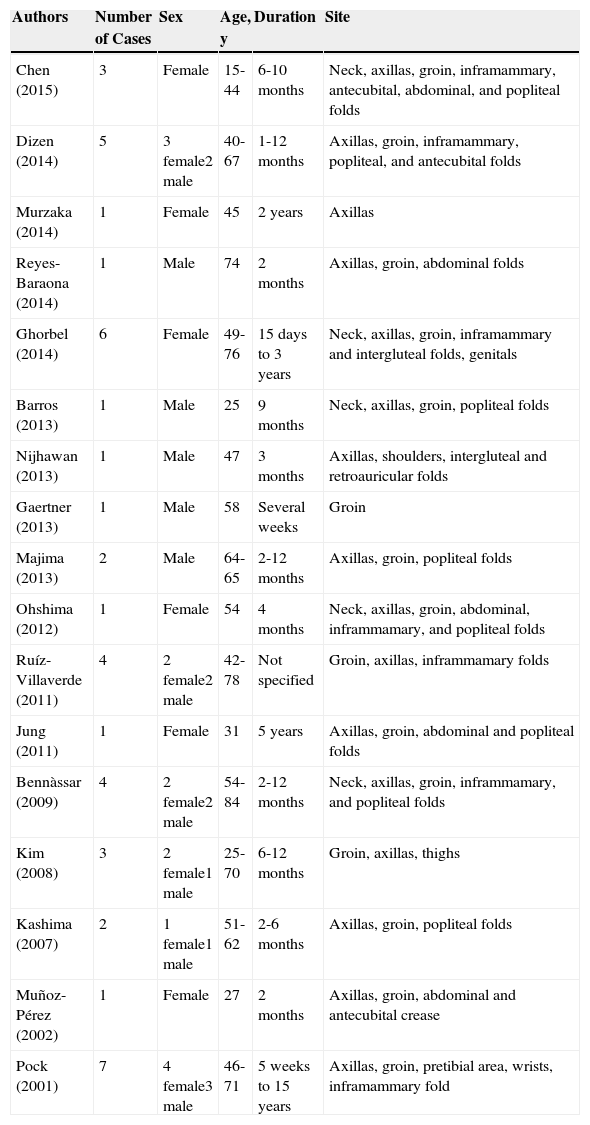
Lichen planus pigmentosus-inversus (LPPI) is a clinical variant of lichen planus, first described by Pock in 2001. To date, 44 cases have been published in the medical literature (Table 1). It usually presents as hyperpigmented macules or plaques located in the flexion creases. Dermoscopy is a useful tool for guiding diagnosis in clinically nonspecific pigmented lesions.
Description of Cases of Lichen Planus Pigmentosus Inversus Published in the Literature.
| Authors | Number of Cases | Sex | Age, y | Duration | Site |
|---|---|---|---|---|---|
| Chen (2015) | 3 | Female | 15-44 | 6-10 months | Neck, axillas, groin, inframammary, antecubital, abdominal, and popliteal folds |
| Dizen (2014) | 5 | 3 female2 male | 40-67 | 1-12 months | Axillas, groin, inframammary, popliteal, and antecubital folds |
| Murzaka (2014) | 1 | Female | 45 | 2 years | Axillas |
| Reyes-Baraona (2014) | 1 | Male | 74 | 2 months | Axillas, groin, abdominal folds |
| Ghorbel (2014) | 6 | Female | 49-76 | 15 days to 3 years | Neck, axillas, groin, inframammary and intergluteal folds, genitals |
| Barros (2013) | 1 | Male | 25 | 9 months | Neck, axillas, groin, popliteal folds |
| Nijhawan (2013) | 1 | Male | 47 | 3 months | Axillas, shoulders, intergluteal and retroauricular folds |
| Gaertner (2013) | 1 | Male | 58 | Several weeks | Groin |
| Majima (2013) | 2 | Male | 64-65 | 2-12 months | Axillas, groin, popliteal folds |
| Ohshima (2012) | 1 | Female | 54 | 4 months | Neck, axillas, groin, abdominal, inframmamary, and popliteal folds |
| Ruíz-Villaverde (2011) | 4 | 2 female2 male | 42-78 | Not specified | Groin, axillas, inframmamary folds |
