca that occurred between 2009 and 2015.
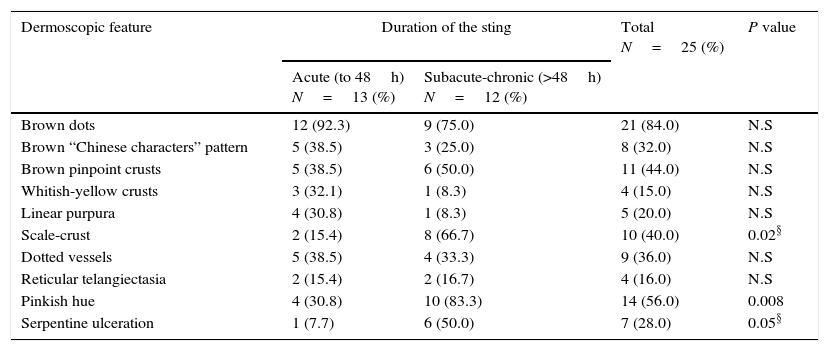
ResultsOverall, the following dermoscopic features were found: brown dots (84%), pinkish hue (56%), pinpoint brown crusts (44%), scale-crust (40%), brown “Chinese characters pattern” (32%), “serpentine” ulceration (28%), linear purpura (20%), and whitish-yellow crusts (15%). Vessels were mainly dotted (36%) or reticular (16%). Scale-crust, serpentine ulceration and pinkish hue were significantly more frequent in lesions older than 2 days.
Conclusions and limitationsOur study identifies 4 dermoscopic features that may represent the contact with P. noctiluca cnidocytes: brown dots, brown “Chinese characters pattern”, pinpoint brown crusts and whitish-yellow crusts. A peculiar finding of “serpentine ulceration” with brown dots would be very suggestive of P. noctiluca sting. We believe dermoscopy is a valuable tool in the diagnosis of jellyfish stings when a clear history of contact is lacking. Further studies are needed to validate our findings in other jellyfish species.
Las medusas son miembros del phylum Cnidaria que comparten una célula urticante especializada, el cnidiocito. En Baleares, Pelagia noctiluca es la medusa más frecuente y tóxica. En ella los cnidiocitos se encuentran en agrupaciones pigmentadas llamadas «verrugas». La dermatoscopia continúa ampliando su uso más allá de las lesiones pigmentadas, pero hasta la fecha no se ha utilizado en el diagnóstico de las picaduras de medusa. El objetivo del presente trabajo es estudiar los hallazgos dermatoscópicos en esta patología en la isla de Mallorca.
Pacientes y métodosRevisamos retrospectivamente las imágenes clínicas y dermatoscópicas de 25 episodios de picaduras de medusa por P. noctiluca entre 2009 y 2015.
ResultadosSe encontraron las siguientes imágenes: puntos marrones (84%), tono rosado (56%), costras marrones puntiformes (44%), escamocostra (40%), patrón en «letras chinas» marrones (32%), ulceración «en serpentina» (28%), púrpura lineal (20%) y costras blancoamarillentas (15%). Los vasos fueron puntiformes (36%) o reticulares (16%). La escamocostra, la ulceración en serpentina y el tono rosado fueron significativamente más frecuentes en las lesiones de más de 2días de duración.
Conclusiones y limitacionesNuestro estudio identificó 4 imágenes dermatoscópicas debidas al contacto con los cnidiocitos: puntos marrones, patrón en «letras chinas» marrones, costras marrones puntiformes y costras blancoamarillentas. La combinación de ulceración «en serpentina» y puntos marrones sería muy sugestiva de picadura por P. noctiluca. La dermatoscopia es una herramienta útil en el diagnóstico de las picaduras de medusas, en ausencia del antecedente de contacto con ellas. Se necesitan más estudios para validar estos hallazgos en picaduras por otras especies de medusa.
