Capillary malformation-arteriovenous malformation syndrome is a rare type of vascular malformation first described in 2003. It is an autosomal dominant inherited disorder that has been reported in association with heterozygous mutations in the RASA1 gene, which encodes the protein RASp21. The clinical picture is characterized by multiple small capillary malformations which are associated with either arteriovenous malformations or arteriovenous fistulas in both the affected individual and other members of their family. We describe 2 new familial cases of this syndrome that were clinically and genetically diagnosed and studied in our hospital.
El síndrome malformaciones capilares-malformaciones arteriovenosas es un tipo de malformación vascular poco frecuente que se describió en 2003. Se hereda de forma autosómica dominante, y se ha objetivado que está causado por mutaciones heterocigotas en el gen RASA1, que codifica la proteína RASp21. Dicho síndrome se caracteriza por malformaciones capilares pequeñas y múltiples que se asocian con malformaciones arteriovenosas o fístulas arteriovenosas, tanto en los individuos afectos como en sus familias. Describimos aquí 2 nuevos casos familiares de este síndrome que hemos diagnosticado y estudiado en nuestro centro, tanto desde el punto de vista clínico como genético.
Capillary malformation-arteriovenous malformation (CM-AVM) syndrome is an autosomal dominant disorder that was first described in 2003. It is caused by heterozygous mutations that deactivate the RASA1 gene, which encodes the protein p120Gap.1 The main characteristic of CM-AVM syndrome is the presence of atypical, multifocal capillary malformations associated with high-flow vascular malformations both in the affected individual and in other family members.2
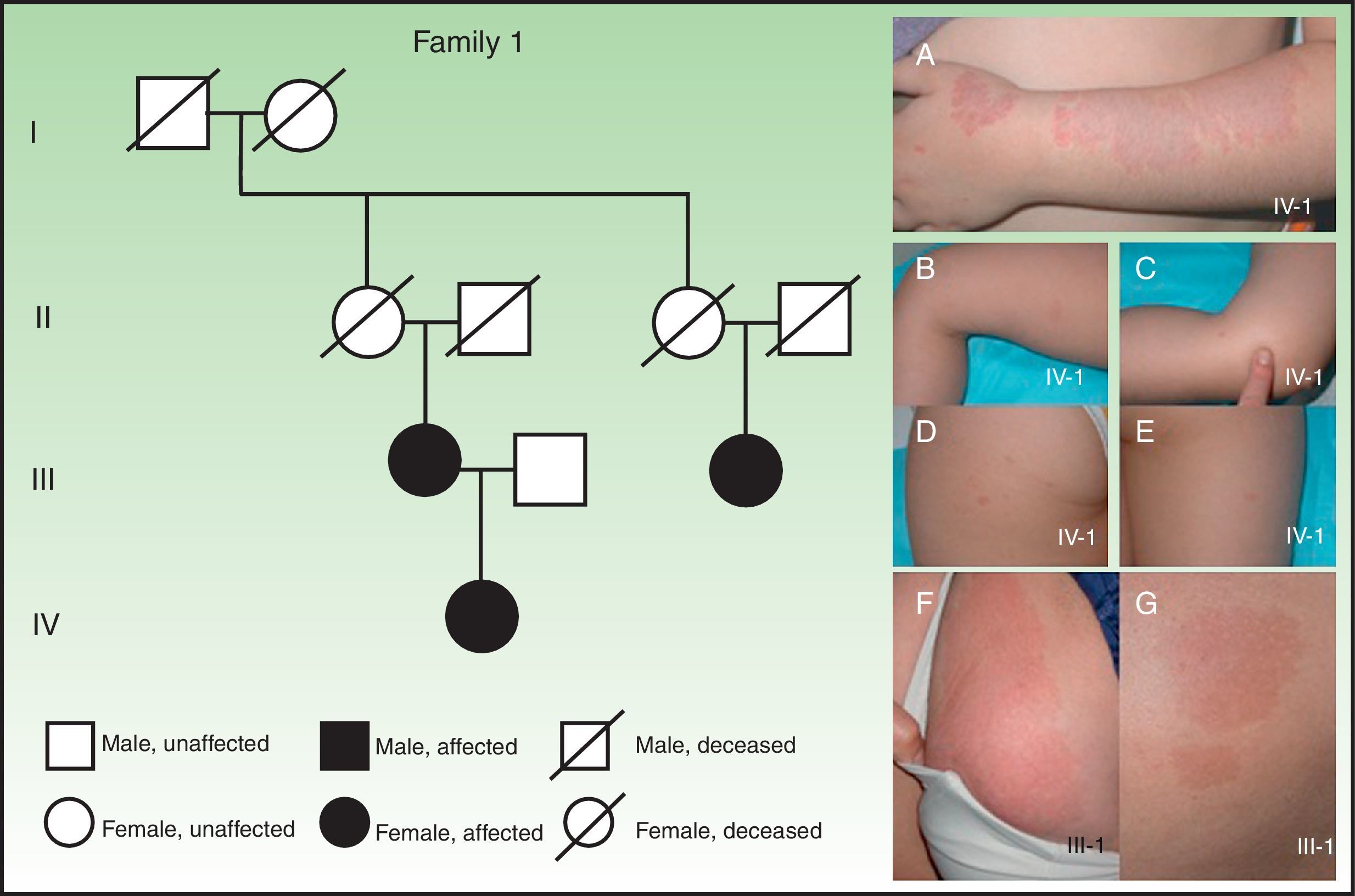
