Atypical lentiginous nevus (of the elderly) is a peculiar form of dysplastic nevus. Clinically, this condition can resemble malignant melanoma and histologically, it has a lentiginous pattern with variable degrees of atypia and an absence of dermal nests. These features may lead to an erroneous diagnosis of lentigo maligna melanoma or lentiginous melanoma.
Material and methodsWe reviewed 14 cases of atypical lentiginous nevus diagnosed at the dermatology department of Hospital General de Valencia in Valencia, Spain between December 2007 and March 2009. We studied the clinical and histopathologic features of the lesions after hematoxylin-eosin, Melan-A, and Ki-67 staining and compared our results to data reported in the literature.
ResultsFour (28%) of the 14 patients (7 men, 7 women) were under 50 years of age. Clinically, most of the lesions (8/14) resembled atypical nevi and they were all located on the back. Histologically, they all had irregular lentiginous epidermal hyperplasia, with a proliferation of individual melanocytes only in the basal layer of the epidermis and an absence of dermal nests. Focal upward migration of melanocytes into the epidermis was present in just 4 cases. All the lesions had cellular atypia, which was moderate in 85% of cases. The Ki-67 proliferation index was low (<5%) in all the lesions analyzed.
ConclusionsAtypical lentiginous nevi, which can be classified as atypical pigmented lesions with a lentiginous pattern, may clinically and histologically resemble melanoma. Our findings support earlier reports that both clinical and histologic findings may suggest a diagnosis of dysplastic nevus. All of the patients in our series are healthy and free of recurrence after 18 months or longer.
El nevus lentiginoso atípico (NLA) del anciano es una forma peculiar de nevus displásico, que clínicamente puede simular un melanoma maligno, y que histológicamente presenta un patrón lentiginoso con grados variables de atipia en ausencia de nidos dérmicos, que puede sugerir erróneamente el diagnóstico de lentigo melanoma o melanoma lentiginoso.
Material y métodosHemos recogido 14 casos de nevus melanocítico lentiginoso atípico diagnosticados entre diciembre de 2007 y marzo de 2009 en el Servicio de Dermatología del Hospital General de Valencia. Hemos estudiado sus características clínicas e histopatológicas tras la tinción de las piezas con hematoxilina-eosina, melan-A y Ki67 y las hemos comparado con los datos publicados en la literatura.
ResultadosEntre los datos clínicos, el 28% eran menores de 50 años, con una relación entre sexos de 1:1. La mayoría de las lesiones sugerían clínicamente un nevus atípico (8/14) y todas aparecieron en la espalda. Todos los casos presentaron hiperplasia epidérmica lentiginosa irregular, con proliferación de células melanocíticas individuales, limitadas a la membrana basal, en ausencia de nidos dérmicos; solo 4/14 tenían también ascenso epidérmico focal. Todos presentaron atipia citológica (en un 85% de los casos moderada). El índice de proliferación, valorado mediante la tinción con Ki67, fue bajo (<5%) en todos los casos estudiados.
ConclusiónLos NLA son lesiones que pueden simular clínica e histológicamente un melanoma, y que se encuentran en el grupo de las lesiones pigmentadas atípicas con patrón lentiginoso: tanto en nuestra serie como en las series previamente publicadas, los hallazgos histológicos y evolución clínica de estos pacientes orientan hacia el diagnóstico de nevus displásico. Actualmente todos los pacientes estudiados están sanos y sin recidivas después de un seguimiento mínimo de 18 meses.