| Jung (2011) | 1 | Female | 31 | 5 years | Axillas, groin, abdominal and popliteal folds |
| Bennàssar (2009) | 4 | 2 female2 male | 54-84 | 2-12 months | Neck, axillas, groin, inframmamary, and popliteal folds |
| Kim (2008) | 3 | 2 female1 male | 25-70 | 6-12 months | Groin, axillas, thighs |
| Kashima (2007) | 2 | 1 female1 male | 51-62 | 2-6 months | Axillas, groin, popliteal folds |
| Muñoz-Pérez (2002) | 1 | Female | 27 | 2 months | Axillas, groin, abdominal and antecubital crease |
| Pock (2001) | 7 | 4 female3 male | 46-71 | 5 weeks to 15 years | Axillas, groin, pretibial area, wrists, inframammary fold |
The patient was a 32-year-old man, with skin phototype III, and no relevant personal or family history, who attended the clinic because of the spontaneous appearance 3 months earlier of 3 asymptomatic skin lesions on the right axilla. These lesions had been progressively spreading since onset. The patient was not taking any medications and had not been overly exposed to sunlight.
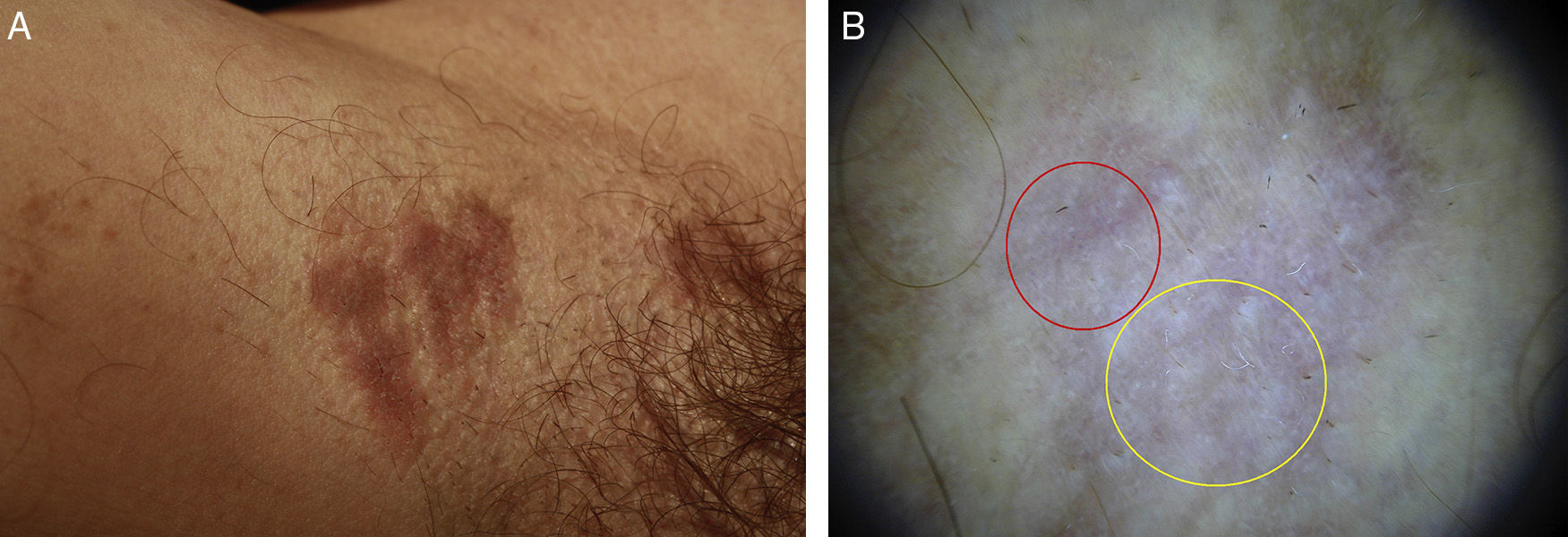
On skin examination, 3 well-defined violaceous-brown plaques were observed (Fig. 1a). Dermoscopy revealed a homogeneous white-bluish pattern with no pigmented reticulum. In several regions, blue-gray and brown-gray globules and dots were observed along with red lines, predominantly at the periphery (Fig. 1b). The lesions were biopsied, and the histologic findings were indicative of lichen planus (Fig. 2). Serology testing for HIV and HCV was negative. Given the absence of symptoms, it was decided not to prescribe treatment. After 12 months of observation, the lesions remained unchanged and no new lesions appeared.
