Cold Urticaria (ColdU) is a type of chronic inducible urticaria (CIndU) where recurrent pruritic wheals and/or angioedema occur after exposure to cold stimulus. Although it usually only affects exposed areas, systemic reactions can occur in severe cases. In this study, we seek to characterize the ColdU cases within our Centre's population of patients.
Material and methodsRetrospective study based on clinical files of patients diagnosed with ColdU followed in an urticaria outpatient clinic in Portugal prior to October 2020.
ResultsWe included 52 patients total (40 women) with median age of 35 years, 19 patients with symptom onset before 18 years-old. ColdU was classified as acquired in all patients. Cold provocation tests were negative in 9 patients and these were classified as atypical ColdU. No significant differences were found between those with pediatric or adult onset of disease. Most of the patients had a localized form of the disease (52%). Despite not being statistically significant, it was found that patient's temperature threshold, assessed with TempTest® 4.0, was higher and stimulation time was shorter in more severe groups. All patients were treated with non-sedating antihistamines (daily or on-demand), finding that those controlled with standard dosages had lower temperature thresholds than those needing higher dosages (p < 0.01). One patient was under treatment with omalizumab.
ConclusionColdU is an heterogenous disease that can have life-threatening event consequences. Cold provocation tests and threshold assessment can be an important tool in the management treatment and in identifying severity groups.
La urticaria por frío (UF) es un tipo de urticaria crónica inducible (CIndU) donde aparecen ronchas pruriginosas recurrentes y/o angioedema tras la exposición a estímulos fríos. Aunque normalmente solo afecta a áreas expuestas, pueden producirse reacciones sistémicas. Nuestro objetivo es caracterizar los casos de UF de nuestro hospital.
Material y métodosEstudio retrospectivo de casos de UF seguidos en nuestra consulta de urticaria en Portugal hasta octubre de 2020.
ResultadosSe incluyeron 52 pacientes, de ellos 40 mujeres. La edad media fue de 35 años. En 19 pacientes, los síntomas comenzaron antes de los 18 años de edad. La UF se clasificó como adquirida en todos los pacientes. Las pruebas de provocación por frío fueron negativas en 9 pacientes, clasificados como UF atípica. No se encontraron diferencias con respecto al inicio en edad pediátrica o adulta. Más de la mitad de los pacientes (52%) tenían una UF localizada. A pesar de no ser estadísticamente significativa, la temperatura umbral evaluada con TempTest® 4.0 fue más alta y el tiempo de estimulación más corto en los pacientes con síntomas más graves. Todos los pacientes fueron tratados con antihistamínicos y uno con omalizumab. Los pacientes controlados con dosis estándar de antihistamínicos tenían temperatura umbral más baja que los que necesitaban dosis más altas (p < 0,01).
ConclusiónLa UF es una enfermedad heterogénea que, en algunos casos, puede poner en peligro la vida del paciente. Las pruebas de provocación con frío pueden ser útiles en el manejo e identificación de grupos de gravedad.
Chronic inducible urticaria (CIndU) is a subgroup of chronic urticaria (CU) where recurrent pruritic wheals and/or angioedema occur after exposure to specific stimuli.1–3 Cold urticaria (ColdU) is one of the most common types of CIndU (5–33%) where symptoms develop after exposure to air, surfaces or water which are colder than body temperature.4–6 ColdU often develops in young adults, and women show a slightly higher prevalence.3,7 Although symptoms are usually localized in cold-exposed areas, in severe cases or in those with extensive cold contact more severe manifestations can result. These can vary from generalized urticarial symptoms to systemic reactions affecting respiratory, gastrointestinal or even cardiovascular system with hypotension and loss of consciousness.6,8 Some studies report up to 20% of cases featuring severe life-threatening reactions.8,9
ColdU can be classified as acquired or familial. According to etiology, ColdU is further classified as primary when there are no underlying identifiable causes, and secondary if there is a known underlying disease. Primary acquired ColdU is the most common form. Secondary acquired ColdU is very rare form and most commonly associated with cryoglobulinemia.1 ColdU can be classified as atypical if there is if there is a positive clinical history but no response to standard CST.1,9
Diagnosis of ColdU is based on clinical history and verified by cold stimulation tests (CST). These are performed through application of a cold stimulus (ice cubes, cool packs, cold water baths, or TempTest®) to the forearm.3,4,10
Treatment consists of cold avoidance and management with antihistamines. For those refractory to antihistamines, omalizumab is recommended – although it has not been approved yet for this indication, there were positive results in some trials.8,11
Materials and methodsPopulation and study designA retrospective study has been undertaken of patients diagnosed with ColdU referred to an urticaria outpatient clinic from 2007 to 2020. Data was collected from clinical charts. Patients were characterized according to demographics, comorbidities (atopic disease, other types of CU, neoplastic and autoimmune disease), family history, severity of symptoms, physical tests results and treatment regimens.
