Langerhans cell histiocytosis (LCH) is a disease of clonal proliferation of immature Langerhans cells.1,2 LCH can affect any organ,3 occurs mainly in children, and is rare in adults. It is even rarer for it to be confined to the skin. We present 3 cases of adult-onset cutaneous LCH treated by surgical excision. No new lesions or systemic or other effects developed during follow-up.
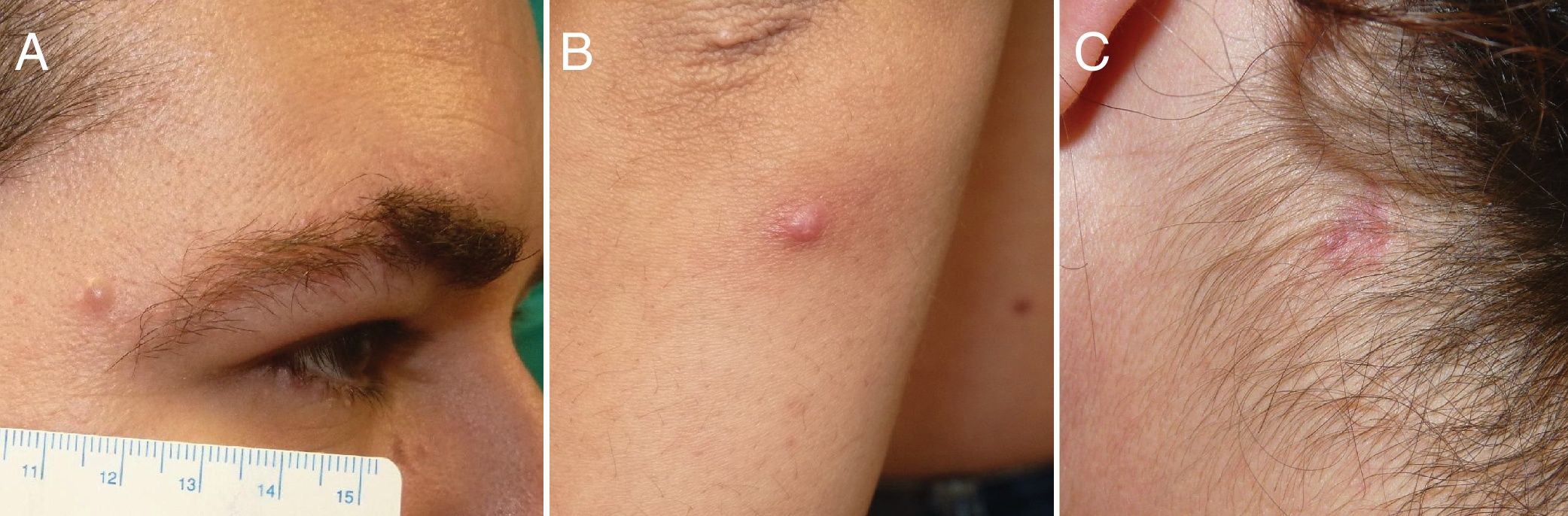
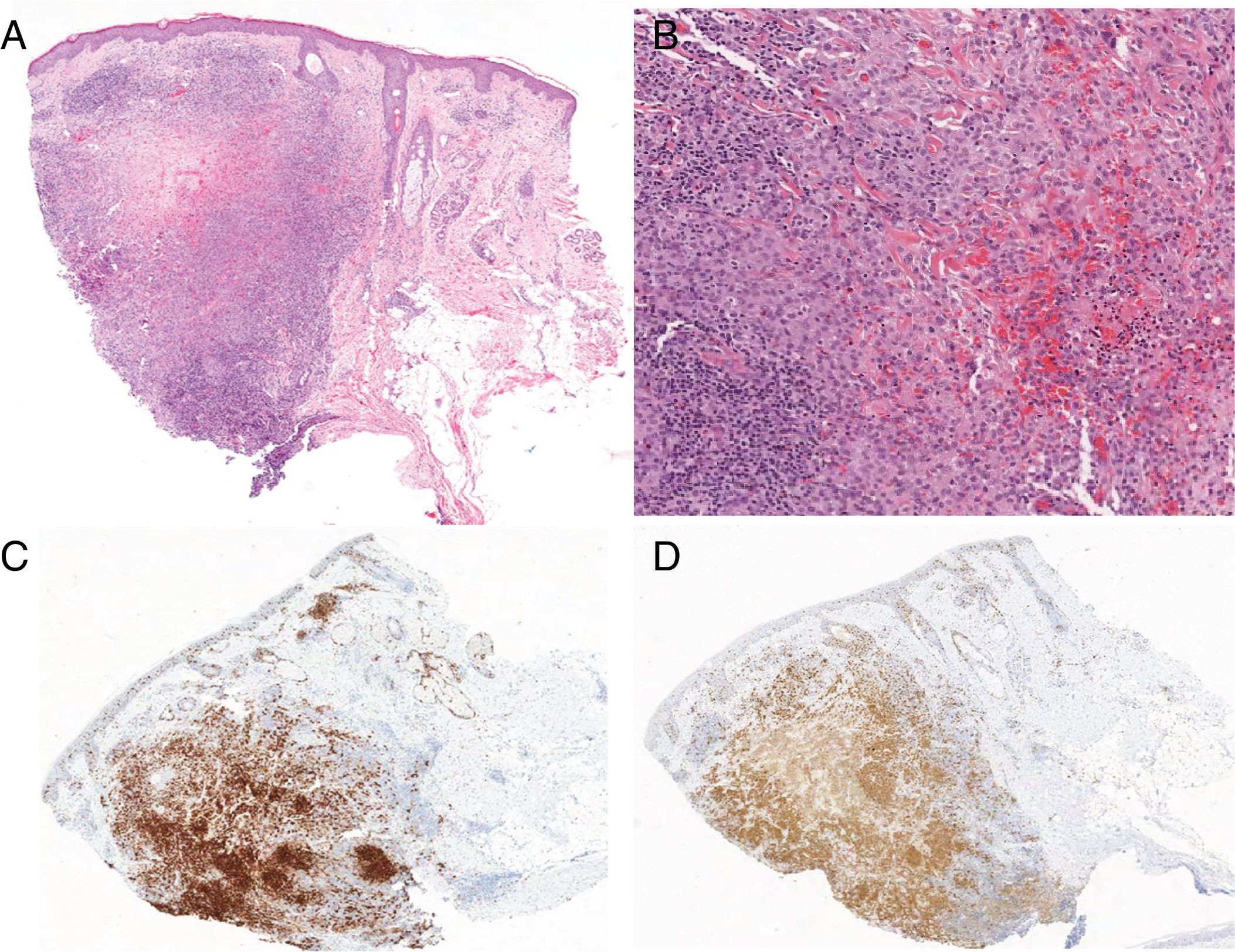
Case 1: A 36-year-old man with no relevant medical history presented with an asymptomatic lesion that had appeared 2 months earlier. It was located on the external edge of the right eyebrow, and there were no associated symptoms. Physical examination showed it to be a papule 6mm in diameter that was slightly erythematous, firm to the touch, and well defined (Fig. 1A). No other skin or mucosal lesions, palpable lymph nodes, or enlarged organs were detected. Histopathology of the excised tissue revealed a normal epidermis and a dense, nodular-type infiltrate (Fig. 2A) composed of dispersed cells with oval or kidney-shaped nuclei resembling coffee beans (Fig. 2B). The cells had a clear eosinophilic cytoplasm, corresponding to histiocytes. The infiltrate also contained necrotic areas, lymphocytes, and eosinophils. The mitotic index was very low. Immunohistochemical staining was positive for S100, CD1a (Fig. 2C and 2D) and CD207 (langerin) and negative for CD68. With these findings we made the diagnosis of LCH and ordered the following additional tests and imaging studies: complete blood count, coagulation screen, biochemistry, hormone profile, urine analysis, chest radiograph, abdominal ultrasound, and bone scans. All findings were normal. The final diagnosis was adult-onset LCH confined to the skin. The patient has remained asymptomatic for 3 years. No new skin lesions, systemic symptoms, or related disorders have developed.
