Histological diagnosis of a clinically suspected nonmelanoma skin cancer (NMSC) is recommended before treatment. For NMSC, concordance between the histological subtype of the preoperative biopsy and the excision specimen of basal cell carcinoma (BCC) has been reported to range from 10% to 81%. No large study on the concordance between NMSC histology seen in a preoperative biopsy with the following tumour specimen from Mohs micrographic surgery (MMS) has been performed in a Latin American population.
ObjectiveThe aim of this study was to analyse and compare the histological subtype of the incisional biopsies reviewed by the dermatopathologist with the histological subtype of the tumour specimen obtained during MMS interpreted by the dermatopathologist and the Mohs surgeon.
MethodsA retrospective analysis of 320 NMSC was performed. The interobserver correlation was based on kappa values.
ResultsThe mean weighted kappa value between the preoperative NMSC biopsy and intraoperative histological subtype of the tumour specimen from MMS analysed by the Mohs surgeon and the dermatopathologist was 0.22 and 0.24, respectively. The correlation in the histologic subtype of the intraoperative tumour specimen from MMS that was interpreted by the dermatopathologist and Mohs surgeon was 0.58.
ConclusionsDermatologists need to be aware of the limited value of incisional biopsies to accurately diagnose the histological subtype of a NMSC. The concordance rate in the histological diagnosis of the tumour specimens that were obtained from MMS between the Mohs surgeon and the dermatopathologist is moderate. However, the correlation is low compared with incisional biopsy subtypes.
Se recomienda diagnosticar histológicamente el cáncer cutáneo no melanoma clínicamente sospechado (CCNM) antes de iniciar el tratamiento. Para el CCNM, se ha reportado una concordancia entre el subtipo histológico de la biopsia preoperatoria y la muestra extirpada del carcinoma de células basales (CCB), que oscila entre el 10 y el 81%. No se han llevado a cabo grandes estudios sobre la concordancia entre la histología del CCNM apreciada en la biopsia preoperatoria y la siguiente muestra tumoral obtenida de la cirugía micrográfica de Mohs (MMS) en la población latinoamericana.
ObjetivoEl objetivo de este estudio fue analizar y comparar el subtipo histológico de las biopsias incisionales revisadas por el dermato-patólogo, con el subtipo histológico de la muestra tumoral obtenida durante la MMS, interpretada por el dermato-patólogo y el cirujano.
MétodosSe realizó un análisis retrospectivo de 320 CCNM. La correlación inter-observador se basó en los valores kappa.
ResultadosEl valor medio ponderado kappa entre la biopsia preoperatoria del CCNM y el subtipo histológico intraoperatorio de la muestra tumoral obtenida de la MMS, analizadas por el cirujano y el dermato-patólogo, fue de 0,22 y 0,24, respectivamente. La correlación en el subtipo histológico de la muestra tumoral intraoperatoria para MMS, interpretada por el dermo-patólogo y el cirujano, fue de 0,58.
ConclusionesLos dermatólogos deben ser conscientes del valor limitado de las biopsias incisionales para diagnosticar de manera precisa el subtipo histológico del CCNM. La tasa de concordancia del diagnóstico histológico de las muestras tumorales obtenidas durante la MMS, entre el cirujano y el dermato-patólogo, fue moderada. Sin embargo, la correlación es baja cuando se compara con los subtipos obtenidos de la biopsia incisional.
Mohs micrographic surgery (MMS) is a surgical treatment for locally invasive malignant cutaneous tumours that minimizes the removal of unaffected tissue. It provides a cure rate close to 99% for primary basal cell carcinoma (CBC) and 97% for squamous cell carcinoma (SCC).1
In MMS, the margins are effectively delineated as the tumour is surgically removed in successive stages. Tumour extensions are pursued until complete excision of the lesion is accomplished by histologic examination of the three-dimensional border of the excised tissue. This allows identification of the location of the residual tumour for subsequent removal.2,3 The advantages of MMS are more precise histologic control, higher cure rates, and maximal preservation of healthy tissue.3
Prior to treatment, punch and shave biopsies have been proposed to confirm the clinical diagnosis of NMSC and to determine the histopathological subtype.4 The histological subtype identified by the biopsy is an important determinant of treatment choice.
