Dermoscopy is a non-invasive diagnostic method that is used to evaluate morphological structures not visible to the human eye; dermoscopy thus helps us to differentiate and diagnose skin lesions.1 It is a useful tool that has enabled us to perform rapid in vivo study.2 There have been few publications on the use of dermoscopy for the diagnosis of skin metastases from malignant internal tumors.
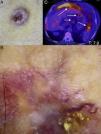
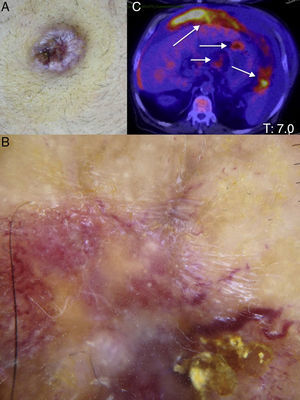
We describe the case of a 67-year-old man who was seen for abdominal distension and an umbilical nodule that had appeared 6 months earlier. The patient reported constipation, abdominal pain, and weight loss of 5kg in the previous month. On examination there was a firm, irregular, ulcerated erythematous nodule of 5cm diameter at the umbilicus (Fig. 1A). The nodule contained serous fluid. Dermoscopy of the nodule with polarized light revealed white shiny structures and an atypical polymorphous vascular pattern with serpentine vessels and curved vessels with milky-red areas (Fig. 1B). This observation of polymorphous vessels and white shiny structures was suggestive of malignancy. Histopathology of the umbilical nodule revealed subcutaneous infiltration by a metastasis from an adenocarcinoma of the colon; the lesion was positive for cytokeratins CK7 and CK20 and CDX-2. Computed tomography and positron emission tomography showed a tumor mass at the hepatic angle of the colon, with liver, umbilical, and peritoneal metastases (Fig. 1C). Two liters of ascitic fluid were drained on paracentesis. Tumor resection was then considered, but the patient died before this could be performed.
Sister Mary Joseph's nodule (SMJN) is an eponym for umbilical skin metastasis from a malignant tumor. It is a rare manifestation, but may be the only presenting sign of a primary malignant visceral tumor.
The correct diagnosis of SMJN is crucial as it occurs predominantly in advanced or metastatic tumors. Clinically it presents as a small, irregular nodule that can be painful and can ulcerate; it can sometimes contain pus, blood, or serous fluid. The clinical differential diagnosis of SMJN includes malignant and benign lesions such as pyogenic granuloma, epidermal cyst, hemangioma, abscess, umbilical hernia, endometriosis, and primary umbilical carcinoma.3 Dermoscopic examination will exclude pyogenic granuloma, basal cell carcinoma, and inflammatory conditions, as these would present other types of vessels.
To date, 3 reports have been published on the dermoscopic features of skin metastases from internal malignant tumors. De Giorgi et al.4 and Oiso et al.5 described atypical polymorphous vascular patterns in skin metastases from a recurrent thyroid carcinoma and in a skin metastasis from a possible occult breast cancer. But it was Mun et al.6 who first described the dermoscopic features of SMJN that had arisen from an adenocarcinoma of the pancreas. Recently, Chernoff et al.7 published an article in which they analyzed the vascular patterns of skin metastases; the most typical dermoscopic findings were serpentine vessels, linear irregular vessels, and unstructured homogeneous areas of pink color.
The dermoscopic vascular pattern is considered to be a pathognomic phenomenon of neovascularization related to neoplastic growth.4 In the present case, dermoscopic examination of the umbilical lesion revealed a polymorphous vascular pattern that raised our suspicion of malignancy and led us to perform a skin biopsy that identified the presence of metastatic adenocarcinoma.
When an umbilical nodule is observed, a metastatic malignant tumor must be excluded as this may be its first clinical manifestation and indicates a poor prognosis. As far as we are aware, this is the second case report of the dermoscopic features of SMJN. The aim of this report is to increase the suspicion of a metastatic tumor when dermoscopic examination of an umbilical lesion reveals a polymorphous vascular pattern. Dermoscopy is now an essential additional tool for dermatologic diagnosis.
Please cite this article as: Garrido Colmenero C. Dermatoscopia del nódulo de la hermana María José. Actas Dermosifiliogr. 2015;106:511–512.