Blue toe syndrome (BTS) is defined as the development of a blue or violaceous discoloration of 1 or more toes in the absence of trauma, serious cold-related injury, or alterations that could cause diffuse cyanosis.1
We present the case of a 46-year-old man, a smoker with a past history of hypertension and hypertriglyceridemia, who was on treatment with enalapril, torasemide, diltiazem, doxazosin, and gemfibrozil. He came to the emergency department because “his toes had gone blue” a few hours after noting an acute, intense pain in the left calf 10 days earlier.
The patient reported no endovascular or surgical procedures in the previous months and no history of intermittent claudication. Physical examination revealed a bluish discoloration of the fourth and fifth toes of the left foot that was spreading in the form of patchy, reticulated erythematous-violaceous macules over the rest of the foot, the ankle, and the distal part of the lower leg (Figs. 1 and 2). The examination was otherwise normal. Chest x-ray, urinalysis, and blood tests including a complete blood count, biochemistry, antinuclear antigen, anticardiolipin antibodies, complement, and immunoglobulins were normal or negative.
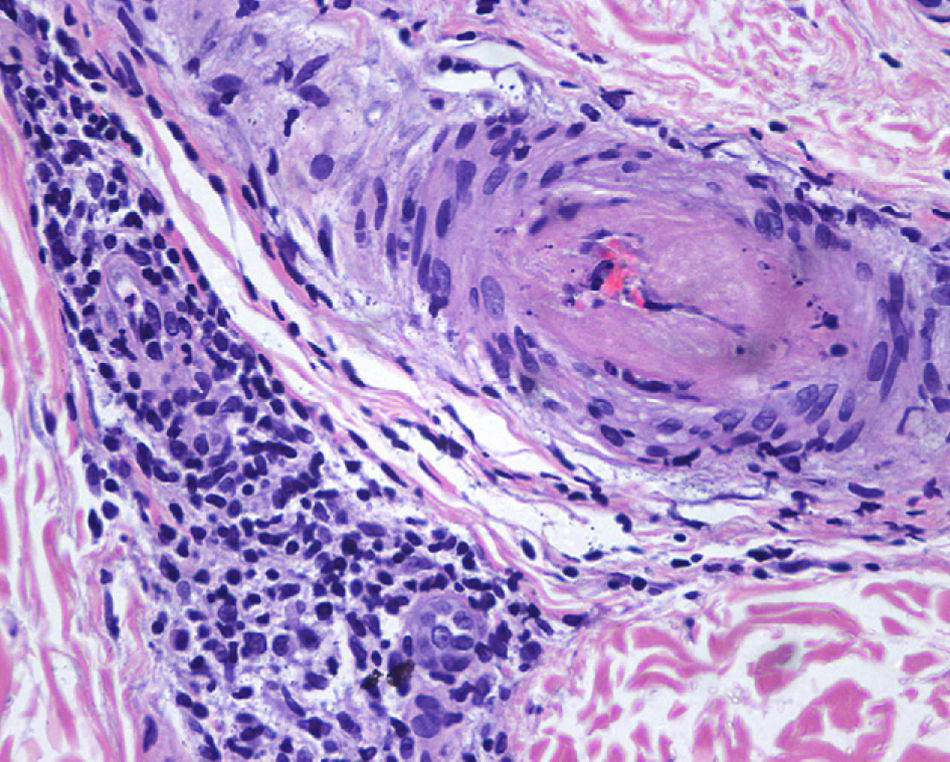
Skin biopsy of 1 of the bluish macules on the left foot revealed foci of thrombosis in a medium-sized arteriole with no signs of vasculitis (Fig. 3). The epidermis was normal. No cholesterol crystals were found.
Arteriography showed turbulent flow in the popliteal artery, a finding consistent with the presence of an aneurysm of the popliteal artery; the rest of the arteriography, including proximal and distal arteries, was normal.
Computed tomography (CT) confirmed the presence of a popliteal artery aneurysm 2cm in diameter with mural thrombus. It excluded other alterations, such as popliteal artery entrapment syndrome. Abdominal CT showed no abnormalities, and aortic aneurysm was ruled out.
The results of additional tests performed to determine the etiology and pathogenesis of the aneurysm were not consistent with a diagnosis of Marfan syndrome, leading us to consider that the aneurysm might be atheromatous in origin.
Popliteal-popliteal bypass was performed with inverted internal saphenous vein. The skin lesions resolved within a few days with no sequelae, and follow-up to 2 years after surgery was favorable.