The success rate of MMS depends on an accurate microscopic evaluation of the specimens. The MMS surgeon does the histopathologic review and is able to translate abnormal findings into appropriate sequential tumour removal. However, there is great variability in the literature regarding the percentage of concordance between the histologic diagnosis of incisional biopsies and the histologic diagnosis that is found with complete tumour excision. Previous studies have shown a moderate agreement ranging from 51.1% to 82% between NMSC subtype on incisional biopsies and subsequent surgical excision.4–7
The aim of this study was to analyse and compare the histological subtype of the incisional biopsies issued by the dermatopathologist with the histological subtype of the tumour specimens obtained through MMS interpreted by the dermatopathologist and the Mohs surgeon.
Materials and methodsIn this retrospective study, we analysed the agreement between histological NMSC subtype from an incisional biopsy and the subsequent MMS excision. Patients of all ages attending the Department of Dermatology at the Dr. José Eleuterio Gonzalez University Hospital in Monterrey, Mexico from November 1988 to November 2015 and who underwent both an incisional biopsy and a subsequent MMS of a histologically proven NMSC were eligible. This project was granted an exemption by our Human Research Committee (number DE 15-008). Demographical and histological data of the preoperative biopsies were retrieved from the medical records. We excluded cases with incomplete medical records and those with damaged or missing Mohs histologic slides. Incisional biopsies were obtained in all NMSC from the area that was most clinically suspected of thick and infiltrative growth through a biopsy punch. The histological subtype reported by a dermatopathologist in the medical records was considered as the incisional biopsy subtype; subsequently, MMS was performed under local anaesthesia.
Data were collected, and the following characteristics were registered: gender, age, tumour location, histological subtype from incisional biopsy and MMS, and the number of stages and sections. The histological subtype of NMSC from the excisional Mohs specimen was independently reviewed by a dermatopathologist and a Mohs surgeon according to defined standard histopathogical features. Both specialists re-examined all histologic tumour layers (“debulking layers” obtained by scalpel excision of the tumour site) to establish an intraoperative diagnosis. For “debulking” layers showing no residual tumour, subsequent Mohs layers were examined. For tumours showing more than one histological subtype, the most aggressive tumour was assumed to be the definite histological subtype of the tumour. An initial agreement between histologic diagnoses on incisional biopsy specimens and histologic diagnoses on subsequent Mohs excision specimens diagnosed by the Mohs surgeon was performed.
The subtypes of all tumours were identified by standard histopathologic characteristics and subsequently classified into BCCs with superficial, nodular, aggressive (micronodular, infiltrative/morpheaform and metaatypical) or other subtypes (adenoid, cystic, pigmented, nodulocystic, keratotic) according to a treatment based classification used in previous studies.4,6 SCC were classified into poor, moderately or well differentiated (Table 1).
A correlation between the preoperative pathology report and the histologic tumour specimen diagnosis established by the Mohs surgeon and the dermatopathologist was made.
Statistical analysisDescriptive results are given as numbers and percentages. Proportions with concordant results were calculated as the proportion of tumours with the same diagnosis in punch biopsy and Mohs excision specimens. The correlation between groups was calculated using Cohen's kappa coefficient. Complete agreement was considered to be a kappa score of 1. Kappa values <0 indicate no agreement and 0–0.20 indicate slight agreement, 0.21–0.40 are interpreted as fair, 0.41–0.60 as moderate, 0.61–0.80 as substantial, and 0.81–1 as almost perfect agreement. Statistical significance for all results was 0.05. Data analyses were performed with IBM SPSS version 20.0 (SPSS, Inc, Armon, NY). The concordance rate was calculated for the preoperative histologic subtype and the diagnosis established by the Mohs surgeon and the dermatopathologist together; for the preoperative incisional biopsy subtype, the concordance rate was calculated with the diagnosis established by the dermatopathologist and the Mohs surgeon separately. A correlation was also calculated for the histologic subtype of the “debulking layers” between the diagnosis given by the dermatopathologist and the Mohs surgeon.