Jellyfish are free-living members of the phylum Cnidaria with whom they share a highly specialized cell type of mechanoreceptor, the cnidocyte or cnidoblast, each containing an intracellular organelle, the nematocyst. Nematocysts are formed and used only by cnidarians to capture and immobilize preys and to defense against predators. Following an appropriate stimulus, either chemical or mechanical, the cnidocyte discharges its nematocysts and injects the venom into the victim.1 The venom of jellyfish is composed of potent proteinaceous porins, neurotoxic peptides, bioactive lipids and other small molecules that are responsible for its cytotoxic, cytolytic, haemolytic and antigenic properties.2 Jellyfish stings produce direct immediate toxicity, either local (pain, oedema, inflammation and necrosis) or systemic. In a small number of patients, they may also trigger an immune response such as anaphylaxis, pruritus, erythema nodosum,1 lichen-planus like eruption3 and persistent or recurrent cutaneous reactions.4 Long-term complications including granulomatous reactions, keloids, retractile scars, pigmentary changes (hyper- or hypopigmentation) or fat atrophy may also occur.1
The diagnosis of jellyfish stings is straightforward and is based on the clinical manifestations and personal history of contact with the Cnidarian. When a clear history of contact with jellyfish is lacking, the lesions may be confused with herpes, impetigo, phytophotodermatitis, stings from other marine animals or with other dermatosis following a whiplash pattern.1,5–9 In these doubtful cases, the microscopic examination of a sticky tape applied to the sting site or the visualization of skin scrapings suspended in saline solution, may reveal the presence of nematocysts adhered to the corneal layer and should allow the identification of the species that caused the sting.1 Also, nematocysts remain attached to the victim's skin from hours to days, and can be detected in a cutaneous biopsy.1,10 Dermoscopy is a rapid non-invasive technique that has been used for the diagnosis of infestations such as scabies, pediculosis, cutaneous larva migrans, ticks and Trombicula bites among others.11 In a previous study, we evaluated the dermoscopic findings of jellyfish stings in 8 patients and only 3 patients were able to identify the jellyfish species, that corresponded to Pelagia noctiluca.12 The aim of the present work is to study the dermoscopic findings of jellyfish stings in a larger group of patients in The Island of Majorca.
Patients and methodsWe retrospectively reviewed the clinical and dermoscopic images of jellyfish stings evaluated in our department during the last seven years (from May 2009 to October 2015). To avoid misdiagnosis, only patients who had identified the jellyfish in close contact with the skin or in the vicinity were included. The identification of the jellyfish was made by the patient or his companions at the time of the sting and was confirmed at the time of consultation by means of a slideshow with pictures that included the most frequent jellyfish found in the Mediterranean Sea.7 These pictures were downloaded from internet, mainly from “https://www.wikipedia.org”.
The following data were collected for each episode: age and sex, location, morphology of the sting (lines, patch or both), date when the sting occurred and if biopsy was performed. Dermoscopic evaluation included the following features: pigmentation pattern, vascular pattern and presence of ulceration, crusting or scaling. To check if dermoscopic signs changed over time, we classified jellyfish stings in acute (up to 48h) and subacute-chronic (between 48h and 30 days), based on the course of experimental jellyfish stings where the erythema during the acute phase disappeared in 2–3 days.13
Statistical analysis was performed using SPSS version 21.0 (IBM Corporation). Pearson's chi square test was used to compare percentages. When indicated, Yates's correction of continuity was applied. P-value cutoff was set at 0.05.
ResultsWe included 25 episodes of jellyfish sting in 22 patients, 11 females and 11 males. Age ranged from 2 to 74 years (mean 42, median 46.5). All stings occurred between May and October and 63.7% between June and August. In our series, the only jellyfish species that our patients identified as responsible for the sting was P. noctiluca; so eventually only stings by this species were included. Three cases had already been included in our previous series.12 Lesions were found in the upper limb (40.7%), lower limb (18.8%), trunk (31.3%) and head/neck (9.3%). Three patients presented two episodes of jellyfish sting. In 5 patients, lesions affected simultaneously two body areas and in one patient, three body areas were affected. Eleven jellyfish stings (44%) presented with linear lesions (including the whiplash pattern), 9 (36%) as circular patches (single or multiple), and 5 (19%) presented a combination of both. In three of these 5 cases, the complete shape of the jellyfish was drawn on the skin. Jellyfish sting duration at time of consultation ranged from 1h to 30 days (mean 4.9 days, median 2 days). Thirteen stings (52%) were classified as acute, and 12 stings (48%) as subacute-chronic.