Diagnostic criteriaDiagnosis of ColdU was based on clinical history of development of wheals, angioedema, or anaphylaxis after cold exposure. Patients were evaluated according to age at onset of symptoms and according to disease severity. Symptoms were classified as: I – localized (urticaria and/or angioedema only in sites in contact with cold stimulus), II – generalized (generalized urticaria and/or angioedema after full body exposure or generalized urticaria after located exposure) and III – systemic (with respiratory and/or cardiovascular compromise).
Cold provocation tests were performed to confirm ColdU: ice cube test and TempTest®4.0 (Moxie, Berlin, Germany). The ice cube test was performed by placing an ice cube wrapped within a thin plastic bag in contact with the patient’s forearm for 5 min and considered positive if wheals developed after 10 min. The TempTest® provides a continuous temperature gradient along its length (from 4 to 44 °C), allowing the identification of temperature and stimulation time thresholds. Cold stimulation time threshold (CsTT) is the shortest duration of cold exposure sufficient to induce a positive test reaction and is determined by varying the time of cold application it takes to induce a wheal and flare-type skin response. The cold temperature threshold (CTT) is the highest temperature sufficient to induce a positive test reaction.
Statistical analysisStatistical analysis was performed using GraphPad Prism® 9.0.0. Descriptive statistics were performed for each variable, categorical variables were presented in frequencies and continuous variables were presented in median and interquartile range (IQR). Comparison between groups was made using the Chi-square or Fischer exact test for categorical and Mann–Whitney U or Kruskal–Wallis H tests for continuous variables. A p-value ≤0.05 was considered statistically significant.
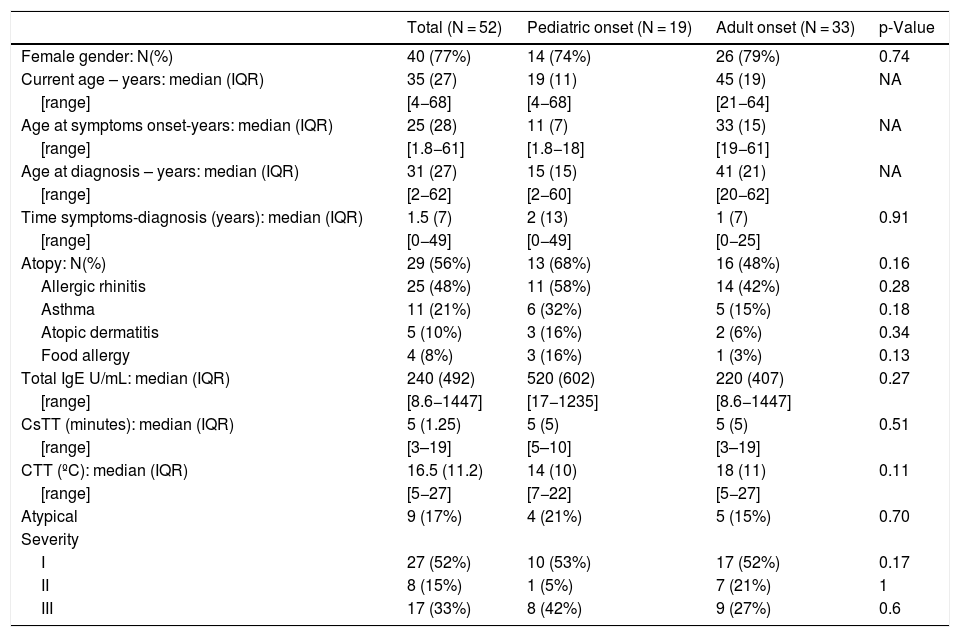
ResultsPatients’ characteristicsPatients’ characteristics are summarized in Table 1.