ResultsA total of 546 NMSC were treated with MMS. We included and analysed 320 NMSC and 226 were excluded because of incomplete medical record data.
The average age of the patients was 64.79 years (range 6–94), of these, 159 (49.69%) corresponded to women and 161 (50.31%) to men. The 6-year-old patient was diagnosed by preoperative and Mohs histology with moderately differentiated SCC. The most frequent location of the tumours was the nose in 143 cases (44.68%), followed by the cheeks in 62 cases (19.38%). The least frequent location was the chin in 1 case (0.31%) (Table 2). Recurrent tumours comprised 15.06% (33 cases) and primary tumours 84.93% (186 cases). The remaining cases (101) lacked this information on medical records.
The most frequent subtypes of NMSC found on incisional biopsy were aggressive and nodular BCCs, followed by moderately differentiated SCC (Table 3). Aggressive and nodular BCCs showed the highest percentage of correlation between the preoperative histological subtype and the MMS specimen subtype read by the Mohs surgeon (Table 4).
Distribution of NMSC cases on incisional biopsy by histological subtype.
| Histological subtype | Number of cases | % |
|---|---|---|
| Well differentiated SCC | 9 | 2.8 |
| Moderately differentiated SCC | 17 | 5.3 |
| Poorly differentiated SCC | 2 | 0.6 |
| Aggressive BCC | 233 | 72.8 |
| Nodular BCC | 33 | 10.3 |
| Adenoid BCC | 8 | 2.5 |
| Superficial BCC | 15 | 4.7 |
| Other types of BCC | 1 | 0.3 |
| DFSP | 2 | 0.6 |
| Total | 320 | 100 |
Aggressive BCC comprised the variants: micronodular, infiltrant/morpheaform and metaatypical.
Summary of diagnoses from tumour layer examination during Mohs micrographic surgery diagnosed by Mohs surgeon and preoperative biopsy diagnosis.
| Tumour diagnosis by Mohs surgeon obtained during Mohs surgery | Concordant with preoperative biopsy diagnosis | Total cases of tumour diagnosis by Mohs surgeon obtained during Mohs surgery |
|---|---|---|
| Superficial BCC | 1 (0.3) | 4 (1.25) |
| Nodular BCC | 11 (3.43) | 84 (26.25) |
| Aggresive BCC | 127 (39.69) | 167 (52.19) |
| Other types of BCC | 2 (0.6) | 16 (5) |
| SCC | 16 (5) | 22 (6.86) |
| DFSP | 2 (0.6) | 3 (0.94) |
| No tumour found | 24 (7.5) | |
| Total | 320 (100) | |
Data are given as numbers and (percentages).
Concordance between the preoperative biopsy and intraoperative histological subtypes of NMSC by the Mohs surgeon was fair (kappa=0.22). This value was slightly lower than the intraoperative subtype established by the dermatopathologist (kappa=0.24). Moderate concordance (kappa=0.58) was found between the histologic subtypes for the intraoperative specimen interpreted by both the dermatopathologist and the Mohs surgeon.
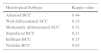
Fair to substantial correlation was calculated between the preoperative biopsy subtype and the histologic subtype defined by both the Mohs surgeon and the dermatopathologist (Table 5). The highest correlation corresponded to moderately differentiated SCC (kappa=0.75), followed by well-differentiated SCC (kappa=0.57). The histological BCC subtype that showed the highest correlation between the biopsy and intraoperative subtype defined by both specialists corresponded to the infiltrative variant (kappa=0.55) (Table 5). The concordance for histologic subtype between the preoperative biopsy and intraoperative Mohs surgeon diagnoses was highest for adenoid BCC (kappa=0.44, Table 6).