Case DescriptionsPatient 1A 4-year-old girl was referred to our department for treatment of a vascular lesion on the left upper limb. She presented a pink macule measuring 17×8cm that had geographic borders and superficial telangiectasias and was located on the dorsolateral aspect of the left forearm (Fig. 1A). The lesion was pulsatile and warm to the touch. The patient reported paresthesia and pain in the lesion. Magnetic resonance imaging and arteriography of the left forearm confirmed the clinical impression of an arteriovenous malformation. Physical examination revealed several smaller capillary malformations, ranging in size from 1cm to 1.5cm, surrounded by whitish peripheral halos and distributed randomly over the body (Fig. 1, B-E). The patient's mother had a capillary malformation measuring 20×5cm on the right breast and another measuring 10×4.5cm on the buttocks (Fig. 1, F and G), and a female cousin of the mother had an intracranial arteriovenous malformation. Cerebral magnetic resonance imaging of the patient was normal.
Clinical characteristics of family 1. A, Arteriovenous malformation on the left upper limb of a 4-year-old girl. B-E, Multiple atypical capillary malformations detected on the upper and lower limbs. F and G, Large capillary malformations on the right breast (F) and on the right thigh and buttock (G) of the patient's mother.
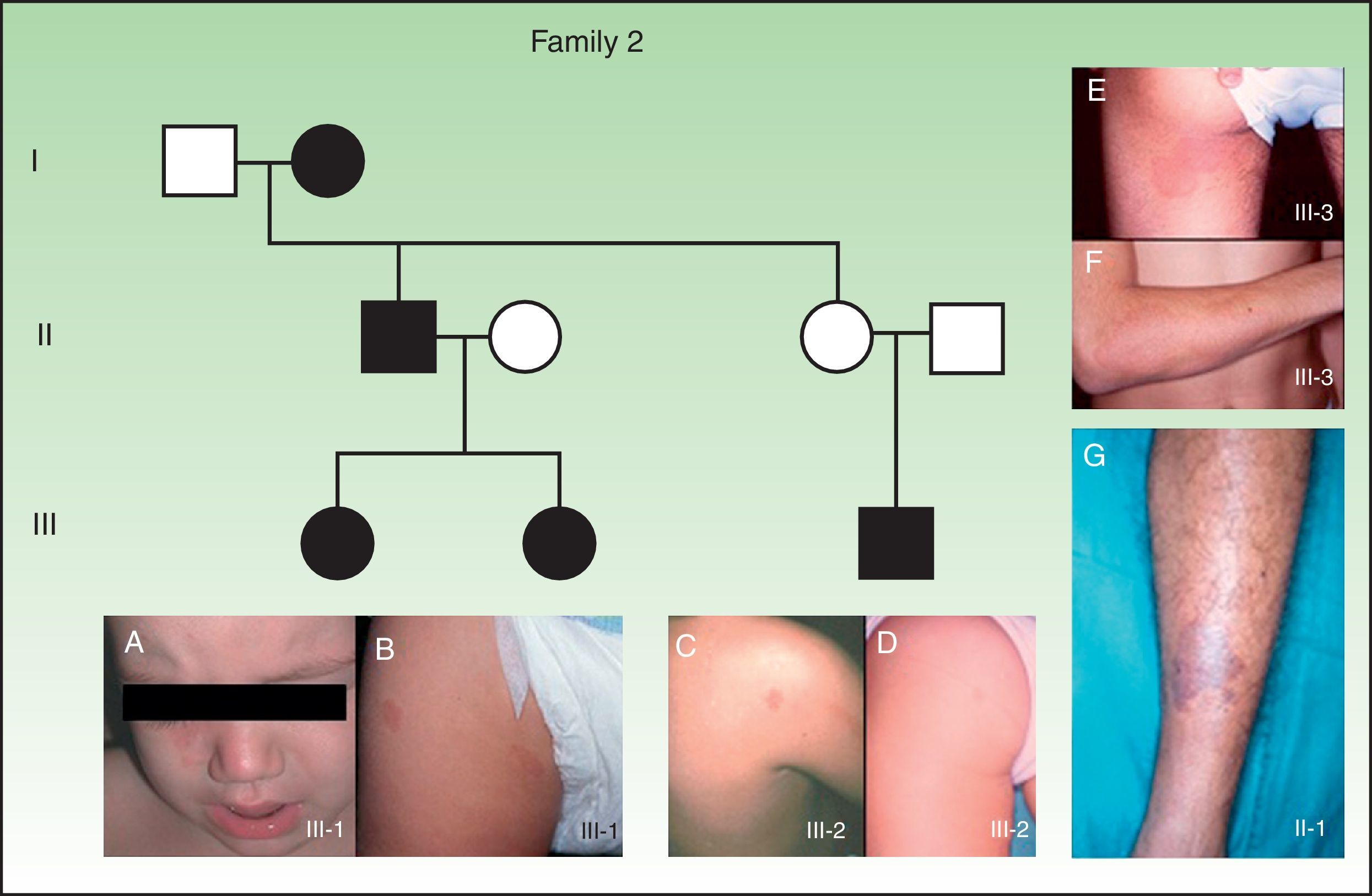
An 18-month-old girl presented a capillary malformation measuring 4×1.5cm on the right cheek and bridge of the nose (Fig. 2A). Physical examination revealed a further 3 smaller capillary malformations elsewhere on the body, ranging in size from 1cm to 1.5cm and surrounded by whitish peripheral halos (Fig. 2B). The patient's older sister had several capillary malformations, ranging in size from 0.5 to 1.5cm, located on the nose, upper limb and lower limb and surrounded by whitish peripheral halos (Fig. 2, C and D). A male paternal cousin of the patient had a capillary malformation measuring 7×4cm on the left thigh and another measuring 13×5cm on the right forearm (Fig. 2, E