A, Dense, nodular-type infiltrate in the dermis, with areas of necrosis; hematoxylin-eosin, magnification ×10). B, Histiocytes with oval or kidney-shaped nuclei resembling coffee beans and clear cytoplasm; accompanied by lymphocytes and eosinophils (hematoxylin-eosin, magnification ×20). C and D, immunohistochemical staining was positive for S100 and CD1a, respectively.
Case 2: A 33-year-old woman reported that an asymptomatic lesion had appeared on her left forearm 6 months earlier. It was an erythematous, infiltrated papule 5mm in diameter (Fig. 1B). No enlarged lymph nodes or organs were found on physical examination. The lesion was removed, and the histopathologic findings, similar to those described in the first case, were consistent with a diagnosis of LCH. The results of additional tests were negative, and no new lesions or other clinical or analytic abnormalities have appeared in 2 years of follow-up.
Case 3: A 49-year-old woman presented with 2 erythematous, papular lesions 5and 7mm in diameter located on her right cheek and back. She also had a 9-mm plaque on the left side of her neck (Fig. 1C). No abnormalities were found on physical examination. Histopathology of an excised lesion was consistent with LCH, and so the remaining two were also removed. The histologic findings were the same. Additional studies gave no positive results. No new lesions or new conditions have developed in 3 years of follow-up.
