Dermatofibroma (DMF) is a benign tumor of myofibroblastic origin that is rare in pediatric patients. The entity was first described in the literature by Hügel in 1991 as plaque-like dermal fibromatosis.1 The term dermatofibroma was later coined by Kamino.2
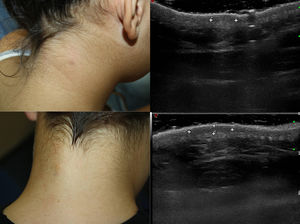
These tumors usually present clinically as a solitary plaque or nodule, and may be multiple, poorly defined, with mild erythema or hyperpigmentation, and are usually asymptomatic, although they may cause mild pruritus. In the pediatric form, the lesions occur predominantly in the cervical region (56%) and tend to remit spontaneously.3 The adult form, however, tends to be located on the shoulders or on the proximal surface of the limbs. It is more common in women (96%) and does not tend to remit spontaneously.4 The clinical differential diagnosis is very broad4 (Fig. 1).
Diagnosis of DMF is histologic. It consists of a proliferation of fusiform cells (fibroblasts and myofibroblasts) arranged with the long axis parallel to the surface of the epidermis and sparing adnexal structures. Immune staining may help with the diagnosis. Expression of vimentin is constant, that of muscle-specific actin and smooth-muscle actin is variable, and focal expression of CD34+ may be seen in some cases.5,6
High-frequency ultrasound, which is increasingly common in dermatologic practice, can help with the clinical diagnosis and may be helpful in the follow-up of these benign tumors.
We took all the patients under 16 years of age with a diagnosis of DMF from the anatomical pathology database of Hospital Universitario de Fuenlabrada, Spain, and we selected those cases in which an ultrasound study had been performed.
The clinical data are shown in Table 1. The study group contained 3 girls and 5 boys. Age at diagnosis ranged between 20 months and 15 years. The lesions were located on the neck (6 patients), on the left shoulder (1 patient), and on the occipital region (1 patient). The lesions had appeared between a month and a year before consultation. Clinically, the lesions were nodular or plaque-like, poorly defined in 6 of the patients (well demarcated in 2 cases), and slightly erythematous or hyperpigmented. One of the patients presented 2 lesions. Three of the lesions were painful and 2 were pruritic; the rest were asymptomatic.
Clinical and ultrasound characteristics of the patients.
| Sex | Age | Location | Time | Clinical features | Physical examination | Ultrasound features | |
|---|---|---|---|---|---|---|---|
| 1 | Female | 15 y | Posterior cervical | 1 mo | Pain, stable | Poorly demarcated, hyperpigmented nodule | Poorly demarcated hypoechoic dermal lesion without Doppler flow |
| 2 | Male | 11 y | Posterior cervical | Months | Asymptomatic, stable | Poorly demarcated nodule | Poorly demarcated hypoechoic dermal lesion without Doppler flow |
| 3 | Male | 11 y | Posterior cervical | 1 y | Asymptomatic, growth | 2 well-demarcated nodules | Poorly demarcated hypoechoic dermal lesion without Doppler flow |
| 4 | Female | 11 y | Left shoulder | Months | Pain | Poorly demarcated nodule | Hypoechoic dermal lesion, increased Doppler flow in points on periphery |
| 5 | Male | 10 y | Posterior cervical | Months | Asymptomatic | Poorly demarcated erythematous nodule | Poorly demarcated hypoechoic dermal lesion with increased Doppler flow |
| 6 | Male | 10 y | Posterior cervical | Months | Asymptomatic, slight growth | Well-demarcated, slightly hyperpigmented nodule. | Poorly demarcated hypoechoic dermal lesion without Doppler flow |
| 7 | Female | 9 y | Occipital | 1 y | Occasional pruritus, progressive growth | Poorly demarcated erythematous nodule | Poorly demarcated hypoechoic dermal lesion without Doppler flow |
| 8 | Male | 20 mo | Posterior cervical | 8 mo | Pruritic, fluctuating size | Greyish-erythematous plaque | Poorly demarcated hypoechoic dermal lesion without Doppler flow |
An ultrasound study with a high-resolution probe (Esaote MyLab® Class C, 18 MHz linear probe) showed rounded, hyperechoic, nonencapsulated, poorly defined, dermal-epidermal lesions without Doppler flow, except in 2 cases, which presented Doppler flow on the periphery.
Clinical diagnosis of DMF may be difficult and high-resolution ultrasound may help with the differential diagnosis and with guiding treatment, essentially in large or pruritic lesions.
The ultrasound differential diagnosis includes lesions such as dermatofibroma, which usually presents as dermal lesions that may extend to the subcutaneous cellular tissue, with poorly defined, spiculated borders, without vascularization, and with changes in the echogenicity of the adjacent tissue7; plaque-like neurofibroma, which also tends to present as hypoechoic lesions located in the dermis, with well-defined borders and posterior reinforcement.8 Other lesions, such as hypopigmented blue nevus, piloleiomyoma, smooth-muscle hamartoma, and connective tissue nevus, tend to be better defined. Dermatofibrosarcoma protuberans has a jellyfish-like appearance, with an oval shape and focally poorly defined borders; it invades the subcutaneous tissue in the form of hypoechoic tentacle-like projections with focal hyperechoic areas and posterior reinforcement and abundant vascularization.9 Desmoid fibromatosis and scars tend to present with a more elongated morphology, although cases of DMF with a linear configuration have been reported.10
A watch-and-wait approach is a valid treatment option, as this is a benign tumor with little tendency toward recurrence. Excision is sometimes required due to the symptoms.
In our experience, given the clinical suspicion and a high-resolution ultrasound study compatible with the diagnosis, an appropriate approach would be clinical and ultrasound follow-up, with biopsy reserved for lesions with atypical characteristics, such as high Doppler flow, and excision of symptomatic lesions only. This conservative approach is valid for all ages, as it avoids unnecessary excisions and the risk of cosmetic defects, especially in pediatric patients, in whom most cases of surgery require general anesthesia or sedation.
Conflicts of InterestThe authors declare that they have no conflicts of interest.