Endometriosis is a gynecological condition characterized by glands and/or endometrial stroma located outside the uterine cavity; it affects approximately 10% of women of reproductive age.1 It mostly occurs in the pelvic cavity, but can also affect extragenital locations, including the skin.1
Umbilical endometriosis accounts for less than 1% of all cases of extragenital endometriosis.2,3 The umbilicus is the most common site for cutaneous endometriosis (40% of all cases).
Case ReportA 29-year-old nulliparous women, a current smoker, presented with umbilical lesions of 2 years’ duration. The lesions were not painful, but she described cyclic bleeding during menstruation. She denied dysmenorrhea, dyspareunia, and infertility, and there was no history of abdominal surgery.
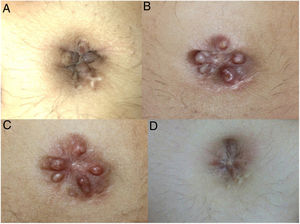
Physical examination revealed several reddish-brown lesions that were nonreducible and painless on palpation (Fig. 1A).
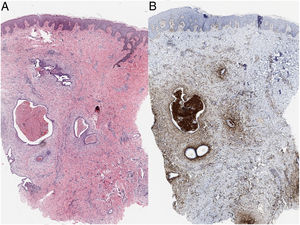
Histologic examination of a biopsy specimen showed endometrial glands lined by a pseudostratified cylindrical epithelium and extravasated red blood cells (Fig. 2A). Immunohistochemical staining was positive for CD10, confirming the presence of ectopic endometrial stroma4 (Fig. 2B).
Subsequent gynecological evaluation including ultrasound and cervical cytology ruled out genital disease.
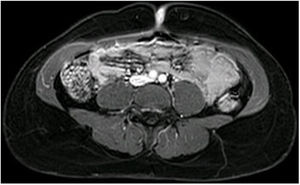
The patient also underwent abdominal magnetic resonance imaging (MRI), which revealed a well-defined oval skin lesion showing intense contrast uptake in the umbilical region. The lesion was touching but did not invade the underlying abdominal muscles (Fig. 3). No other foci of endometriosis were observed.
Surgical excision was considered during follow-up, but the patient became pregnant and the surgery was postponed. The lesions remained stable during pregnancy and resolved spontaneously several days after delivery (Fig. 1B–D). No recurrences or new lesions have occurred during 2 years of follow-up.
DiscussionUmbilical endometriosis accounts for between 0.4% and 4% of all endometriosis cases.5 Secondary umbilical endometriosis is more common than primary umbilical endometriosis and is associated with surgical scars following abdominal surgery. Patients with the primary form of this disease do not have a prior surgical history.
Umbilical endometriosis usually affects women in their third decade of life and typically presents as an asymptomatic or painful red-violaceous nodule that exhibits cyclic bleeding during menstruation.
A tentative diagnosis is usually based on clinical findings and confirmed by histology. Apart from endometrial glands and stroma, histology may also show hemosiderin deposits, inflammatory changes, and marked mitotic activity. Immunostaining with CD10, which is positive in the endometrial interstitium, is useful when glands are not seen on histology.4
The differential diagnosis should include cutaneous metastases, melanoma, seborrheic keratosis, pyogenic granuloma, and keloids.
Imaging tests such as ultrasound, computed tomography, and MRI are useful for ruling out involvement of other organs and establishing lesion depth.6
Surgical excision is the treatment of choice. Hormone therapy can be used in patients with systemic disease or before surgery to try to reduce the size of lesions.
In relation to the effect of pregnancy on umbilical endometriosis, Razzi et al.7 published the case of a woman whose lesions resolved spontaneously 2 months after biopsy, at 24 weeks’ gestation. Wiegratz et al.,8 by contrast, described a patient with a 2-year history of primary umbilical endometriosis whose nodules enlarged progressively during pregnancy and whose bleeding changed from cyclic to continuous. The woman underwent surgery before the pregnancy reached full term. Our patient's lesions remained stable during pregnancy, although they protruded more as the belly grew. The bleeding stopped during pregnancy and the lesions resolved spontaneously several days after delivery.
Pregnancy has conventionally been believed to have a beneficial effect on endometriosis, and some patients have even been advised to become pregnant as part of their treatment plan. In a recent review, however, Leeners et al.9 concluded that there was insufficient evidence to expect pregnancy to reduce the number or size of endometriosis lesions.
There is also insufficient evidence to predict the effects of pregnancy on umbilical endometriosis based on the 3 cases described to date.
We have described, to our knowledge, the third case of umbilical endometriosis in a pregnant woman. The patient's lesions remained stable during pregnancy and resolved spontaneously after birth. More cases are required to determine the effects of pregnancy on umbilical endometriosis.
Conflicts of InterestThe authors declare that they have no conflicts of interest.