and F). The patient's father had an arteriovenous malformation on the right lower limb (Fig. 2G) and her paternal grandmother had an arteriovenous malformation on her right forearm. Familial CM-AVM syndrome was suspected. The patient underwent cerebral magnetic resonance imaging and angiography, which revealed the presence of an arteriovenous fistula in the territory of the middle cerebral artery. Because the lesion was associated with a high risk of bleeding, selective embolization of the arteriovenous fistula was performed even though the patient had no symptoms. The patient remains asymptomatic after more than 4 years of follow-up.
Clinical characteristics of family 2. A, Capillary malformation on the right cheek of patient 2, an 18-month-old girl. B, Smaller capillary malformations distributed randomly over the body of the same patient. C and D, Several smaller, less apparent capillary malformations on the patient's older sister. E and F, Large capillary malformations on a male cousin of the patient. G, Arteriovenous malformation on the right lower limb of the patient's father.
Blood samples were collected from all affected family members and sent to Prof. Miikka Vikkula and Dr. Nicole Revencu of the Laboratory of Human Molecular Genetics (Christian de Duve Institute of Cellular Pathology, Université Catholique de Louvain, Brussels, Belgium) for genetic testing. All affected family members were positive for mutations in the RASA1 gene.
DiscussionCapillary malformations, or port-wine stains, are the most common vascular malformations, occurring in 0.3% of newborns.3 These low-flow vascular lesions present as pale pink, erythematous, or violaceous macules. Capillary malformations are usually unilateral but can affect any part of the body. Unlike other macular lesions that appear on the face and fade over time (nevus flammeus neonatorum, also known as salmon patch or angel's kiss), capillary malformations tend to darken with age.