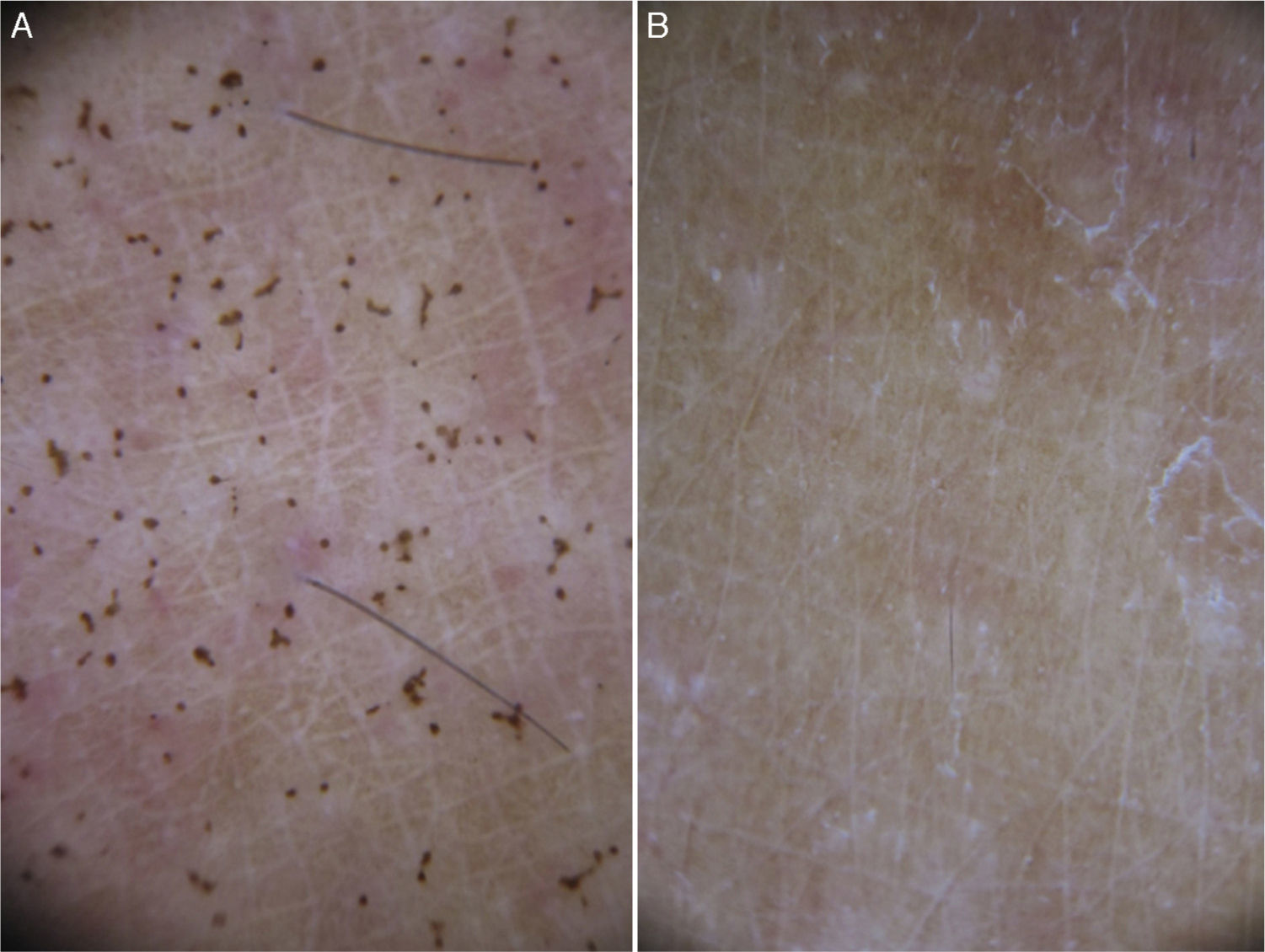
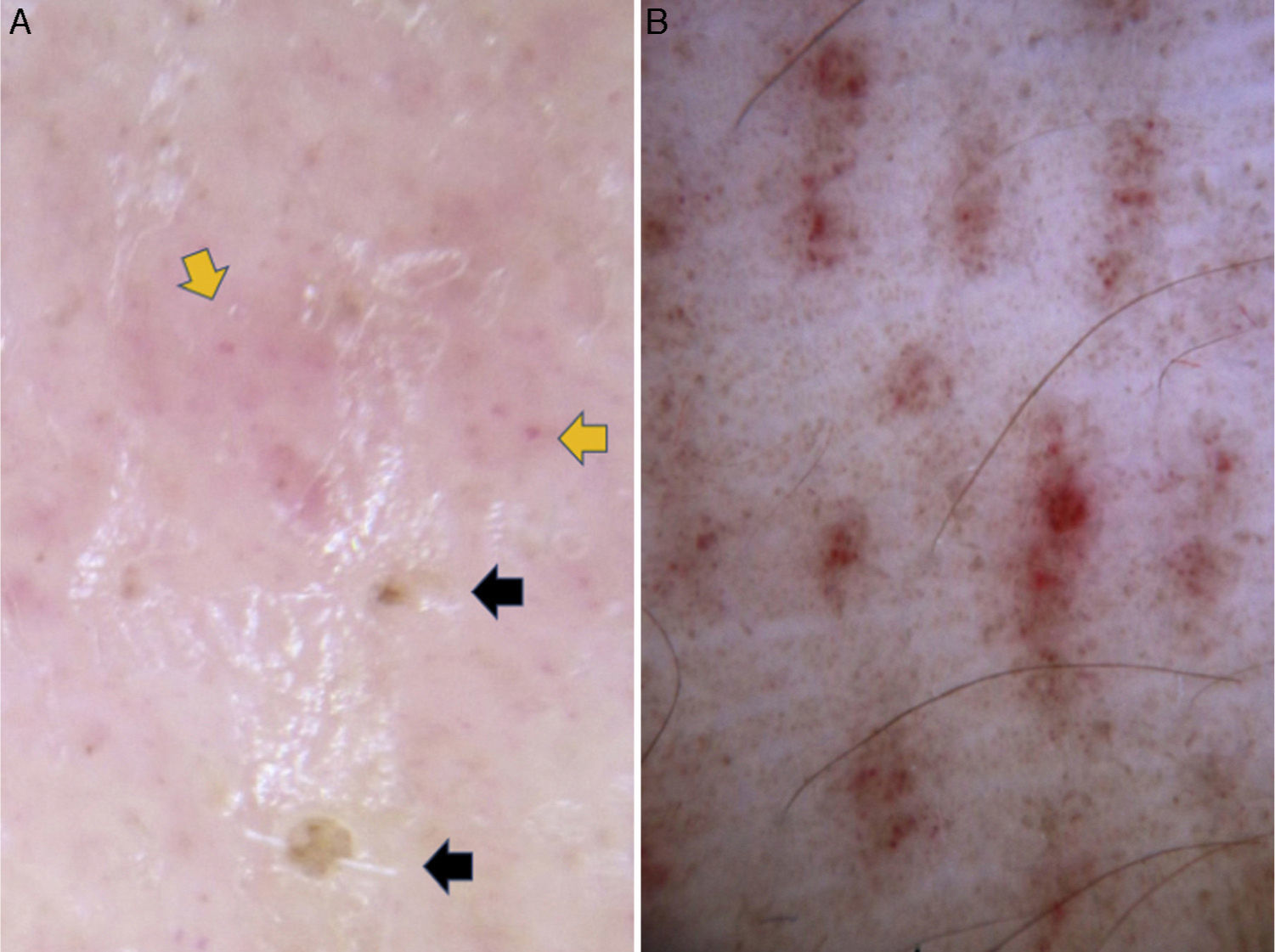
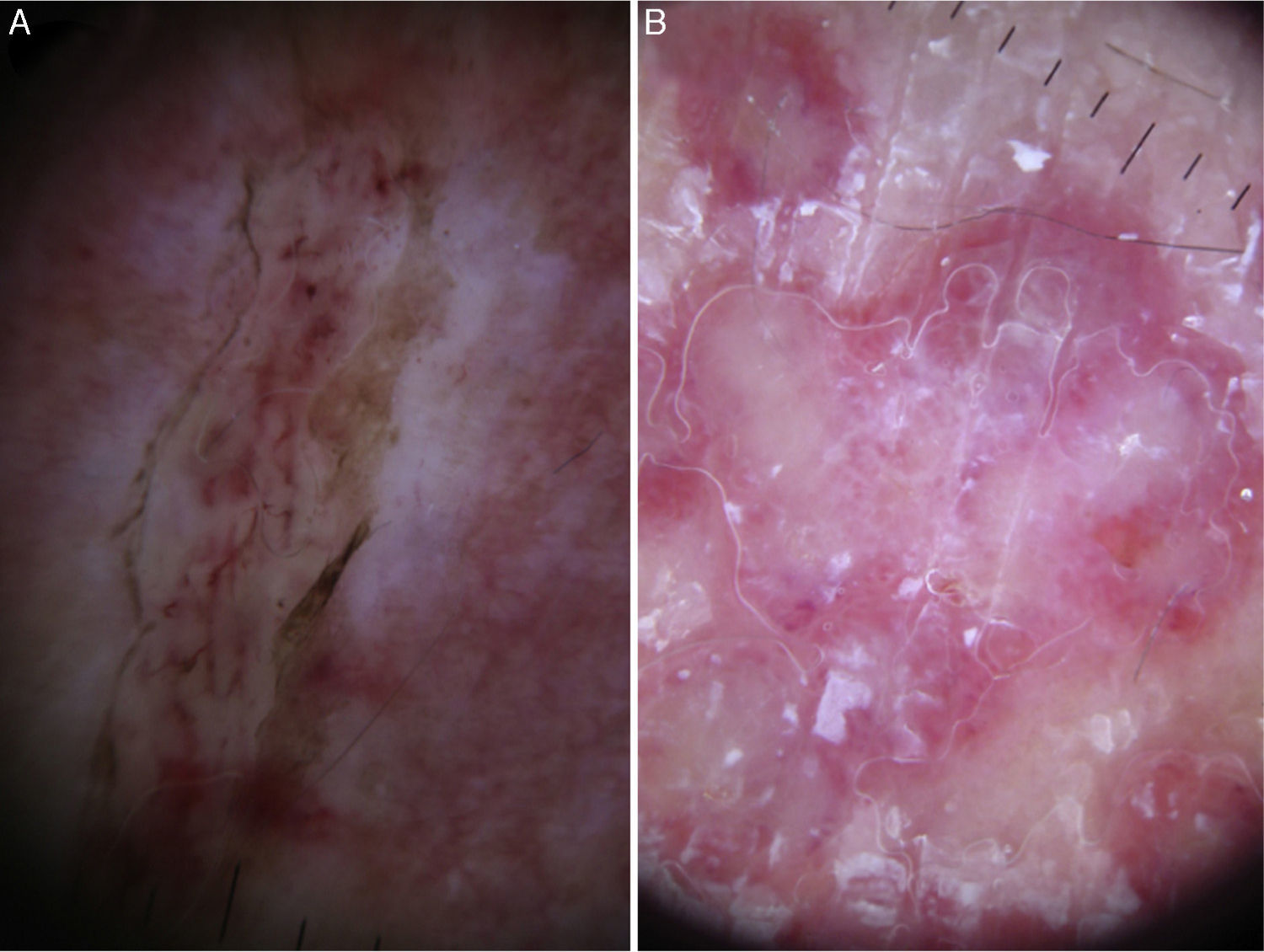
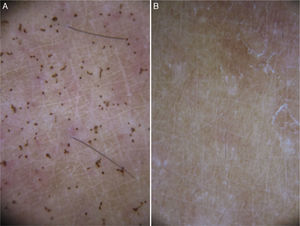
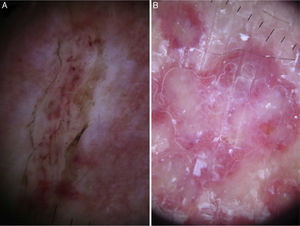
We found the following dermoscopic features (Figs. 1–4): brown dots (84.0%), pinkish hue (56.0%), pinpoint brown crusts (44.0%), scale-crust (40.0%), brown “Chinese character” pattern (32.0%), “serpentine” ulceration (28.0%), linear purpura (20.0%), and whitish-yellow crusts (15.0%). When vascular pattern was