LCH is a rare disease that is diagnosed mainly in children under the age of 15 years. Over that age, the estimated incidence is 5to 9cases per million population.1,4 The spectrum of clinical presentations ranges widely,3–6 varying according to the organ affected. In some cases lesions are solitary and resolve on their own, whereas in others the disease is disseminated and life-threatening.3,4,6,10 The recent classification system of the Histiocyte Society refers specifically to a Langerhans (L) group of diseases.4 Diagnosis is based on clinical, radiologic, and histopathologic findings, the last of which identifies a histiocytic infiltrate with the characteristic immunophenotypic features of LCH. The disease can affect any organ but is mainly found in bones, skin, hypophysis, liver, spleen, lymph glands, and lungs; less often, the central nervous (other than at the hypophysis) and hematopoietic systems are involved.3,4
The pathogenesis of LCH remains unclear.3,4,6,7 The BRAF V600E mutation, which overstimulates the MAPK pathway, is present in half of patients with LCH. Smaller proportions of patients carry the MAP2K1 MEK1 or MAP3K1 ARF mutations. Mutations in the PICK1 and PICK3R2 genes, affecting the PIK3CA pathway, have also been described.4 These findings support the theory that LCH is a neoplastic process.3,4 However, the inflammatory component and the fact that the clinical course is sometimes benign suggest a reactive process. Cases of familial LCH have been reported, though no genetic predisposition has yet been identified.4
Adult-onset LCH confined to the skin is very rare.1,5,8 This form may present as a solitary papular or nodular lesion, with or without ulceration, or as multiple lesions.1,9 It may even mimic other skin diseases.10 In a series of 18 patients who presented with cutaneous lesions, the ages ranged from 20 to 89 years and no pattern related to race or gender was identified.1 Nearly half (8/18) had solitary lesions (papules or nodules) or ulcerated lesions in skin folds. On further study, bone involvement was found in 1 of these patients and myelodysplastic syndrome was diagnosed in 2 of them. During a mean follow-up period of 41 months, 2 patients developed noncutaneous LCH and 5 patients were diagnosed with progressing blood tumors (2 cases of myelomonocytic leukemia and 1 case each of histiocytic sarcoma, diffuse large B-cell lymphoma, and peripheral T-cell lymphoma). The authors of that series also reviewed the literature, finding 74 patients with initial presentations involving the skin, 4 of whom had extended histiocytosis and 8 of whom had blood diseases found during diagnosis or follow-up. The authors suggested that the association between LCH and myelomonocytic disorders could be related to the common origin of the cells in bone marrow.1 LCH is currently thought to arise in myeloid dendritic cells of the bone marrow, which express the same antigens as cutaneous Langerhans cells.
The differential diagnosis of LCH includes several neoplastic and inflammatory diseases.10 Knowledge of the lesions’ immunophenotype is therefore essential for a firm diagnosis. Histology must demonstrate an infiltrate of Langerhans cells positive for CD1a and/or CD207 (langerin),3,6 a criterion that has replaced the finding of Birbeck granules by electron microscopy.6 Positive staining for CD207 rules out indeterminate cell histiocytosis.4
Searching for possible extension of disease to other tissues and follow-up are essential when treating adults with skin lesions to rule out LCH in other locations and concurrent conditions.1,6 Findings will be mainly blood disorders, such as typically occur in children. Tests and imaging studies recommended for adults with LCH include a complete blood count, biochemistry, chest radiograph, hormone profile, bone scans, and abdominal ultrasound; these studies are ordered at baseline and every 6 months during follow-up for asymptomatic patients.1,3 A full physical examination, complete blood count and biochemistry, and abdominal ultrasound as well as a chest radiograph are usually ordered annually for at least 3 years.3 Bone marrow should be biopsied if infiltration is suspected, although some authors believe the procedure should be routine.1
Because LCH in the adult is so rare, optimum treatment has not been established. The prognosis is good for patients with LCH confined to a single organ or system,3,6 but they should be followed closely.3,10 Local treatments (surgery, topical corticosteroids, or corticosteroid infiltrations) can be used. Multiple, ulcerated, or resistant lesions can be treated with systemic corticosteroids, phototherapy, radiotherapy, interferon, and various chemotherapeutic regimens.6,9 It has been suggested that ulceration may affect the prognosis, although to date the reported outcomes have been inconsistent.1
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Drs Juan Luis Santiago Sánchez-Mateos and Claudia Ramos-Rodríguez collaborated in preparing this report.
Please cite this article as: Flores-Terry MA, Sanz-Trenado JL, García-Arpa M, Cortina-de la Calle MP. Cutaneous Langerhans Cell Histiocytosis Presenting in Adulthood. Actas Dermosifiliogr.2019;110:167–169.