A, Hyperpigmented plaques with a flat surface in the right axilla. B, Dermoscopic image of hyperpigmented plaque in the right axilla. A homogeneous white-bluish pattern (yellow circle) is observed with presence of blue-grayish globules and dots and red lines, predominantly in the periphery (red circle). DermLite II Pro-HR (10x).
LPPI usually affects patients with a low phototype of Caucasian or Asian origin, with no predilection for sex. The age of presentation is usually between 25 and 84 years (mean age, 58 years). The etiology of these lesions is unknown. There is no known causal relationship with medications, exposure to sunlight, HCV infection, or malignant tumors. Pathogenesis appears to be related to the T-lymphocyte-mediated cytotoxicity affecting basal keratinocytes.1
This clinical variant is characterized by the insidious appearance of macules or hyperpigmented plaques of a brown-violet color. The lesions are asymptomatic or mildly itchy and have variable size, well-defined borders, and a smooth surface. Wickham striae may be present. The lesions are located in intertriginous and flexion regions, mainly in the axilla (involved in 90% of the cases), groin, inframammary folds, and popliteal region. Less frequently, they can also appear on the neck and posterior auricular furrow. The condition usually involves several folds, and it is rare for it to affect a single area, as was the case in our patient. Lesions do not appear on mucosa, the scalp, skin appendages, or the palms or soles. In 10% of cases, lesions consistent with lichen planus or lichen planus pigmentosus appear simultaneously in areas outside the flexion folds, and can affect up to 10% of the body surface area.1,2
Histologically, these lesions are characterized by a similar pattern to lichen planus and regression may be observed: orthokeratotic epidermal atrophy (although hyperkeratosis and minimal hypergranulosis can also appear), hydropic degeneration of the basal layer, lichenoid inflammatory infiltrate composed of lymphocytes and histiocytes in the superficial papillary dermis, and areas of pigmentary incontinence and melanophagia.1,2
Dermoscopy is a useful diagnostic tool that provides additional information to the clinical workup of inflammatory diseases. We have only encountered 1 previously published case of dermoscopy in LPPI.3 Dermoscopy of lichen planus has, in contrast, been described and studied previously in the literature.4–10 The most common dermoscopic finding in lichen planus is the presence of whitish striae clinically consistent with Wickham striae. Wickham striae appear in a minority of patients with LPPI, and so whitish striae should be an uncommon dermoscopic finding. Other findings indicative of lichen planus reported previously are yellow-brown dots, blue-gray dots, comedones, corn pearls, milia-like cysts, red globules/dots, and red lines. In our case, 2 dermoscopic findings associated with lichen planus were observed: the blue-grayish and brown-grayish dots/globules, consistent with melanophages in the dermis and the red lines consistent with capillary ectasia in the superficial dermis. The blue-gray and brow-gray dots may be associated with greater persistence of the lesions, greater resistance to treatment, and worse prognosis.4,5,9 The dermoscopic patterns of LPPI show similarities with those of lichen planus but more cases would be needed to compare the findings of the 2 conditions.