Atypical lentiginous nevus, originally defined as lentiginous dysplastic nevus of the elderly, was first described in 1991 by Kossard et al.,1 who had observed clinically atypical pigmented lesions with histologic features conforming to the pathology of dysplastic melanocytic nevus with a lentiginous pattern. Because atypical lentiginous nevus manifests clinically as pigmented, asymmetric, multicolored lesions that appear in areas of chronic sun damage, this condition can be confused with melanoma, lentigo simplex, and atypical melanocytic nevus.2
Atypical lentiginous nevus is a peculiar form of dysplastic nevus that is difficult to diagnose. Clinically, the condition can resemble melanoma, and it is difficult to establish a differential diagnosis based on the histologic findings between dysplastic nevus and melanoma, in particular lentiginous melanoma and lentigo maligna.1,2 Given the similarities between atypical lentiginous nevus and lentiginous melanoma, some authors have suggested that these 2 conditions are the same entity, and it is possible that some case series of lentiginous melanoma have included cases of atypical lentiginous nevus.3–6 Other authors, however, regard atypical lentiginous nevus to be an independent entity of uncertain malignant potential.1,2,7
We reviewed 14 cases of atypical lentiginous nevus diagnosed in our department with the objective of describing the clinical and histopathologic features that can aid in the diagnosis of this entity.
Materials and MethodsThis was a retrospective analysis of the clinical and histologic data of 14 patients diagnosed with atypical lentiginous nevus in the dermatology department of the Hospital General Universitario in Valencia between December 2007 and March 2009 (Table 1). The cases were independently assessed by 2 dermopathologists (V.A. and A.M.), who agreed on the diagnosis of atypical lentiginous nevus in all cases. The clinical data analyzed were age, sex, site of the lesions, and clinical diagnosis. The presence or absence of certain histopathologic features and additional criteria were analyzed as follows: lentiginous epidermal hyperplasia (regular or irregular) with proliferation of single or nested melanocytes; dermal nests (mild, moderate, or abundant); solar elastosis (mild, moderate, or severe); fibrosis in the papillary dermis (concentric or with signs of regression); upward migration of melanocytes into the epidermis (focal or generalized); lymphohistiocytic inflammatory infiltrate (mild, moderate, or heavy); cellular atypia (mild, moderate, or severe), taking into account the relative sizes of melanocyte and keratinocyte nuclei (the M/K size ratio), which under normal conditions is <1:1. Finally, the presence or absence of adnexal involvement (eccrine, follicular, or of other types) was also assessed.
Epidemiological, Clinical and Histological Characteristics of 14 Patients with Atypical Lentiginous Nevi.
| Patient/Age, y/Sex | Site | Clinical Appearance | Irregular Epidermal Hyperplasia | Dermal Nests | Proliferation of Single Melanocytes | Solar Elastosis | Dermal Fibrosis | Upward Migration | Inflammatory Infiltrate | Cellular Atypia (M/K Size Ratio)a | Adnexal Involvement |
| 1/78/M | Back | Lentigo simplex | Yes, irregular patches of hyperpigmentation | No | Yes, mild | Yes, mild | Yes | No | No | Moderate (M=K) | No |
| 2/60/F | Back | Atypical nevus | Yes | No | Yes | No | Concentric | Yes | Moderate | Mild (M>K) | Yes, eccrine |
| 3/49/M | Back | Atypical nevus | Yes, irregular hyperpigmentation | No | Yes | Yes, mild | Concentric | Yes, focal | Moderate | Mild (M=K) | Yes, follicular |
| 4/62/F | Back | Atypical nevus | Yes | No | Yes | Yes, mild | No | No | No | Moderate (M=K) | Yes, eccrine |
| 5/36/F | Back | Atypical nevus | Yes | No | Yes | No | Yes | No | Yes, mild | Moderate (M=K) | No |
| 6/61/M | Back | Atypical nevus | Yes | No | Yes | Yes, moderate | No | Yes, focal | Yes, moderate | Moderate (M=K) | Yes, follicular |
| 7/47/F | Back | Melanocytic nevus | Yes | No | Yes | No | No | No | No | Moderate (M=K) | No |
| 8/71/F | Back | Melanocytic nevus | Yes, irregular hyperpigmentation | No | Yes | Yes, mild | Yes, signs of regression | No | Yes, moderate | Moderate (M=K) | No |
| 9/75/M | Back | Atypical nevus | Yes | No | Yes | No | Yes, signs of regression | Yes, focal | Yes, moderate | Moderate (M>K) | No |
| 10/26/F | Back | Melanocytic nevus | Yes | No | Yes | No | No | No | Yes, mild | Moderate (M=K) | No |
| 11/62/M | Back | Atypical nevus | Yes | No | Yes | No | Concentric | No | Yes, moderate | Moderate (M>K) | No |
| 12/55/M | Back | Melanoma | Yes | No | Yes | Yes, moderate | Concentric | No | Yes, mild | Moderate (M=K) | Yes, follicular |
| 13/62/F | Back | Atypical nevus | Yes | No | Yes | No | Concentric | No | Yes, mild | Moderate (M=K) | No |
| 14/55/M | Back | Atypical nevus | Yes | Yes, mild | Yes | No | Concentric | No | No | Moderate (M>K) | Yes, follicular |
M: male; F: female.