Patients characteristics.
| Total (N = 52) | Pediatric onset (N = 19) | Adult onset (N = 33) | p-Value | |
|---|---|---|---|---|
| Female gender: N(%) | 40 (77%) | 14 (74%) | 26 (79%) | 0.74 |
| Current age – years: median (IQR) | 35 (27) | 19 (11) | 45 (19) | NA |
| [range] | [4−68] | [4−68] | [21−64] | |
| Age at symptoms onset-years: median (IQR) | 25 (28) | 11 (7) | 33 (15) | NA |
| [range] | [1.8−61] | [1.8−18] | [19−61] | |
| Age at diagnosis – years: median (IQR) | 31 (27) | 15 (15) | 41 (21) | NA |
| [range] | [2−62] | [2−60] | [20−62] | |
| Time symptoms-diagnosis (years): median (IQR) | 1.5 (7) | 2 (13) | 1 (7) | 0.91 |
| [range] | [0−49] | [0−49] | [0−25] | |
| Atopy: N(%) | 29 (56%) | 13 (68%) | 16 (48%) | 0.16 |
| Allergic rhinitis | 25 (48%) | 11 (58%) | 14 (42%) | 0.28 |
| Asthma | 11 (21%) | 6 (32%) | 5 (15%) | 0.18 |
| Atopic dermatitis | 5 (10%) | 3 (16%) | 2 (6%) | 0.34 |
| Food allergy | 4 (8%) | 3 (16%) | 1 (3%) | 0.13 |
| Total IgE U/mL: median (IQR) | 240 (492) | 520 (602) | 220 (407) | 0.27 |
| [range] | [8.6−1447] | [17−1235] | [8.6−1447] | |
| CsTT (minutes): median (IQR) | 5 (1.25) | 5 (5) | 5 (5) | 0.51 |
| [range] | [3–19] | [5–10] | [3–19] | |
| CTT (ºC): median (IQR) | 16.5 (11.2) | 14 (10) | 18 (11) | 0.11 |
| [range] | [5−27] | [7−22] | [5−27] | |
| Atypical | 9 (17%) | 4 (21%) | 5 (15%) | 0.70 |
| Severity | ||||
| I | 27 (52%) | 10 (53%) | 17 (52%) | 0.17 |
| II | 8 (15%) | 1 (5%) | 7 (21%) | 1 |
| III | 17 (33%) | 8 (42%) | 9 (27%) | 0.6 |
NA: non applicable.
A total of 52 patients were included, with the majority being female (N = 40, 77%). The median age of the patient group at the time of the study was 35 years old. The onset of symptoms was on average at 25 years-old with a median delay in diagnosis of 1.5 years. All patients had an acquired form of ColdU.
In relation to past medical history, one patient had a diagnosis of systemic lupus erythematosus, one psoriatic arthritis, one autoimmune thyroiditis and one chronic lymphocytic leukemia. All patients were tested for cryoglobulins and cold agglutinins and all had negative results. Twenty-nine (56%) patients had a history of atopic disease, most of them allergic rhinitis (N = 25, 48%). Five patients also had other forms of CIndU (4 with cholinergic urticaria, 1 with heat urticaria) and 3 hadchronic spontaneous urticaria (CSU).
All patients were submitted for ice cube test and TempTest®, 43 (82.7%) patients had a positive CST (5 with negative TempTest® and positive ice cube test). Critical thresholds were assessed: median CTT 16.5 °C (IQR 11.2 °C) and CsTT 5 min (IQR 1.25 min). An atypical form of ColdU was diagnosed in 9 patients (positive history and negative cold provocation tests).
