Hidrocystomas and hidradenomas are adnexal tumors that originate from sweat glands and are typically of apocrine origin. They are usually diagnosed histologically because they lack characteristic clinical findings.1–5
Dermatoscopy is a noninvasive technique that can help in the diagnosis of these tumors. We present the dermatoscopic features of 3 cases of apocrine hidrocystomas and 1 case of a solid-cystic apocrine hidradenoma.
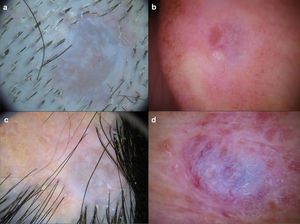
Case 1: A 68-year-old man attended the clinic because of an asymptomatic lesion that had appeared 6 months earlier in the right parietal region (Fig. 1A). The mildly erythematous nodule measured 1cm in diameter. The dermatoscopic image showed a homogeneous pattern of pale grey/bluish color, with whitish cotton wool-like structures and linear irregular vessels (Fig. 2A). Histopathology showed a cystic structure lined by an epithelium formed of a double layer of cuboidal cells with no cytologic atypia and areas of decapitation secretion, consistent with diagnosis of apocrine hidrocystoma (Fig. 3A).
Histologic images (hematoxylin-eosin, original magnification ×20). A and B, Dermal cysts enveloped in a double layer of cuboidal cells. Well-defined tumor composed of cells with abundant eosinophilic cytoplasm and other cells of a more basaloid appearance. C, Cystic structures in the center of the lesion.
Case 2: A 62-year-old woman attended the clinic because of an asymptomatic lesion on the right helix that had been present for several years. The translucent cystic lesion measured 1cm in diameter (Fig. 1B). The dermatoscopic image showed a homogeneous pattern of pale grey/bluish color, with brown-orange regions to the left of the lesion, whitish cotton wool-like structures, and linear irregular vessels (Fig. 2C). Histology was consistent with apocrine hidrocystoma (Fig. 3B).
Case 3: A 30-year-old woman had a 1cm nodule on a sebaceous nevus in the interparietal region (Fig. 1C). The dermatoscopic image showed a homogeneous pattern of pale grey/bluish color, with whitish cotton wool-like structures, and linear irregular vessels (Fig. 2C). Histology confirmed the diagnosis of apocrine hidrocystoma.
Case 4: An 81-year-old woman attended the clinic because of an asymptomatic lesion on the right arm. Clinical examination revealed a well-defined, erythematous nodule measuring 1.5cm in diameter (Fig. 1D). The dermatoscopic image showed a homogeneous pattern of pale grey/bluish color, with brown-orange areas, whitish cotton wool-like structures, and linear irregular vessels peripherally (Fig. 2D). Histologically, the lesion was a nonencapsulated dermal tumor comprised of cells with no atypia and abundant eosinophilic cytoplasm and cells whose nuclei had a more basaloid and hyperchromatic appearance. Foci of clear cells could be seen. The lesion showed cystic formations with mucin in the lumen, as well as a sclerotic and vascularized stroma (Fig. 3C). The above was compatible with a diagnosis of solid-cystic apocrine hidradenoma.
Apocrine hidrocystomas are benign adnexal cystic tumors of unknown etiology. Possible causes include sweat duct occlusion or adenomatous cystic proliferation of apocrine glands (apocrine cystadenoma). Histologically, they usually have multiple cystic spaces, with papillary protrusions and a wall composed of an inner layer of cuboidal cells and an outer layer of myoepithelial cells. These lesions are usually surrounded by a fibrous stroma with small-diameter vessels inside.2,3
Apocrine hidradenoma is a benign adnexal tumor of uncertain histogenesis. It is a multilobed, nonencapsulated, well-defined neoplasm comprised mainly of neoplastic epithelial cells and small ductal lumens. There are several histologic patterns: nodular hidradenoma, solid-cystic hidradenoma, and clear-cell hidradenoma.1,4,5
Correct diagnosis of hidrocystoma and hidradenoma is difficult solely on the clinical presentation and subsequent histologic confirmation is required. The clinical differential diagnosis is very broad and includes conditions such as other adnexal tumors, epidermal cysts, basal cell carcinoma, and amelanocytic melanoma.1–5
Correia et al.6 described the dermatoscopic findings from 2 eccrine hidrocystomas, but they only reported the presence of a well-defined cystic lesion free of vessels. Although not mentioned in the text of the article, a homogeneous pale grey/bluish pattern could be observed in the photograph of one of the cases. There is also a dermatoscopic description of a case of clear-cell hidradenoma, in which the presence of purpuric areas and some linear and hairpin vessels are noted on the tumor surface.7 The purpuric areas correspond histologically to hemorrhage into the cystic spaces of the tumor. In addition, there is a description of a case of malignant nodular hidradenoma, in which polymorphic vascular structures were observed.8 The authors suggested that these can be seen in tumors of eccrine origin.
All of our cases (3 apocrine hidrocystomas and 1 solid-cystic hidradenoma) had a homogeneous pale grey/bluish pattern, whitish cotton wool-like structures, and linear vessels. In 2 cases, focal brown-orange areas were observed. No purpuric areas were observed in any of our cases. The greyish color arises probably because these tumors contain sialomucin, which causes a diffraction effect similar to that observed in Kaposi sarcoma. The whitish cotton wool-like structures are a reflection from the stroma or connective tissue, while the dilated vessels in the superficial dermis correspond to the peripheral linear vessels in the dermatoscopic image. The presence of clear cells laden with glycogen could be responsible for the brown-orange focal structures. In conclusion, we should suspect these tumors in the case of nodular lesions, particularly on the head. Dermatoscopy is a technique that can help in diagnosis, particularly in the absence of dermatoscopic findings suggestive of other clinically similar tumors such as basal cell carcinoma and amelanotic melanoma.
Please cite this article as: Cieza-Díaz D, Avilés-Izquierdo J, Ciudad-Blanco C, Parra-Blanco V. Dermatoscopia de tumores apocrinos: presentación de 4 casos. Actas Dermosifiliogr. 2013;104:826–828.