present, vessels were mainly dotted (36.0%) or reticular (16.0%). In Table 1, the frequency of dermoscopic features is summarized according to the time since the sting occurred. Scale-crust, serpentine ulceration and pinkish hue were significantly more frequent in lesions older than 2 days. Circular milky-red areas were observed in only one case of persistent chronic reaction. Linear purpura and reticular telangiectasia were no longer observed after 7 days. Histopathological study was performed in a jellyfish sting 18h duration, from a selected area containing brown dots dermoscopically (Fig. 5).
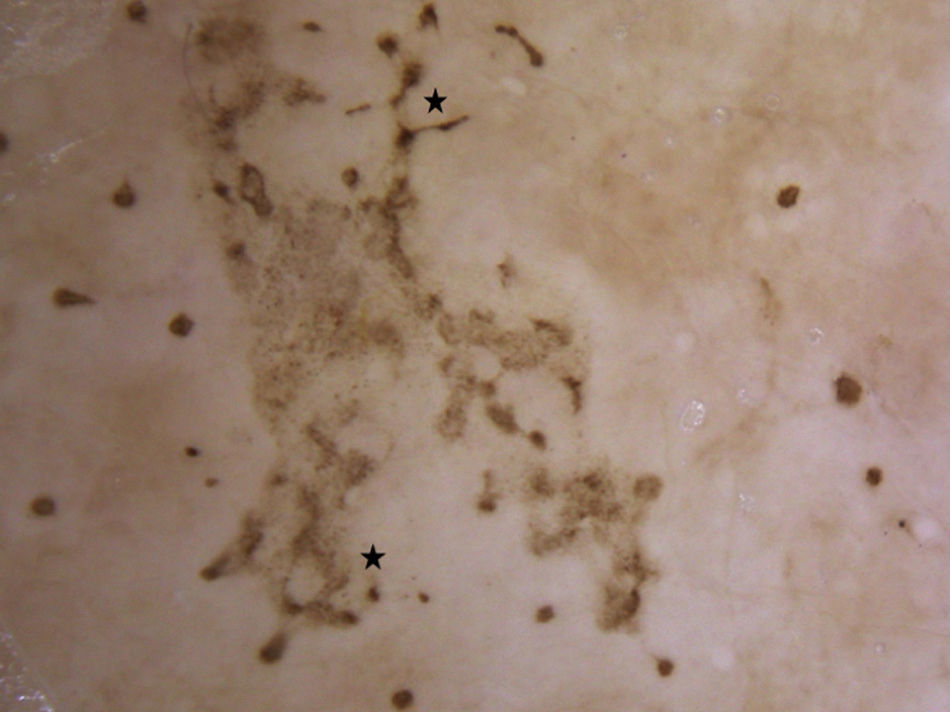
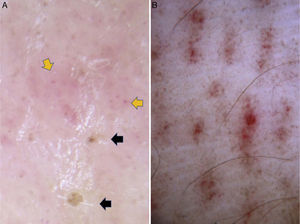
Dermoscopic findings in Pelagia noctiluca stings. Brown “Chinese characters” pattern. Brown dots appear connected by lines (*) composed of a fine light brown granular pigment, resembling Chinese letters. Clinical presentation corresponded to linear vesicles regularly spaced due to the contact with the “warts” contained in the oral arms of Pelagia noctiluca.
