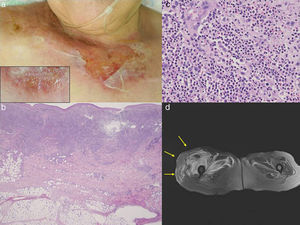
A 79-year-old female, who had suffered from myelodysplastic syndrome (MDS) (RAEB-1), was referred to our department complaining of painful lesions on the neck, chest and lower extremities with fever-up which appeared three weeks previously. She had received occasional transfusion for her MDS, but granulocyte-colony stimulating factor (G-CSF) was not administered. Physical examination showed ill-defined, tender edematous erythemas with bullous and erosive lesions on the chest (Fig. 1a). In addition, painful fresh-colored erythematous plaques were scattered on the lower extremities. Laboratory examination showed slightly elevated white blood cell counts (9100/μl with 27% Band, 29% Seg, 12% Lym, 4% Mono, 4% Eo, 9% Baso, and 10% Meta), and increased levels of erythrocyte sedimentation rate (136mm/h) and C-reactive protein (9.0mg/dl). A biopsy specimen from the chest showed dense neutrophilic infiltration throughout the edematous dermis (Fig. 1c). Bacterial culture resulted sterile. Bone marrow biopsy revealed severe hypocellular bone marrow with a marked decrease of erythroblasts and megakaryocytes. After admission, systemic prednisolone (20mg/day) was started which resulted in the improvement of skin lesions. However, during the course, she complained of severe muscle pain of the right thigh along with fever up to 39°C. Examination by MRI showed edematous swelling on the right gluteus maximus muscle (Fig. 1d). Unfortunately, muscle biopsy was not performed, because her general conditions worsened. Serum creatine kinase level was not elevated and myositis was gradually improved without dose-up of prednisolone. However, her general condition was worsened, and she died of disseminated intravascular coagulation, renal failure, and complete A-V block one month after admission.
(a) Painful, erosive lesions on the upper chest with peripheral tense blisters (insert). (b) Histological features showing dense neutrophil infiltration throughout the edematous dermis. (c) Higher magnification showed neutrophil infiltration. (d) MRI examination revealed edematous swelling on the right gluteus maximus muscle.
Sweet's syndrome is characterized by tender erythematous skin lesions accompanied by fever-up, in which inflammatory cells predominantly consisted of neutrophils infiltrate diffusely in the dermis. Sometimes Sweet's syndrome presents with atypical variants,1 and bullous variant is histologically characterized by extensive neutrophilic exocytosis and severe edema of the upper dermis. Whether cases of bullous Sweet's syndrome are commonly associated with hematological disorders is controversial.2,3 In the present case, bullous lesions were developed in a patient with active and severe MDS. The patient had no other apparent triggers such as upper airway or gastrointestinal infections and the use of new drugs, for the induction of Sweet's syndrome. Also, the patient developed non-bullous infiltrative erythema on the knee, and muscle tenderness during the course. So far, several cases of extracutaneous manifestations of Sweet's syndrome have been reported involving the lung, digestive tract, joints, lymph nodes, liver, spleen, eyes, central nervous system, and bone.4 Only several cases of neutrophilic myositis have been reported in association with neutrophilic dermatosis5; however, to our knowledge, there have been no reports of neutrophilic myositis in association with bullous Sweet's syndrome. A previously reported case developed severe sterile neutrophilic myositis as the first manifestation of acute myelogenous leukemia.6 In the present case, myositis was developed soon after admission, which occurred almost concurrently with cutaneous manifestations. Because of the increased risk of infection, we did not escalate the dose of prednisolone; however, muscle lesions were transient and gradually improved. Because muscle biopsy was not carried out, it is uncertain that the patient developed neutrophilic myositis during the course. Hematoma was unlikely, but other factor such as infection was not denied, because drainage procedures were not performed. In such cases as immunocompromised patients like ours, it is often difficult to decide whether other organ involvement is caused by aseptic neutrophilic infiltration or infection.
Conflict of interestsThe authors declare no conflict of interests.