In nineteen patients (37%) symptoms had begun prior to them being 18 years old. No significant differences in the evaluated parameters were found between the groups whose symptoms began before or after 18 years old.
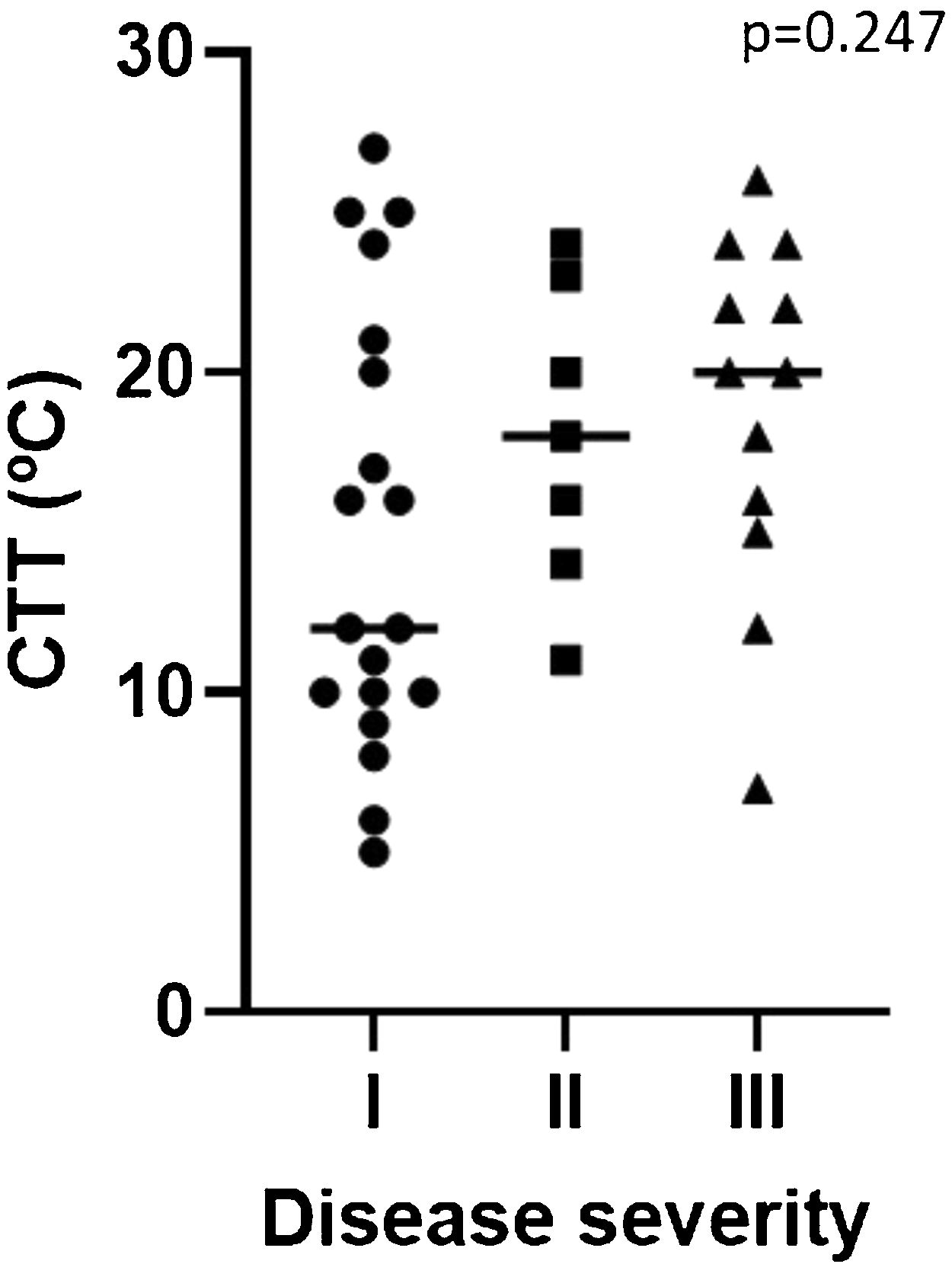
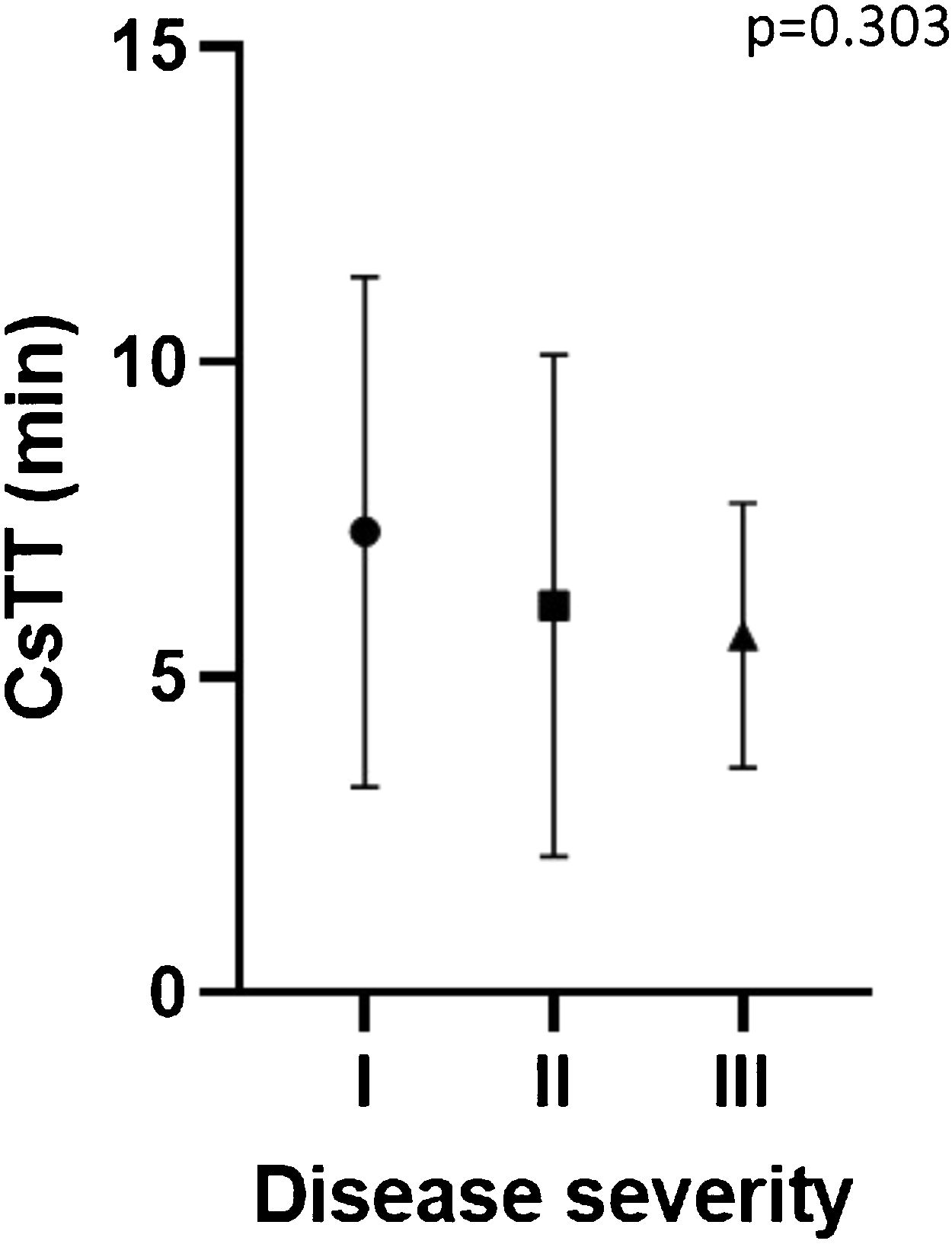
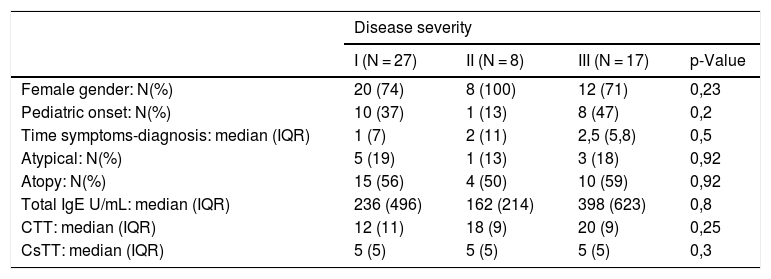
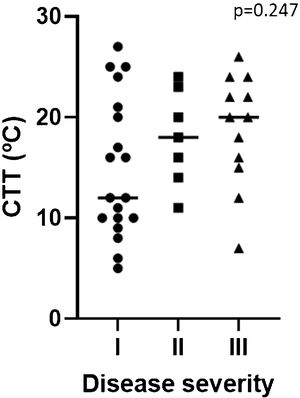
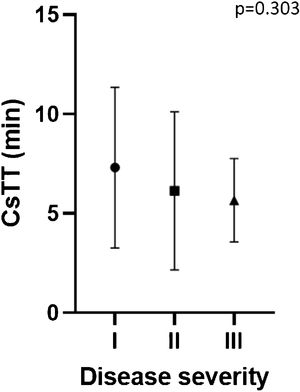
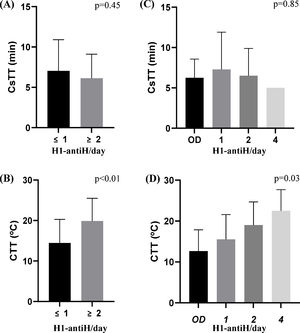
Disease severityTwenty-seven patients (52%) had a localized form of the disease and seventeen (33%) had systemic symptoms including cardiovascular and/or respiratory compromise (Table 1). No significant differences