Breast implant–associated anaplastic large cell lymphoma (BIA-ALCL) is a very rare form of T-cell lymphoma and its incidence has grown in recent decades. The most common presentation is breast swelling due to periprosthetic seroma. In this article, we describe a case of BIA-ALCL whose first clinical manifestation was skin lesions in the intermammary area. There have very few reports of this presentation in the literature.1
A 70-year-old woman was referred to our department for evaluation of an erythematous, indurated plaque with slight superficial scaling in the intermammary area and increased right breast volume (Fig. 1). She had been diagnosed with right breast carcinoma 5 years earlier and had undergone mastectomy and prosthetic breast reconstruction. She was receiving hormone therapy. No signs of recurrence had been detected in a follow-up mammogram 4 months earlier. The ultrasound examination had shown waves indicating possible periprosthetic fluid collection but no findings suggestive of malignancy. The patient reported asthenia and considerable weight loss in recent months. Skin biopsy showed spongiotic dermatitis with a superficial and deep perivascular lymphohistiocytic infiltrate. No tumor cells were observed and immunohistochemical staining was negative for cytokeratin 19 and CD30.
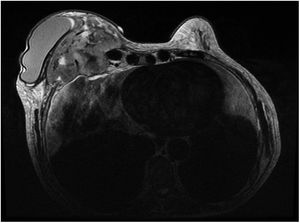
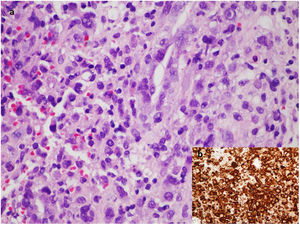
Magnetic resonance imaging was ordered to assess the possibility of a cutaneous metastasis from breast cancer or a prosthetic complication. The findings showed a retroprosthetic mass invading the chest wall and extending into the mediastinum (Fig. 2). Aspiration of the periprosthetic fluid showed large CD30+, CD3+, and ALK- tumor cells, confirming the diagnosis of BIA-ALCL (Fig. 3). Given the presence of extramammary disease, the patient was treated with systemic chemotherapy (cyclophosphamide, hydroxydaunorubicin, and prednisone) and brentuximab before surgical explantation of the implant and capsulectomy.
A, Microscopic image of the cell block preparation from the periprosthetic fluid (hematoxylin-eosin, original magnification ×60) showing large loose and small discohesive clusters of pleomorphic tumor cells against a background of inflammatory granulation tissue. B, Strong immunohistochemical expression of CD30.
BIA-ALCL is a lymphoproliferative disorder caused by tumor cells invading the capsule or periprosthetic fluid. The mean age at diagnosis is 52.5 years and the mean time from breast implantation to diagnosis is 9 years.2 BIA-ALCL presents as periprosthetic seroma in 86% of cases,2 although it can also manifest as a mass, nodule, or lymph node enlargement. Skin lesions are very rare.1
Just 2 cases of BIA-ALCL with skin lesions as the presenting manifestation have been reported.1,3Elswick and Nguyen1 described the case of a woman who presented with a breast mass, erythema, and breast swelling in addition to elevated acute phase reactants in the blood work-up. The skin biopsy was negative for malignancy, suggesting to the authors that the skin lesions were due to a periprosthetic infection concurrent with the lymphoma. In the case published by Alcalá et al.,3 however, the detection of CD30+ tumor cells during histologic examination of the skin nodules was key to establishing a diagnosis of BIA-ALCL rather than breast cancer recurrence. Nineteen of the 186 patients in the PROFILE (Patient Registry and Outcomes for Breast Implants and Anaplastic Large Cell Lymphoma Etiology and Epidemiology2) registry developed skin lesions in addition to other systemic manifestations, and 12 of these lesions were described as redness on the skin. Type of skin lesion was not specified in the other cases, and none of the lesions were analyzed histologically.
Neither our case nor the cases in the literature (with the exception of that described by Alcalá et al.3) exhibited specific clinical or microscopic changes. BIA-ALCL should be suspected in patients with breast implants who develop skin lesions, in particular erythema, and breast swelling.
It has been hypothesized that the etiology of BIA-ALCL is multifactorial and is influenced by type of implant, genetic predisposition, and possible chronic periprosthetic superinfection associated with a bacterial biofilm.4
The Spanish Ministry of Health recently published a clinical protocol for the detection of BIA-ALCL that recommends an initial ultrasound assessment with aspiration and cytologic and microbiologic analysis of periprosthetic fluid.5 BIA-ALCL is histologically characterized by a proliferation of highly pleomorphic lymphoid cells with abundant cytoplasm and an irregular nucleus.3 Diagnosis must be confirmed by immunohistochemistry, which characteristically shows CD30 positivity and ALK negativity in all tumor cells.3,6
BIA-ALCL is generally localized at diagnosis and the prognosis is excellent following surgical excision.7 Extracapsular spread is very uncommon. In their review of 173 cases of BIA-ALCL, Brody et al.8 reported just 18 cases of extracapsular spread and 9 of these had a fatal outcome.
We have described a new case of advanced-stage BIA-ALCL in a woman who, in addition to increased breast volume, presented with skin lesions and constitutional syndrome. She required chemotherapy prior to surgery.
Although BIA-ALCL is rare, the number of cases in recent years has increased exponentially.8 It is crucial thus to be familiar with this condition, as early diagnosis together with detection of localized disease is associated with a favorable prognosis following surgical explantation and capsulectomy.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Gracia-Darder I, Izquierdo N, Boix-Vilanova J, Ramos D. Linfoma anaplásico de células grandes asociado a implantes mamarios. Actas Dermosifiliogr. 2021;112:928–930.