Dermoscopic findings in Pelagia noctiluca stings. Serpentine ulceration and circular milky-red areas. (A) Superficial linear ulceration presents as a winding road due to the contact with the tentacles of the jellyfish (“serpentine ulceration”). The edges of the ulcer are delimited by scales and contain brown dots. Linear purpura is shown inside the ulcer. (B) Distinctive “circular milky-red areas” on a recurrent, persistent, inflammatory reaction to jellyfish sting. The configuration of these circular milky-red areas match with the “warts” morphology of the jellyfish.
Dermoscopic findings in 25 episodes of Pelagia noctiluca stings.
| Dermoscopic feature | Duration of the sting | Total N=25 (%) | P value | |
|---|---|---|---|---|
| Acute (to 48h) N=13 (%) | Subacute-chronic (>48h) N=12 (%) | |||
| Brown dots | 12 (92.3) | 9 (75.0) | 21 (84.0) | N.S |
| Brown “Chinese characters” pattern | 5 (38.5) | 3 (25.0) | 8 (32.0) | N.S |
| Brown pinpoint crusts | 5 (38.5) | 6 (50.0) | 11 (44.0) | N.S |
| Whitish-yellow crusts | 3 (32.1) | 1 (8.3) | 4 (15.0) | N.S |
| Linear purpura | 4 (30.8) | 1 (8.3) | 5 (20.0) | N.S |
| Scale-crust | 2 (15.4) | 8 (66.7) | 10 (40.0) | 0.02§ |
| Dotted vessels | 5 (38.5) | 4 (33.3) | 9 (36.0) | N.S |
| Reticular telangiectasia | 2 (15.4) | 2 (16.7) | 4 (16.0) | N.S |
| Pinkish hue | 4 (30.8) | 10 (83.3) | 14 (56.0) | 0.008 |
| Serpentine ulceration | 1 (7.7) | 6 (50.0) | 7 (28.0) | 0.05§ |
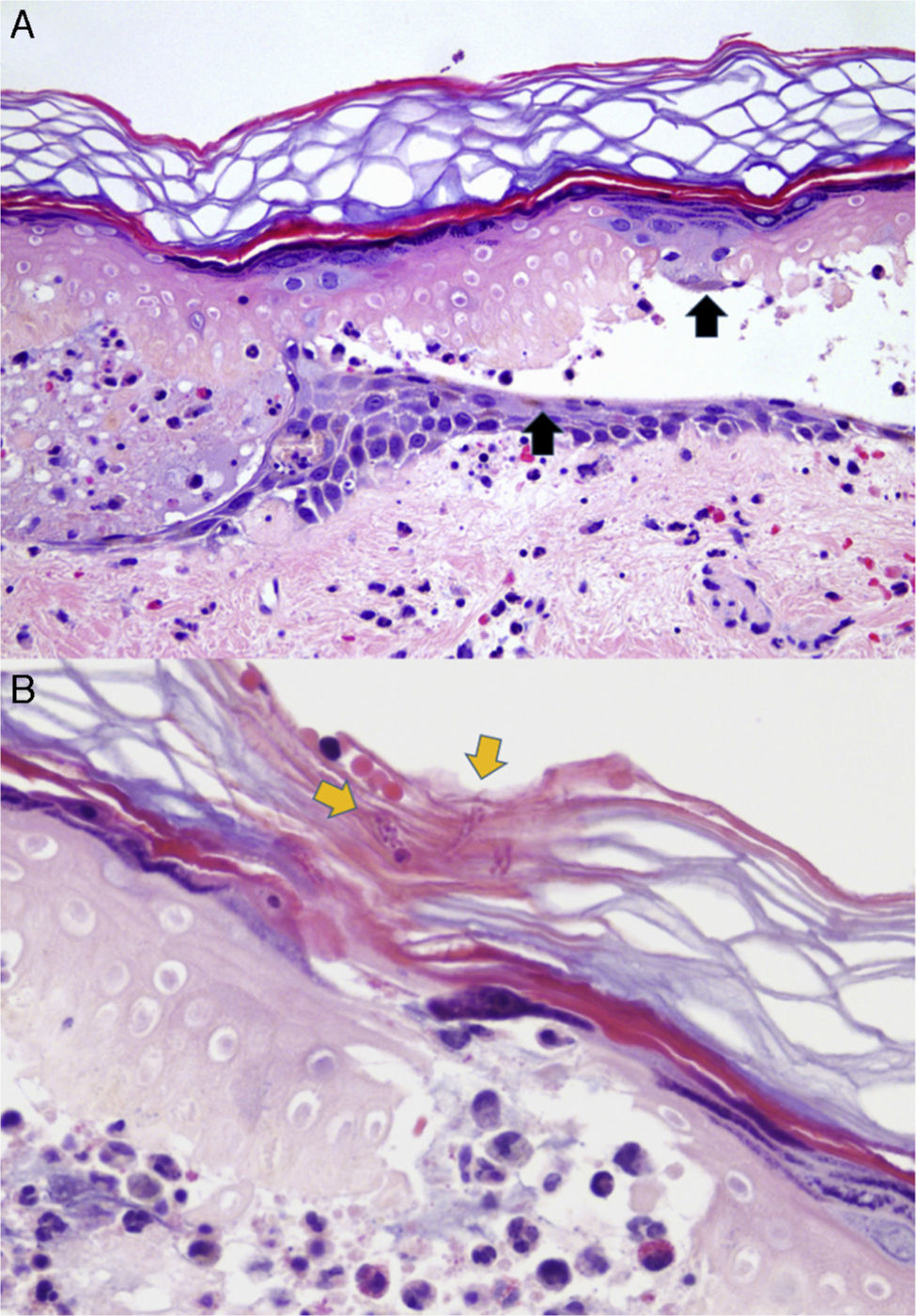
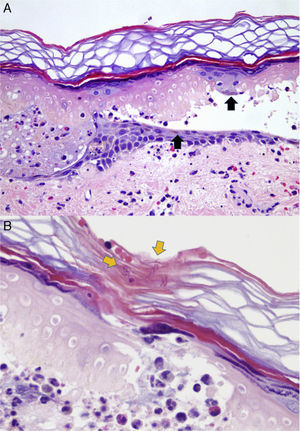
Dermoscopic-pathological correlation of brown dots. (A) Epidermal necrosis with vesicle formation. Melanin is found dispersed into the debris and remnants of pigmented keratinocytes (black arrows). Dermal inflammation with oedema, vasodilatation and erythrocyte extravasation is shown (H&E 100×). (B) Fragments of the tubules of nematocysts are seen in the stratum corneum (yellow arrows) (H&E 200×).