In all cases, the pigmented lesion was surgically excised with narrow margins (1-2mm). In cases in which the melanocytic nevus persisted clinically or histopathologically, the patients underwent a second intervention to ensure complete excision of the lesion. All patients were followed up for a minimum of 18 months.
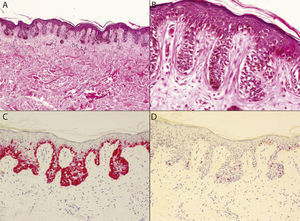
ResultsFour of the 14 patients (28%) were under 50 years of age and both sexes were affected equally (the ratio of men to women was 1:1) (Table 1). The diagnosis suggested by the clinical appearance of the lesions was atypical nevus in 57% of the cases (8/14), lentigo simplex in 7% of the cases (1/14), and melanoma in 7% of the cases (1/14) (Fig. 1). In all cases, the lesions were located on the back. All of the biopsy specimens were studied using hematoxylin-eosin, Melan-A, and the mitotic marker Ki-67. Histopathologic findings revealed that all of the lesions had irregular lentiginous epidermal hyperplasia. An irregular pigmentation pattern was seen in 3 lesions, 1 of which had achromic patches. Proliferation of single melanocytes confined to the basal layer of the epidermis was seen in all cases, and focal upward migration of melanocytes into the epidermis was observed in only 4 lesions (Fig. 2, A and B). Dermal nests, which were small and focal, were only present in 1 case. All of the lesions had cellular atypia, which was moderate in 12 of the 14 cases (85%). The M/K size ratio was 1:1 in 10 cases and between 1:1 and 2:1 in the remaining 4 cases. Adnexal invasion, present in 6 patients (42%), was follicular in 4 cases (28%) and eccrine in 2 cases (14%). Six of the 14 patients (42%) presented solar elastosis, mild in 4 cases and moderate in 2. Dermal fibrosis was present in 13 of the patients studied (93%) and was concentric in 6 cases (42%). Mild-to-moderate inflammatory infiltrate was present in 10 cases (71%). Incontinence of pigment was observed in all cases and melanin was present in the stratum corneum in 2 cases. Melan-A staining confirmed the predominance of proliferating melanocytes in the basal layer of the epidermis and weak, focal pagetoid invasion (Fig. 2C). The Ki-67 proliferation index was low (<5%) in all of the cases analyzed (Fig. 2D).
A, Irregular lentiginous epidermal hyperplasia with solitary melanocytes distributed asymmetrically at the dermal-epidermal junction and no dermal nests (hematoxylin-eosin, original magnification ×40). B, Proliferating cells exhibit foci of moderate cellular atypia. Focal pagetoid migration of melanotyes can be observed, with invasion of adnexal structures in some cases (hematoxylin-eosin, original magnification ×200). C, Melan-A immunohistochemical staining reveals the predominance of proliferating melanocytes in the basal layer of the epidermis, with focal pagetoid invasion (Melan-A, original magnification ×100). D, Absence of mitosis and low Ki-67 proliferation index (<5%) (Ki-67, original magnification×100).