were found between the groups in the evaluated parameters (Table 2). Despite not being statistically significant, CTT was higher and CsTT was lower in more severe groups (Figs. 1 and 2).
Characteristics according to disease severity.
| Disease severity | ||||
|---|---|---|---|---|
| I (N = 27) | II (N = 8) | III (N = 17) | p-Value | |
| Female gender: N(%) | 20 (74) | 8 (100) | 12 (71) | 0,23 |
| Pediatric onset: N(%) | 10 (37) | 1 (13) | 8 (47) | 0,2 |
| Time symptoms-diagnosis: median (IQR) | 1 (7) | 2 (11) | 2,5 (5,8) | 0,5 |
| Atypical: N(%) | 5 (19) | 1 (13) | 3 (18) | 0,92 |
| Atopy: N(%) | 15 (56) | 4 (50) | 10 (59) | 0,92 |
| Total IgE U/mL: median (IQR) | 236 (496) | 162 (214) | 398 (623) | 0,8 |
| CTT: median (IQR) | 12 (11) | 18 (9) | 20 (9) | 0,25 |
| CsTT: median (IQR) | 5 (5) | 5 (5) | 5 (5) | 0,3 |
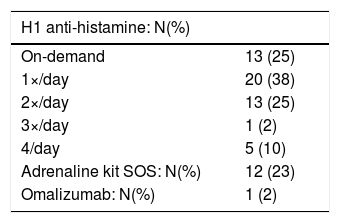
Pharmacologic treatment (summarized in Table 3) was prescribed for all patients, 13 (25%) were on intermittent/as needed therapy. Maximum dosage of H1-antihistamine (4×/day, 2ª line therapy) was prescribed in 10% of patients. Due to severe symptoms refractory to H1-antihistamine treatment, one patient was treated with omalizumab. Adrenaline was prescribed in 12 (23%) patients, all of them with severe symptoms. No patients needed to use the adrenaline kit after diagnosis.