Jellyfish stings are very common among sea bathers in the Balearic Islands. In the summer of 2014, sea lifeguards attended 12,860 swimmers in the Balearic beaches, and of these, 209 were treated for jellyfish stings.14 However, jellyfish stings are not a frequent cause of dermatologic consultation since most cutaneous lesions are mild and transient.2,15 Several species in the Mediterranean sea, including P. noctiluca (mauve stinger), Rhizostoma pulmo (barrel jellyfish), Chrysaora hysoscella (compass jellyfish), Caribdaea marsupialis (sea wasp), Rhopilema nomadica and possibly, Aurelia aurita (moon jellyfish) are considered potentially harmful to humans.7,16 According to reports from a network of observers, the only toxic jellyfish species found in the Balearic beaches are P. noctiluca and less frequently, A. aurita.17P. noctiluca is by far the most common jellyfish found in the Mediterranean Sea7,16,18 and this could explain that it was the only identified species in our series.
P. noctiluca has four thick oral arms and a bell or exumbrella of 4–13cm in diameter with eight thin tentacles hanging from it which can reach up to 3 or more metres in length.1 Their nematocysts are arranged in characteristic clusters called “warts” distributed over its entire surface, which makes the whole body, including the bell, potentially toxic.2,15
Contact with P. noctiluca causes immediate pain, burning and erythematous-edematous vesicular lesions, that follow a linear or whiplash distribution if the contact is established with its tentacles.2,15 Sometimes, it is possible to see the “print” of the bell on the skin, which appears as a circular patch; and less frequently the complete silhouette of the jellyfish is observed.15,19 Lesions usually resolve in 1–2 weeks and may leave a scar or pigmentary changes.15,20 Recurrent skin eruptions have been described,2,21 and in our series, only one patient developed a recurrent eruption. Dermoscopy in this case revealed the presence of circular, confluent, milky-red areas reminiscent of the jellyfish's warts (Fig. 4B).
