Primary cutaneous CD4+ small/medium-sized pleomorphic T-cell lymphoproliferative disorder (CD4+ PCSM-TLPD) is an uncommon entity that was first included as an independent entity (named CD4+ primary cutaneous small/medium-sized pleomorphic T-cell lymphoma) in the 2005 classification of lymphoid neoplasms of the WHO-EORTC (World Health Organization–European Organization for Research and Treatment of Cancer). Given its apparent indolent character, the nomenclature was changed in 2016 to CD4+ PCSM-TLPD, although this remained a provisional entity. We present the first case of simultaneous appearance of CD4+ PCSM-TLPD in 2 sisters.
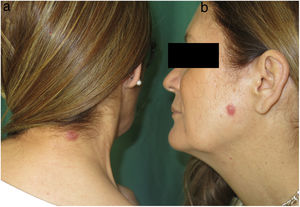
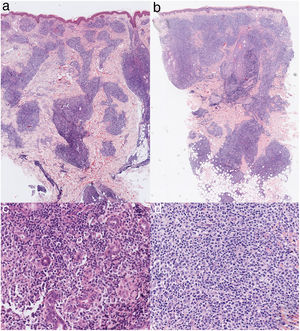
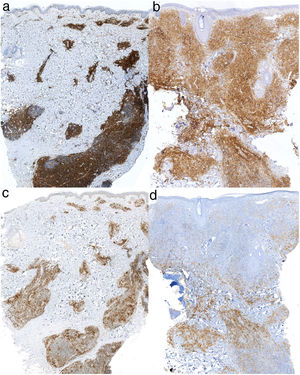
Two sisters, aged 54 and 58 years, were seen for similar lesions located on the left cheek and cervical area, respectively, that had appeared 2 and 3 years earlier, respectively. Neither of the sisters reported any potential triggers. The patients did not live together, but both lived in rural areas. The physical examination revealed firm, infiltrated, erythematous cupuliform papules with neat borders (Fig. 1). Histology showed a dense lymphohistiocytic infiltrate in the dermis and hypodermis with tropism for adnexal structures. Epidermotropism was absent. The infiltrate consisted of small-to-medium-sized pleomorphic lymphocytes, with mild-to-moderate atypia (Fig. 2). Immunohistochemistry was positive for CD3, CD4, and PD-1, and negative for CD10 and Bcl-6, and revealed large isolated CD30+ cells and preserved CD7/CD5/CD2 immunostaining (Fig. 3). Accompanying CD8+ and CD20+ cell populations were also observed. Monoclonal T-cell receptor (TCR)-beta rearrangement was observed for both samples, with no clonal overlap between samples. The results of the staging workup (cervical thoracic abdominal pelvic computed tomography scan and lactate dehydrogenase analysis) were negative. It was decided to adopt a wait-and-see approach, and spontaneous remission was observed after 6 months in both patients.
Histological images of the lesions in the cervical region (A) and on the left cheek (B) showing lymphohistiocytic infiltrate in the dermis and hypodermis with tropism for adnexal structures and the absence of epidermotropism (hematoxylin-eosin, original magnification ×2). Histological images of the lesions in the cervical region (C) and on the left cheek (D) showing infiltrate consisting of pleomorphic cells with mild-to-moderate atypia (hematoxylin-eosin, original magnification ×20).
Immunohistochemistry showing positive staining for CD4 (original magnification ×2) in the lesions in the cervical region (A) and on the left cheek (B). Immunohistochemistry showing positive staining for PD-1 (original magnification ×2) in the lesions in the cervical region (C) and on the left cheek (D).
CD4+ PCSM-TLPD is classified as a provisional entity within the category of cutaneous lymphomas, of which it accounts for approximately 2% of cases. Although it can occur at any age, it typically affects adults that have reached the fifth decade of life, and no clear sex predisposition is described.1–8 The pathogenesis of this entity is unknown and controversial; a recent series of 62 patients, of whom 11 underwent genomic analyses, reported no associated genomic alteration.2
CD4+ PCSM-TLPD typically presents as solitary lesions in the upper body (mainly the head or neck), usually in the form of asymptomatic nodules, plaques, or erythematous tumors.2 Histology reveals infiltrate composed of small-to-medium-sized pleomorphic lymphocytes with mild-to-moderate cellular atypia, the absence of obvious epidermotropism, and, in some cases, tropism for adnexal structures.2 The immunohistochemical profile of these cells is CD3+, CD4+, CD30-, CD8-, with variable loss of T-cell markers (CD7, CD5, and CD2) and variable positivity for follicular T-helper cell markers (PD-1, Bcl-6, and CXCL-13).2–4 The true nature of these cells is not entirely clear. Accompanying the neoplastic T cells are populations of CD20+ B cells and CD8+ T cells, as well as some large, isolated, pleomorphic CD30+ cells (<30%). The proliferative (Ki-67) index is usually less than 50%.2 A monoclonal TCR gene rearrangement has been described in more than 80% of cases in the majority of published series.1–8
CD4+ PCSM-TLPD has a very favorable prognosis, with a 5-year survival rate of 80–90%.2,4 In the most extensive (n = 136) case series published,3 Beltraminelli and coworkers reported no extracutaneous involvement in 45 patients followed for a mean period of 64 months. Systemic involvement has only been described in a series of 24 patients published by García-Herrera et al.6 The authors reported 5 cases of extracutaneous involvement and proposed that rapid growth, a high proliferative index, and scarce CD8+ infiltrate were poor prognostic factors, although the study population consisted of patients with very heterogeneous characteristics. We believe that based on their characteristics (large, fast-growing lesions with variable expression of CD4, loss of CD7, a high proliferative index, and extracutaneous involvement), these lesions would be better classified as primary cutaneous peripheral T-cell lymphoma not otherwise specified. No other cases of systemic involvement have been described in any of the other published series.1–8 Treatment options include surgery (first-line treatment in patients with solitary lesions), topical corticosteroids, and phototherapy. Only 3 cases of complete spontaneous remission are described in the literature.5,9,10
The differential diagnosis includes other cutaneous B-cell and T-cell lymphomas, as well as reactive lymphoproliferative processes and pseudolymphomas, the latter of which are difficult to differentiate.5 The presence of pleomorphism and cellular atypia, the loss of T-cell markers, positivity for follicular T-helper cells, and monoclonal TCR rearrangement are findings that can help guide the diagnosis of CD4+ PCSM-TLPD, although these findings may also be present to a lesser extent in reactive processes.2–5
In conclusion, we present 2 new cases of CD4+ PCSM-TLPD and describe for the first time 2 simultaneous cases of this entity in sisters. Both patients achieved spontaneous remission, of which there are few reports in the current literature. The true nature of this entity and its differential diagnosis from reactive lymphoproliferative processes has been the subject of some controversy since its classification as a form of cutaneous lymphoma. The simultaneous appearance of this lesion in 2 sisters supports a reactive origin, given the possibility of exposure to similar environmental factors, as well as a possible influence of as-yet-unknown genetic factors.
Please cite this article as: Ponce S, Peñate Y, Montenegro T. Trastorno linfoproliferativo primario de células T pleomórficas pequeñas/medianas CD4+ coincidente en dos hermanas. Actas Dermosifiliogr. 2020;111:271–273.