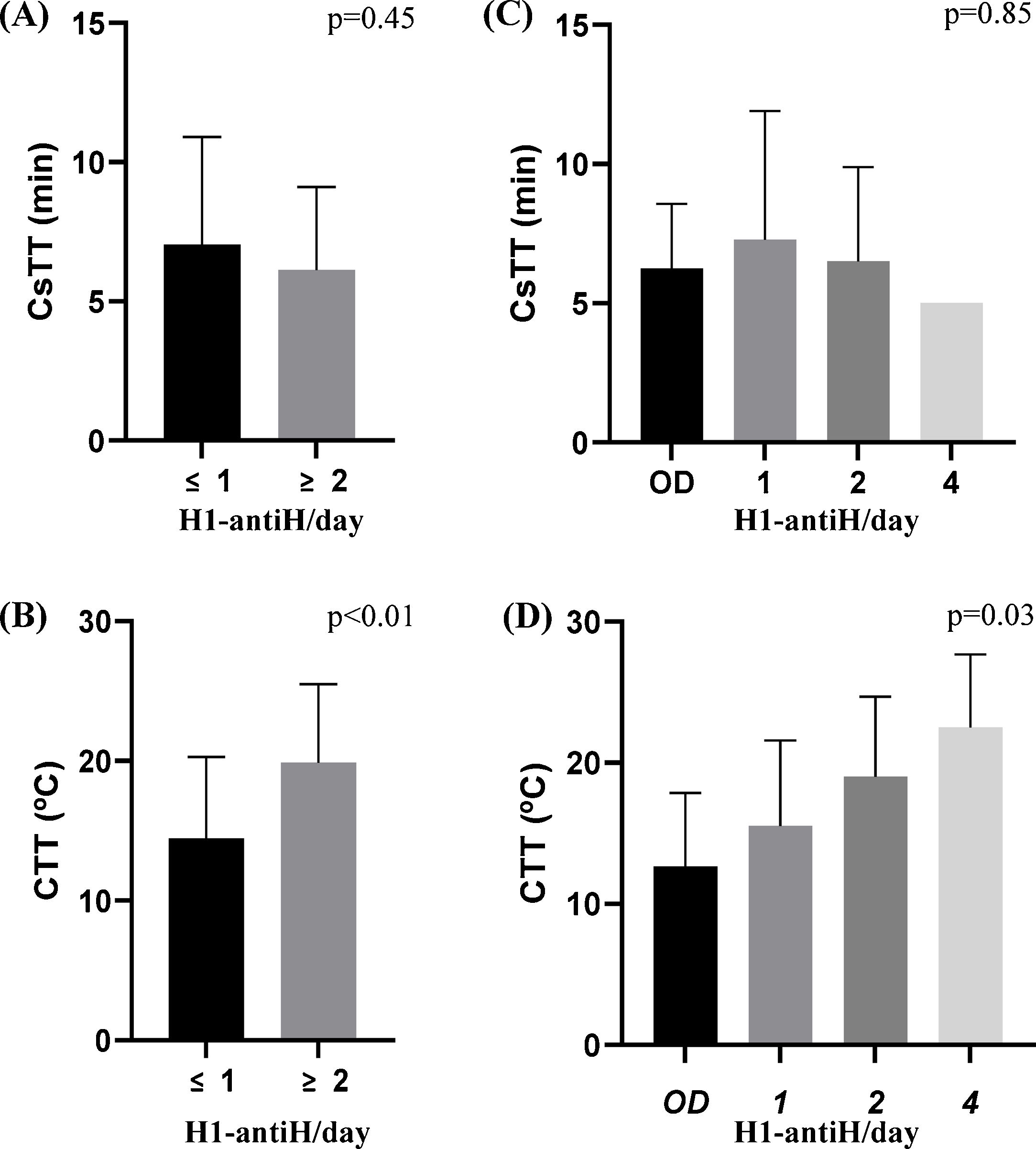
When evaluating CsTT and CTT according to antihistamine daily regimen, we found that patients with higher dosages of antihistamine had significantly higher CTT (p = 0.03) but not CsTT (p = 0.85) (Fig. 3C and D). Moreover, CTT difference increased in significance after patients were divided into two groups, those with on demand or 1×/day treatment and those needing a 2×/day or more dosage (p < 0.01) (Fig. 3B).