Similar to other series,15,16 lesions were located mainly on the extremities and in contrast to previous studies no male predilection was found. This finding may reflect an inclusion bias.
The results of our study reveal 4 dermoscopic features that may represent the contact with the nematocysts of P. noctiluca: brown dots, brown “Chinese character pattern”, pinpoint brown crusts and whitish-yellow crusts. These features were observed in jellyfish stings from unidentified species,12 suggesting that P. noctiluca may have been the causative species, although further studies are needed to support this assumption.
Histological examination of jellyfish stings reveal nematocysts above the stratum corneum and fine thread-like tubules penetrating the epidermis.10 We performed selected skin biopsy from dermoscopic brown dots in a sting of 18h duration and observed dermoepidermal necrosis and fragments of fine refractile threads of the nematocysts in the epidermis (Fig. 5). Dermoscopic-pathological correlation of this single case suggests that “brown dots” may represent the entry point of the nematocyst into the skin (Fig. 1). We used the term “pinpoint brown crusts” (Fig. 3) in larger lesions that may correspond to deeper dermal penetration of the nematocyst, with more necrosis and central crusting. When no pigment was observed, the term “whitish-yellow crusts” was used.
The exumbrella and oral arms of P. noctiluca have brown pigment of melanic nature mainly located on the “warts”.22 We could speculate that this exogenous pigment could penetrate the skin through the puncture20 contributing to the brown colour observed on dermoscopy. However, the more probable explanation is that the brown colour is due to epidermal melanin dispersed in the necrotic content of the vesicles, as observed in the histology (Fig. 5A). When the vesicles observed histologically merge, the resulting dermoscopic image is a combination of dots and lines that do not follow the normal skin marks. Because are reminiscent of the Chinese alphabet letters, we termed this pattern brown “Chinese characters” (Fig. 2). Interestingly, at least one of the dermoscopic brown structures described was present in 23 episodes (88%) and these findings may be a characteristic dermoscopic feature of P. noctiluca stings. Although less common than the brown dots, the brown “Chinese characters” pattern, to our knowledge, has not been described in any other disease yet. All of these dermoscopic features disappeared over time, and were no longer perceptible after 4 weeks (Fig. 1B). These findings may help us in the differential diagnosis with post-inflammatory pigmentation due to the jellyfish sting,15,20 which shows blue or grey granules on dermoscopy, corresponding to melanin in the papillary dermis.23
Histological analysis of jellyfish stings often show extravasation of erythrocytes10 (Fig. 5) and we believe that clinical visualization of linear purpura (Fig. 3B) is most probably caused by direct toxicity of the vascular endothelium from the P. noctiluca venom.2 Dermoscopic vascular features such as pinkish hue and red dots (Fig. 3A) were more frequent in chronic lesions. The red dots may be due to toxic or immunologic damage of the venom to the vessels. Circular milky-red areas were observed in only one case of persistent chronic reaction (Fig. 4B). The dermoscopic image of serpentine ulceration (Fig. 4A) may be explained by the cytotoxic and dermonecrotic properties of the venom.2 The feature of serpentine ulceration together with brown dots would be very suggestive of contact with the tentacles of P. noctiluca.
Although visual recognition of the jellyfish is the usual method to identify the jellyfish species in field studies,17,18 this method may involve species misclassification. In our series, all patients were residents and had no difficulty in recognizing the jellyfish when the pictures were shown. The second most frequent jellyfish that regularly arrives at the Balearic beaches is A. aurita,17 easily distinguishable from P. noctiluca. Misrecognition with C. hysoscella (compass jellyfish) or Chrysaora quinquecirrha (sea nettle) is possible, but both are much less common than P. noctiluca in our beaches.16,17 Another limitation of our study is that our findings are limited to an unique jellyfish species. Further studies are needed to evaluate these dermoscopic features in jellyfish stings caused by species other than P. noctiluca.
In conclusion, this study of the dermoscopic spectrum of jellyfish stings identifies 4 dermoscopic features that may represent the penetration of P. noctiluca nematocysts: brown dots, brown “Chinese characters” pattern, pinpoint brown crusts and whitish-yellow crusts. We believe that our study provides further knowledge in an unexplored field of dermoscopy. The recognition of these dermoscopic findings in typical cases of P. noctiluca stings may help us to establish the diagnosis when a clear history of contact with the cnidarian is lacking.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Conflicts of interestThe authors declare no conflict of interest.