Correlation between the preoperative biopsy subtype and the histologic defined by both a Mohs surgeon and a pathologist.
| Histological subtype | Kappa value |
|---|---|
| Moderately differentiated SCC | 0.75 |
| Well differentiated SCC | 0.57 |
| Infiltrant BCC | 0.55 |
| Nodular BCC | 0.47 |
| Adenoid BCC | 0.47 |
| Superficial BCC | 0.42 |
| Basosquamous carcinoma | 0.37 |
| Poorly differentiated SCC | 0.33 |
In most cases, there was a low concordance between the initial NMSC diagnosis and the final Mohs tumour layer diagnosis for both the dermatopathologist and the Mohs surgeon. This concordance appears to be lower than the agreement percentages reported by similar studies. Haws et al.6 found a histological concordance of 81% between punch and shave biopsies and their subsequent excision with margins. In a more recent study, Roozeboom et al.4 found a lower percentage of agreement (60.9%) between BCC subtype on a punch biopsy and the subsequent subtype of the whole lesion. Izikson et al.5 compared the biopsy diagnosis and the Mohs “debulking” slides in 513 cases of primary NMSC and found concordance in 51.1% of aggressive and nonaggressive tumour subtypes. Another study of Mohs resection of BCCs reported a lower accuracy rate of 10% on biopsy specimens, which was considered to be a result of the lack of specification of BCC subtypes in the pathology report.8 A study showed an agreement of 67.1% between histological BCC subtype on a punch biopsy and subsequent excision specimens in recurrent BCC.4
Some of the previous studies grouped excisional biopsies in aggressive and non-aggressive subtypes; in contrast to our study where we compared individual NMSC subtypes, these studies could report higher concordance values. In most reports, excisional histological specimens were obtained through standard excision; only our study and one previous study5 compared preoperative specimens with tumour specimens obtained through Mohs surgery.
Small sampling biopsies in large tumours could contribute to show a discrepancy between the incisional biopsy and the intraoperative Mohs diagnosis. Additionally, the selection of a determined site for an incisional biopsy does not exclude the presence of a mixed subtype on the same lesion. Preoperative biopsies could also coincide with the site of a scar or an area that was previously treated, failing to establish an accurate diagnosis. Furthermore, pathologists may use different criteria to diagnose histological subtypes, reporting only the predominant subtype or reporting a limited number of subtypes on incisional biopsies. A limitation in our study consists of the lack of evaluation of incisional biopsy slides by the Mohs surgeon and the re-evaluation by the dermatopathologist. However, a moderate concordance was found for the intraoperative histological subtype diagnosis that was obtained through MMS between the dermatopathologist and the Mohs surgeon. Moreover, the highest concordance rate for each subtype in incisional biopsies and excisional Mohs specimens by both specialists corresponded to SCC subtypes, most likely because of the smaller number of subtypes defined for this variant of NMSC.
In summary, a biopsy reported by a general pathologist or dermatopathologist is not capable, according to our study, of providing adequate sampling for NMSC subtyping. The scenarios that could explain these results are a lack of specification of NMSC subtypes in biopsy samples, the use of different diagnostic criteria by general pathologists to determine histological subtyping in this group of skin cancers, and sampling variations on preoperative biopsies that could lead to a different interpretation of the histological subtype. This study supports that two or more histological subtypes of NMSC could coexist on the same lesion, and this could impact the therapeutic approach and prognosis of this type of tumour. A variable that could influence the concordance between preoperative and operative histological specimen subtypes is tumour size, since a larger tumour could comprise diverse NMSC subtypes. This may be studied as factor altering concordance in further studies. It is advisable for the dermatologist to review the incisional biopsy histology to corroborate the pathology report before deciding the best therapeutic approach.
In conclusion, the detection of intraoperative subtypes during MMS leads to a higher probability of detecting the presence or persistence of aggressive tumour subtypes at the margins, leading to a higher cure rate. Accurate knowledge of the histological subtypes leads to the selection of the appropriate treatment modality. The relatively recent implementation of this type of surgery in our country and the lack of higher concordance rates between histological interpretations prompts the standardization of histology training in centres where dermatologic surgery, and moreover, MMS is performed.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Conflict of interestThe authors declare no conflict of interest.