Most capillary malformations occur sporadically and present as solitary lesions. However, since the first description of cases of multiple familial capillary malformations by Shelley and Livingood4 in 1949, numerous authors have suggested that this type of capillary malformation follows a pattern of autosomal dominant inheritance with variable expression.5 Following these observations, CM-AVM syndrome was first described in 2003 as being the result of a heterozygous mutation in chromosome band 5q13.3,1,2 specifically in the RASA1 gene.6,7 This gene encodes the protein p120Gap, an inhibitor of the Ras pathway, which is involved in cell growth, differentiation, and proliferation.8,9 Atypical capillary malformations—the main feature of CM-AVM syndrome—are present in 100% of families with the mutation.10–12 The capillary malformations associated with this syndrome are characterized by an erythematous brownish color, multifocality, random distribution, the presence of a whitish peripheral halo around the lesions, and an increase in local temperature. The malformations may be present at birth, but they usually appear in early childhood. The size of the lesions ranges from 1cm to more than 15cm. Atypical capillary malformations indicate greater susceptibility to high-flow vascular anomalies (arteriovenous malformations or arteriovenous fistulas); a high-flow vascular malformation has been found in at least 1 member of all the families with this mutation that have been studied to date.10–12 The high-flow malformations associated with CM-AVM syndrome can affect skin, muscle, bone, the intracranial region, or the spinal region.13 One study found that up to 18% of patients with the RASA1 gene mutation have an associated arteriovenous malformation or fistula (intracranial in 7.1% of cases and extracranial in 11.4% of cases).10 It is also possible that some reported cases of Cobb syndrome (an arteriovenous malformation of the spinal cord associated with a capillary malformation along the involved dermatome) are, in fact, cases of CM-AVM syndrome.14
It is therefore the multifocal nature of a patient's capillary malformations that should raise suspicion of CM-AVM syndrome and prompt the physician to investigate the existence of potential internal arteriovenous malformations before they cause symptoms. In the case of high-flow cerebral or spinal vascular lesions, detection is of the utmost importance because the first manifestation of such lesions can be hemorrhage, leading to serious consequences.13,14 A recent study found that in 43% of cases of children with intracranial hemorrhage secondary to arteriovenous malformation, atypical capillary malformations were present in the patient or a first-degree relative.15 In the case of our second patient, we detected an arteriovenous fistula in the territory of the middle cerebral artery that might otherwise have first manifested as spontaneous bleeding.
It should be noted that a nonnegligible percentage (21%) of the patients with multifocal capillary malformations (associated or not with high-flow arteriovenous malformations) who have been tested by Prof. Vikkula are negative for the mutation of the RASA1 gene.10 However, most of those cases were sporadic (10/12) and only 2 families have been studied. Patients with multifocal capillary malformations who are negative for the mutation probably have a yet unknown mutation of the RASA1 gene, because they and their family members also have a higher risk of high-flow arteriovenous malformations (present in up to 25% of cases). It is therefore recommended that these patients and their family members undergo screening for high-flow lesions. Genetic testing should be performed if possible because it can help to establish a genotype-phenotype correlation. It is not essential, however, because screening for associated arteriovenous malformations is justified in these patients regardless of the results of genetic testing.
In conclusion, the results of the aforementioned studies suggest that an exhaustive medical history should be taken for any patient with atypical capillary malformations and that the patient and his or her family members should undergo a full physical examination so that any atypical capillary malformations or high-flow vascular lesions that suggest an autosomal dominant pattern of inheritance can be detected. If the phenotype with capillary and arteriovenous malformations is found, the patient with the atypical capillary malformations and his or her family members should undergo magnetic resonance imaging and angiography to screen for subclinical high-flow intracranial and spinal vascular lesions. This approach can make it possible to anticipate cerebral and spinal hemorrhages, which could have fatal consequences for these families. The patients described in this article did not undergo cerebrospinal magnetic resonance imaging because the article that described the association between multiple capillary malformations and spinal arteriovenous malformations was published in 2010, several years after the patients were treated in our department.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
The authors thank the patients and their families for their collaboration. We also wish to thank Prof. Vikkula for performing the genetic tests that made it possible to detect the mutation of the RASA1 gene in the affected families.
Please cite this article as: Català A, et al. Síndrome malformaciones capilares-malformaciones arteriovenosas: presentación de 2 casos, claves diagnósticas y manejo. Actas Dermosifiliogr. 2013;104:710–3.