Atypical lentiginous nevus is a lentiginous melanocytic proliferation with clinical features that often resemble those of melanoma. Its classification has been the subject of some debate and histopathologic findings do not always completely resolve clinical uncertainties as they can be indicative of both dysplastic nevus and melanoma.4,8–10
Clinically, atypical lentiginous nevus manifests as a pigmented lesion located in an area of chronic sun damage—primarily on the back or the proximal parts of the limbs—in individuals aged 50 to 70 years. Unlike lentigo maligna, however, atypical lentiginous nevi do not usually occur on the face or scalp. The lesions range in size from 0.3 to 1cm and are asymmetric and multicolored. This condition can be clinically confused with lentigo simplex or atypical melanocytic nevus, and the clinical picture is often suggestive of melanoma. Dermoscopy usually reveals an irregular reticular pattern of pigment distribution with poorly defined edges, often with various different patterns and colors, pigment spots, and hypochromic areas.2
Histologically, atypical lentiginous nevus is characterized by irregular lentiginous epidermal hyperplasia, the presence of nests in the rete ridges, predominance of isolated melanocytes in the basal layer of the epidermis, foci of moderate cellular atypia, and the absence of dermal nests. Focal pagetoid migration of melanocytes can be observed, with invasion of adnexal structures in some cases. A mild lymphohistiocytic inflammatory infiltrate is often observed in the upper dermis with concentric papillary fibrosis and pigmentary incontinence. Solar elastosis is usually absent or very mild and no mitosis is observed.
The histologic findings in an atypical lentiginous nevus may lead to a differential diagnosis with dysplastic nevus and other lentiginous melanocytic proliferations (Table 2). Unlike other forms of dysplastic nevus, tumor proliferation in atypical lentiginous nevus consists primarily of solitary melanocytes that do not form dermal nests. In fact, this absence of dermal nests is one finding that may suggest a diagnosis of lentigo maligna or lentiginous melanoma.3,4,6,11 Unlike other lentiginous proliferations such as solar lentigo, lentigo simplex, and nevus lentiginous, atypical lentiginous nevus presents—in addition to cellular atypia—irregular epidermal hyperplasia, single and nested melanocytes in the rete ridges, and irregularly distributed melanocytes in the suprapapillary epidermis that may converge focally.2,3 Atypical lentiginous nevus also presents other features suggestive of melanoma (lentiginous melanoma and lentigo maligna), including, in some cases, adnexal involvement and, occasionally, foci of pagetoid spread of melanocytes into the upper layers of the epidermis. Unlike lentigo maligna, however, atypical lentiginous nevus usually presents moderate cellular atypia with no spindle-shaped cells, no epidermal atrophy, and little or no solar elastosis.2,3
Differential Diagnosis of Lentiginous Melanocytic Proliferations.