Differential diagnosis should be established with erythema dyschromicum perstans, postinflammatory hyperpigmentation, figurate erythema, fixed drug eruption, lichen planus pigmentosus, acanthosis nigricans, contact dermatitis, and candidal intertrigo.1,2
The outcome ranges from spontaneous resolution in a few weeks to persistence for several months or years, with the latter being the most common. The most commonly used treatments are calcineurin inhibitors and medium-potency topical corticosteroids, though success is limited in both cases. Some authors recommend only symptomatic treatment.1,2
We thank Dr. Fernando Burgos Lázaro, Dr. Eva Fernández Cogolludo, Dr. Miguel Ángel Gallego Valdés, and Dr. Antonio Aguilar Martínez for their help.
Please cite this article as: Imbernón-Moya A, Churruca-Grijelmo M, Martínez-Pérez M, Lobato-Berezo A. Dermatoscopia del liquen plano pigmentado inverso. Actas Dermosifiliogr. 2015;106:857–859.

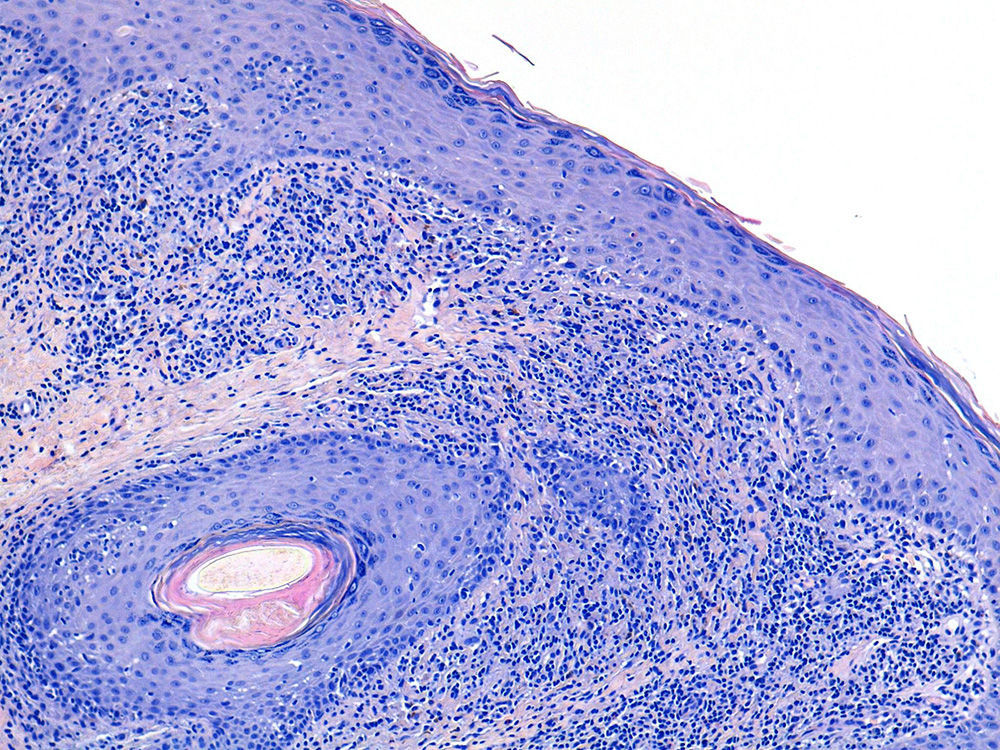
![Hydropic degeneration of the epidermal basal layer, presence of melanophages, and lymphohistiocytic infiltrate in the superficial papillary dermis (hematoxylin-eosin [4x]). Hydropic degeneration of the epidermal basal layer, presence of melanophages, and lymphohistiocytic infiltrate in the superficial papillary dermis (hematoxylin-eosin [4x]).](https://static.elsevier.es/multimedia/15782190/0000010600000010/v1_201512060022/S1578219015002711/v1_201512060022/en/main.assets/thumbnail/gr2.jpeg?xkr=ue/ImdikoIMrsJoerZ+w9/t1/zx4Q/XH5Tma1a/6fSs=)