CTT and CsTT according to H1-antihistamines treatment regimens (H1-antiH/day). A and B—patients were divided in two groups: ≤1 representing patients treated on-demand or 1/day and ≥2 representing those needing 2 or more antihistamines to control the disease. C and D: Y represents daily dosage of antihistamines (OD-on demand). Only one patient was treated with 3/day dosage and had negative CST.
Similar to previous studies1,5,8 we found that ColdU affects younger individuals and more commonly women.
The relevance of atopy in ColdU patients is debatable, as some studies report relation with the severity or persistence of the disease,5,6 and others failed to find that association.9 In our population a majority of patients had history of atopic disease (56%) but that did not relate to either severity of symptoms or earlier onset of disease.
The presence of CIndU in CSU patients is well established and studies report prevalence that can range from 13.1% to 36.3% of patients.12,13 As would be expected, patients can suffer from ColdU alongside another CindU or CSU, with previous studies reporting this in up to 30% of patients.4,14 The more commonly associated CIndU were symptomatic dermographism (21–22%) and cholinergic urticaria (8–10%).7,8 In our study we found that only 15% had another type of chronic urticaria diagnosed and 9.6% were diagnosed with other CIndU, with cholinergic being the most reported (80%). Although there are no studies evaluating the prevalence of different types of CIndU in the Portuguese population, in a recent work in our center, from a cohort of 477 CU patients with all forms of CU, CIndU accounted for 14% of cases and there was more than one form of CIndU in 8%, data that matched with our findings in this study.15 In this study, 6% of our ColdU patients (N = 3) had coexisting CSU, a percentage not far from that found by Neittaanmäki et al. (1.8%).7
Contrary to previous reports,9,16 in patients whose symptoms began in childhood ColdU were more likely to have negative ice cube tests (hypothesized to be due to insufficient time of exposure), we found no differences between patients whose symptoms began before or after adulthood. Seventeen percent of our patients were diagnosed with atypical urticaria, which is consistent with data found in the literature that points to a prevalence between 4 to 49%.6,7,9
ColdU is an heterogenous presentation with symptoms varying from local whealing to anaphylaxis, often relating to the extension and duration of exposure.4,14 Being able to identify risk factors and specific fenotypes of patients with severe reactions would have a beneficial impact in the management of these patients. The assessment of CTT and CsTT in patients with ColdU is recommended and widely used allowing physicians to better advise patients in trigger avoidance, monitor efficacy and adjust dosage of antihistamines.3,8 Some studies relate CTT and CsTT with disease severity and as a predictor of sistemic reactions, showing a shorter CTT and a higher CsTT in patients with more severe disease.9,17 In our study there was a trend for shorter CTT and higher CsTT in patients with systemic reaction, but it did not reach statistical significance.
Patients need to be advised to avoid prolonged exposure to cold stimuli below their temperature threshold, however this is difficult to achieve in everyday life.3,11 First-line treatment is non-sedative second generation anti-H1 antihistamines. Even though patients with less severe disease can control symptoms with cold avoidance and as-required 2nd generation H1 antihistamines, many patients need high doses to control daily symptoms (up to 4/day).3,10,18 Therefore H1 antihistamine dosage is usually personalized. CTT assessed by TempTest has previously showed to be a useful tool in determining efficacy and minimal dosage necessary to prevent symptoms in patients with ColdU.14,19 In our study we found that patients needing higher dosages of antihistamines had higher CTT, however this was not true regarding CsTT, suggesting temperature threshold to be more determinant than exposure time in determining antihistamine dosage.
To those refractory to antihistamine treatment, omalizumab (although not yet approved) has shown good results in ColdU patients.11
ColdU is an heterogenous disease that can present as a life-threatening event. Cold provocation tests and threshold assessment can be an important tool in the management of the disease and identifying severity groups. Cold avoidance and 2nd generation H1-antihistamines (1st and 2nd line) are the standard treatment.
This study was limited by its retrospective nature, yet we present a diversified population that correlates with other studies.9 Larger prospective and multicentric works are needed to clarify the etiopathogenesis of ColdU and identify risk factors for severe disease. The approval of omalizumab usage in ColdU refractory to antihistamines is also an important subject of investigation.
Conflict of interestThe authors declare that they have no conflict of interest.