| Lentiginous Junctional Nevus (Benign) | Solar Lentigo | Lentigo Maligna | Lentigo Simplex | Atypical Lentiginous Nevus (of the Elderly) | Lentiginous Melanoma (Nevoid Lentigo Maligna) | Small Cell (Nevoid) Melanoma | |
| Size | <0.5cm | 0.2-4cm or larger | 1cm or larger | 1-3mm | 0.3-1cm | 1cm or larger | 1cm or larger |
| Epidermal hyperplasia (elongated rete ridges) | Always, regular | Usually, regular | Rarely; epidermal atrophy is common | Occasionally, regular | Always, irregular | Always, irregular | Variable, irregular |
| Dermal nests | Never | Never | Never | Never | Rarely | Occasionally | Always |
| Lentiginous proliferation of melanocytes | Small nests in rete ridges | Rarely, without nests | Confluent junctional melanocytes without nests | Isolated junctional nests | Prevalence of isolated junctional melanocytes; occasional nests in rete ridges | Irregularly distributed nests and melanocytes with tendency to coalesce | Variable; nests or single cells |
| Solar elastosis | Occasionally | Always | Always | Occasionally | Rarely, mild-to-moderate | Rarely, mild-to-moderate | Rarely, mild-to-moderate |
| Dermal fibrosis | Occasionally, mild | Never | Occasionally | Never | Usually, prominent | Occasionally, focal | Usually, prominent |
| Upward migration | Never | Never | Always | Never | Rarely | Usually, focal | Always |
| Inflammatory infiltrate | Occasionally, mild | Occasionally, lichenoid | Occasionally, lichenoid | Never | Usually, mild-to-moderate | Usually, moderate | Usually, frequent regression |
| Cellular atypia | Never | Never | Moderate-to-severe; spindle-shaped and, rarely, epithelioid cells | Never | Focal; mild-to-moderate; epithelioid cells | Moderate, epithelioid cells | Moderate-to-severe; small, spindle-shaped, desmoplastic cells |
| Adnexal involvement | Never | Never | Usually | Never | Occasionally | Occasionally | Always |
| Mitosis | Never | Never | Occasionally, junctional | Never | Never | Rarely, junctional | Usually, dermal |
Although there is no consensus on the classification of atypical lentiginous melanocytic proliferations, several authors have asserted that lesions of this sort may progress to melanoma.2,3,6,12 Given the uncertain prognosis associated with atypical lentiginous melanocytic proliferations, the ability to recognize these entities is fundamental, especially when histology is based on a partial biopsy. When rare histologic features—such as superficial fibrosis, melanophages, lichenoid inflammatory infiltrate, regression, and pigmentary incontinence—are found in an apparently benign lentiginous melanocytic lesion, a diagnosis of melanoma should be considered and complete excision of the lesion is recommended.2,3,6,12
This descriptive study had certain limitations: the findings associated with atypical lentiginous nevus were not compared with findings from a similar group of patients with lentiginous melanoma. Controlled analytic studies of larger series are needed to definitively establish the characteristics and nosological position of atypical lentiginous nevus relative to other atypical melanocytic proliferations, in particular lentiginous melanoma and lentigo maligna.
Recent studies have assessed the usefulness of fluorescence in situ hybridization (FISH) as a tool for diagnosing melanocytic lesions with inconclusive histopathologic findings.13–16 In the specific case of lentiginous melanocytic proliferations, patients with lentiginous melanoma have been found to have chromosomal aberrations not present in a control group of patients with benign lentiginous nevi.17 Eventually, molecular analysis techniques may make it possible to develop an exhaustive classification of atypical melanocytic lesions. These techniques could be particularly useful in determining whether atypical lentiginous nevus and lentiginous melanoma are independent entities separate from lentigo maligna.
Our experience corroborates previously published data that show that most atypical lentiginous nevi consist of a lentiginous epidermal hyperplasia with proliferation of atypical melanocytes, occurring both singly and in nests, at the dermal-epidermal junction. Exceptionally, focal adnexal involvement may be present, and in such cases a diagnosis of lentigo maligna melanoma or lentiginous melanoma should be considered. The absence of cell apoptosis or mitosis, the low Ki-67 proliferation index (<5%), and the limited pagetoid invasion as revealed by the Melan-A marker are findings that favor a diagnosis of nonmalignant melanocytic proliferation (dysplastic nevus). All patients included in the study are currently healthy and showing no signs of recurrence following complete excision of the lesion and at least 18 months of follow-up.
ConclusionAtypical lentiginous nevi, which can be classified as atypical pigmented lesions with a lentiginous pattern, may clinically and histologically resemble melanoma. Our findings support earlier reports that both clinical and histologic findings indicate a diagnosis of dysplastic nevus. Knowledge of this peculiar form of atypical nevus can help doctors to avoid a misdiagnosis of melanoma.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
The authors thank Antonio Martínez for his invaluable collaboration on this study.
Please cite this article as: Agustí-Mejias A, et al. Nevus lentiginoso atípico. Estudio clínico-patológico de 14 casos. Actas Dermosifiliogr. 2012;103:394-400.