In 1961, Feder et al2 described the cases of 6 patients who developed painful purple toes 3 to 8 weeks after starting treatment with oral coumarins. The term blue toe syndrome was coined 15 years later in an article describing 31 patients with angiographic evidence of proximal vascular emboli, usually originating in the femoral or popliteal arteries but also released from aortic aneurysms.3
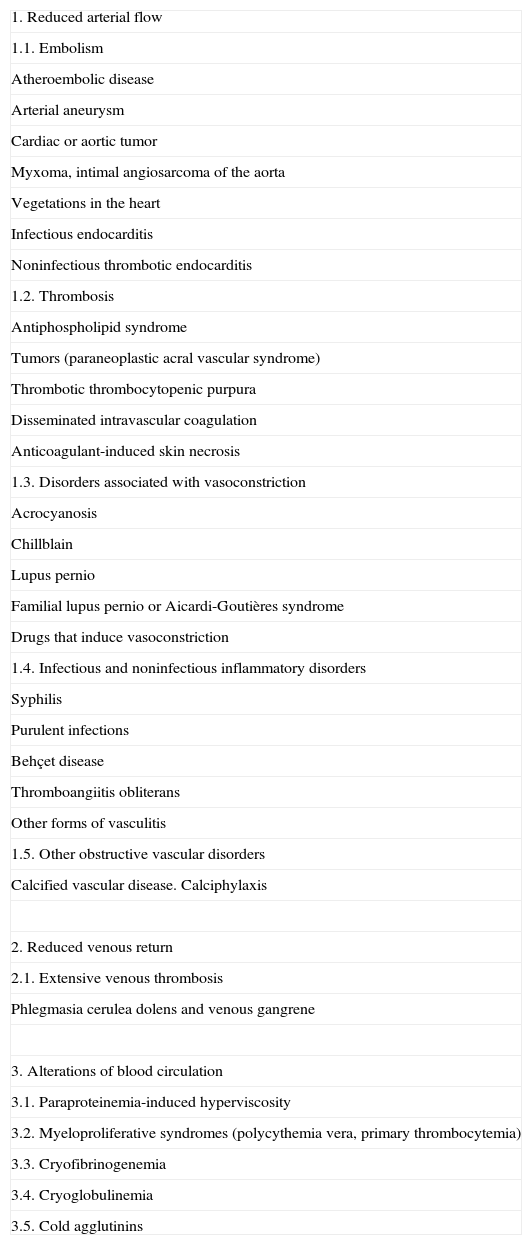
Since its initial description in 1961, numerous etiologies that can give rise to this sign have been reported (Table 1). While it has always been known as a syndrome, the term should more properly be called a sign because it refers to the description of a clinical condition that can be observed by a physician. Hence our use of “blue toe sign” in the title of the present article.
Etiology of the Blue Toe Sign.
| 1. Reduced arterial flow |
| 1.1. Embolism |
| Atheroembolic disease |
| Arterial aneurysm |
| Cardiac or aortic tumor |
| Myxoma, intimal angiosarcoma of the aorta |
| Vegetations in the heart |
| Infectious endocarditis |
| Noninfectious thrombotic endocarditis |
| 1.2. Thrombosis |
| Antiphospholipid syndrome |
| Tumors (paraneoplastic acral vascular syndrome) |
| Thrombotic thrombocytopenic purpura |
| Disseminated intravascular coagulation |
| Anticoagulant-induced skin necrosis |
| 1.3. Disorders associated with vasoconstriction |
| Acrocyanosis |
| Chillblain |
| Lupus pernio |
| Familial lupus pernio or Aicardi-Goutières syndrome |
| Drugs that induce vasoconstriction |
| 1.4. Infectious and noninfectious inflammatory disorders |
| Syphilis |
| Purulent infections |
| Behçet disease |
| Thromboangiitis obliterans |
| Other forms of vasculitis |
| 1.5. Other obstructive vascular disorders |
| Calcified vascular disease. Calciphylaxis |
| 2. Reduced venous return |
| 2.1. Extensive venous thrombosis |
| Phlegmasia cerulea dolens and venous gangrene |
| 3. Alterations of blood circulation |
| 3.1. Paraproteinemia-induced hyperviscosity |
| 3.2. Myeloproliferative syndromes (polycythemia vera, primary thrombocytemia) |
| 3.3. Cryofibrinogenemia |
| 3.4. Cryoglobulinemia |
| 3.5. Cold agglutinins |
Adapted from Hirschmann JV et al,.1
Our patient presented acute reduction of arterial perfusion due to the occlusion of arteriolar vessels by emboli arising from a mural thrombus in a popliteal artery aneurysm. Although relatively rare, popliteal artery aneurysm is the most common peripheral arterial aneurysm and it is associated with aneurysmal disease at other sites in up to 45% of patients.4,5 Imaging studies should therefore be performed to exclude the presence of other aneurysms.
The most feared complication of popliteal artery aneurysm is acute distal ischemia of the limb after a thrombotic event within the aneurysm. Such ischemia can affect the lower leg below the knee if the thrombus completely occludes the popliteal artery. However, if microemboli block distal arteries or arterioles, the condition will affect a more limited area of the limb, giving rise to blue toe syndrome and other changes.
As this clinical sign can have many causes and is not specific, the etiologic diagnosis of the disease causing the condition must be based on a detailed clinical history and directed additional tests.
Early diagnosis is essential as, depending on the cause of the blue toe sign, the patient's life, or at least limb, could be at risk.
We present a patient with blue toe syndrome or, as we propose, blue toe sign caused by embolism from a popliteal artery aneurysm, an etiology rarely reported for this syndrome.6,7 In this case, early diagnosis contributed to a good clinical outcome.
Please cite this article as: Martínez-Morán C, García-Donoso M C, Moreno A, Borbujo Jet al. Signo del dedo azul como manifestación inicial de aneurisma de la arteria poplítea. Actas Dermosifiliogr.2011;102:551-52.